Contents
35th week of pregnancy (37 weeks)
At 35 weeks of pregnancy (37 weeks), the mother-to-be enters her ninth month of pregnancy. The baby is physiologically ready to be born, but to gain more strength and weight, it is good that he still remains in his mother’s womb, who in turn must take care of herself.
35 weeks pregnant: where is the baby?
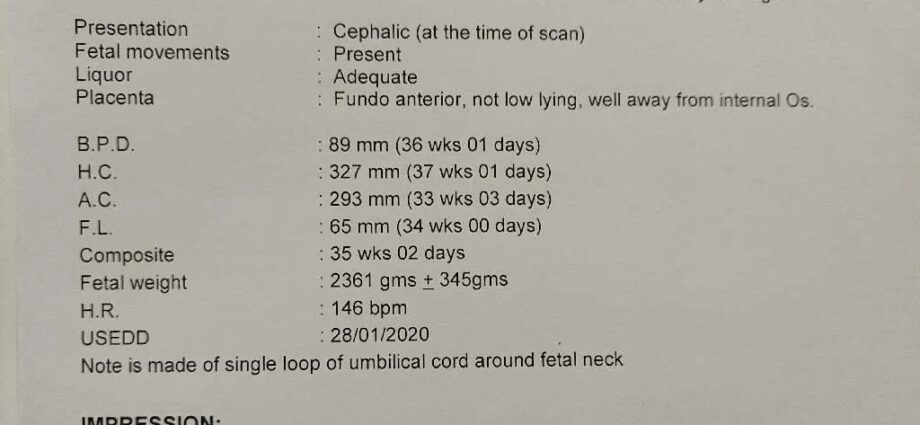
At the beginning of the 9th month of pregnancy, the baby measures on average 45 cm. Its weight is 2,4 kg. By birth, he will gain 30 to 40 g per day.
His head has reached, to within a few millimeters, its birth size, a cranial perimeter of about 9 cm. Its skull is made up of different bony plates connected by fibrous spaces: the fontanelles. As it is not completely ossified, the skull will be able to model itself during childbirth in order to facilitate the baby’s passage through the different straits of the mother’s pelvis.
The baby is held upside down, arms crossed, legs grouped together, unless he has remained in a seat, like 5% of babies. Even if it begins to be very cramped to move at ease, it continues to alternate between active phases and phases of sleep. His sleep is now composed of phases of restless sleep and phases of calm sleep.
He swallows 500-700 ml of amniotic fluid per day. He thus trains himself in the sucking reflex and is already beginning his awakening to the taste.
Where is the mother’s body at 35 weeks pregnant?
The uterus has grown a lot and continues to rise. By the ninth month, it measures about thirty centimeters and is located between the point of the breastbone and the navel. At the top, he presses on the diaphragm, sometimes interfering with breathing. At the bottom, it compresses the bladder, causing frequent urges to urinate. The stomach is not left out, which can lead to very unpleasant gastroesophageal reflux, especially at night. The whole digestive system is also slowed down under the effect of this pressure but also of pregnancy hormones. Constipation is therefore frequent.
Breasts continue to prepare for breastfeeding. They are tense, the network of veins more and more apparent. A few drops of colostrum can sometimes bead on the nipples, but some expectant mothers will not have any at all during their pregnancy. No worries: this does not bode well for the ability to breastfeed or not.
With the weight and increased blood volume, the legs are also strained. Venous insufficiency is common at the end of pregnancy, with heavy legs, a feeling of swelling or even the appearance of small varicose veins. To limit discomfort, it is recommended to elevate your legs at rest and to walk for about XNUMX minutes a day. Compression stockings can be prescribed by the doctor or midwife if necessary. Be careful, however: the sudden appearance of edema should lead to a consultation without delay, this may be a sign of preeclampsia.
Contractions and pains
The contractions multiply throughout the day: the belly hardens for about thirty seconds. These are Braxton Hicks contractions or reactive contractions (fatigue at the end of the day or following an effort). These contractions should remain irregular and painless.
In terms of pain, back pain is a classic at the end of pregnancy. With the weight of the uterus in the front, it is in fact the entire center of gravity of the body that is modified, and the lumbar muscles are highly stressed.
Under the influence of the hormonal secretions which increase with the approach of the childbirth, the body prepares itself little by little for the day J. With the volume of the belly and the joints which relax for the childbirth, pains can appear at the level of the pelvis. We speak of relaxation of the pubic symphysis (the joint at the front of the pelvic girdle), or pubalgia. These pains usually subside with rest.
What are the signs of childbirth?
When to go to the maternity ward? This is indeed the big question for the 9 month pregnant mother-to-be. Here are the signs to watch out for.
Regular and painful contractions
Labor contractions are regular, painful, and more and more intense. They can be felt in the stomach, lower abdomen, lower back, buttocks or perineum. At term, that is to say after 37 weeks, the expectant mother is generally advised to go to the maternity ward after regular contractions (every 5 minutes) for 2 hours for a first child, then 1 hour for a first child. The following. During this time, the mother-to-be can take a hot shower or bath to see if the contractions subside (except in the event of loss of fluid, in which case head to the maternity ward). If the contractions persist, it’s time to head to the maternity ward. During the admission examination, a vaginal examination will be carried out in order to assess the condition of the cervix and the height of the baby in the baby. The contractions will be evaluated by monitoring. These two gestures make it possible to know if the labor has really started or if it is about a false job.
Loss of water or liquid
Any loss of fluid in greater or lesser quantity requires going to the maternity ward without delay, because once the water bag is open, the risk of infection is real. Loss of water may precede contractions; it will then be the trigger for labor. If the loss of water occurs after the onset of contractions, it will accelerate them.
The loss of the mucous plug
The mucous plug is a collection of mucus that protects the cervix throughout pregnancy. A few days or weeks before the term, when the cervix begins to soften, the mother-to-be may notice the loss of white mucus, sometimes streaked with small streaks of blood. This is the famous mucous plug. This is a sign that the body is preparing, but it does not mean the start of labor. There is therefore no need to go to the maternity ward in the presence of this only loss of the mucous plug.
Apart from the signs of childbirth, other situations require going to the maternity ward without waiting at the end of the pregnancy:
blood loss: whether it is red or brown blood, all blood loss requires going to obstetric emergencies.
decrease in baby’s movements: it is advisable to consult, if only to be reassured, in the absence of fetal movements for 24 hours.
fever (temperature above 38 ° C): at this stage of pregnancy, any infection can have an impact on the baby, so it is important to find its origin and treat it quickly.
signs of preeclampsia: headache, sudden onset of edema, ringing in the ears, visual disturbances, nausea and vomiting, general malaise, pain in the upper part of the stomach or under the ribs on the right.
In case of doubt or concern, do not hesitate to contact the maternity ward. Her team is there to reassure and advise the mother, whatever the situation. The approach of childbirth is a unique moment, it is quite normal to need to be reassured.
Preparation for childbirth
Childbirth preparation courses continue in the maternity ward or in a midwife’s office. At home, it is advisable to regularly practice the exercises learned during the lessons: breathing, tilting movements of the pelvis, etc. If the expectant mother follows a preparation in sophrology, prenatal hypnosis, prenatal singing, prenatal yoga, she can also do some exercises at home.
From this week, it is possible to perform a daily massage of the perineum to soften it for childbirth. This regular perineal massage would limit the risk of tears and episiotomy during childbirth, different studies suggest. The only contraindication: a vaginal infection. To perform this massage, it is advisable to use an oil suitable for massaging the perineum. In practice, it is advisable to introduce the thumb at the entrance to the vagina, and to rotate the index and middle fingers on the skin. If in doubt, do not hesitate to seek advice from your midwife.
Maternity suitcase
While the baby can arrive overnight, the maternity suitcase needs to be packed. Maternity usually provides a list, but here’s a quick reminder of the essentials.
The delivery bag:
a comfortable t-shirt or a large shirt
a pair of socks
a water mist
something to snack on for dad
baby’s first outfit: bodysuit, cotton or wool bra (depending on the season), wool hat, pajamas, pair of socks, diapers (if not provided by the maternity ward), sleeping bag
the little extras: a nursing pillow, music, reading, the special homeopathy childbirth kit (Gelsemium against anxiety, Ignatia amara for cervical dilation, Arnica montana to recover from childbirth are some of the classics) , sweet almond oil to relax the perineum, essential oils for childbirth
The papers :
ID card
Vital card
mutual insurance certificate
family record book or early recognition
blood group card
test results: ultrasound report, anesthesia blood work, vaginal swab of streptococcus B
The baby’s keychain:
6 bodysuits (birth size or 1 month depending on the assumed weight) with crossed opening on the front
6 pajamas
3 wool or cotton bras (depending on the season)
two caps
socks
mittens
two sleeping bags
6 bibs or swaddles
newborn size diapers
3 bath towels
a special baby soap
a change product, washable or cotton wipes
a thermometer
an outfit for the outing, with combipilot in winter
Mom’s suitcase:
3 comfortable pajamas or nightgowns (possibly nursing)
5 comfortable outfits for the day, easy to open when breastfeeding
a vest
a pair of slippers
3 bath towels and a small bath mat
a toiletry bag (shower gel, shampoo, toothbrush, toothpaste, makeup)
about ten cotton panties, mesh panties or disposable briefs
a package of special maternity sanitary napkins (if not provided by the maternity ward). Favor non-plasticized materials (organic cotton for example)
a dirty laundry bag
the phone charger
if breastfeeding: 2 to 3 nursing bras, breast pads, lanolin
Things to remember at 37:XNUMX PM
The 7th and final prenatal consultation takes place this week or next. Like every month, the practitioner checks the tension, the uterine height, the weight and the cervix by a vaginal examination. He will also check the fetal presentation (the way the baby looks) by palpating the tummy. The usual biological examinations are prescribed: serology of toxoplasmosis in case of negativity, irregular agglutinins in case of rhesus negative, albumins. In addition to ensuring the good health of the baby and its mother, this consultation aims to establish a prognosis for childbirth.
In the event of presentation at headquarters, an external maneuver version is sometimes offered. It is generally performed around 37 WA, under ultrasound monitoring and control. With his hands, the obstetrician-gynecologist will exert pressure on the stomach in order to help the baby to tilt upside down. The success rate of the maneuver varies from 48 to 77% depending on different factors: more or less flexible uterus, multiparity (higher success rate compared to the mother whose first pregnancy is), baby’s position more or less lower, mum’s weight gain (movements are more efficient through the abdominal wall if the weight gain is reasonable), but also operator experience.
If the baby remains in breech, a vaginal birth or cesarean section will be considered depending on the size of the baby at the last ultrasound, the dimensions of the pelvis, and of course the mother’s wishes.
If the consultation with the anesthesiologist, the blood test and / or the vaginal sample for streptococcus B have not yet been done, we must not delay.
If the future dad wishes to take his paternity leave (11 consecutive days within 4 months after the birth), he must inform his employer at least one month before the start date of the leave, by registered letter with acknowledgment of receipt or letter delivered. in person against discharge. If he intends to take this leave directly after the 3 days of birth leave, this is the last time to send this letter.
Advice
His first year of life, the baby will be followed on a monthly basis by a general practitioner or a pediatrician. The shortage of pediatricians being real in some cities, it is advisable to find out about making an appointment and the deadlines before the birth of the baby. The PMI also offer consultations, very practical for weighing your baby during the first weeks.
If a birth plan has been written, it’s time to finalize it and share it with the birthing team. This document is above all a support for thinking about the birth and discussing with the medical team.
If the portage in a sling is considered, the ideal is to follow a babywearing workshop before the arrival of the baby. This method of carrying respects the physiology of the infant, provided that it is properly carried out. Hence the importance of learning the right actions from a specialist.
Pregnancy week by week: 33th week of pregnancy 34th week of pregnancy 36th week of pregnancy 37th week of pregnancy |