Contents
Questions about what makes some people more at risk than others from the severe course of COVID-19 and which factors contribute to how serious the disease develops are still open. Here are the first attempts to answer.
- What makes some people ill or without symptoms, and for others COVID-19 ends in hospitalization?
- Doctors and scientists have found several important links between our characteristics and the course of the coronavirus infection
- Age, gender, genes, and other diseases are critical to the course of COVID-19
- You can find more such stories on the TvoiLokony home page
Gender differences in immune responses have been noted. Studies have shown that males have higher plasma levels of cytokines and chemokines than females. On the other hand, in women there is a stronger stimulation of T lymphocytes, which in men additionally decreases with age. These findings suggest that male gender and older age are associated with an increased risk of severe disease and mortality.
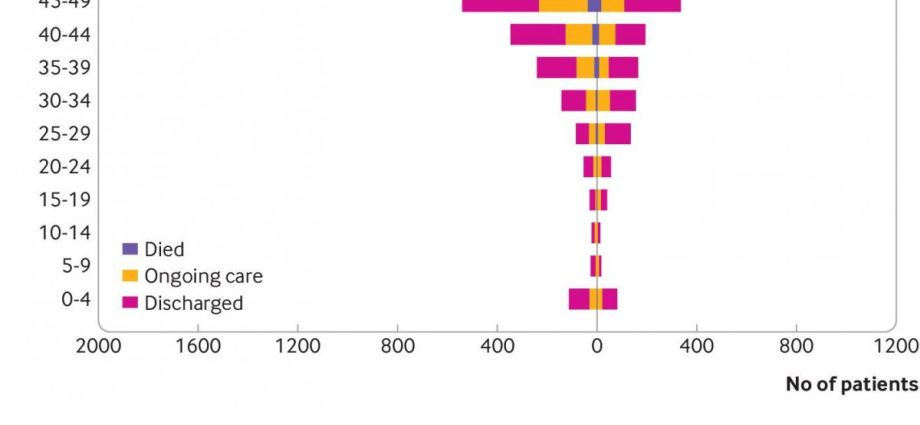
The ratio of infection to mortality is lowest among those aged 5-9 years, then increases with age, with the risk of death doubling approximately every eight years. Some scientists have hypothesized that the virus cannot penetrate into the cells of younger children, as it does to adult cells, because children produce fewer ACE2 receptors (angiotensin II converting enzyme receptor), which is where the virus attaches.
Other hypotheses include the possibility that children have a stronger and more effective initial immune response to the virus and that they may have some resistance to recent exposure to other coronaviruses.
However, more and more researchers believe that the difference between adults and children may be due to the condition of their blood vessels. The endothelium is usually much better in children than in adults. Additionally, older people are more likely to have comorbidities. In addition, with age, the body’s defenses weaken, not least because the thymus in which T lymphocytes mature, decreases.
The findings of scientists at the National Institutes of Health indicate that some people who develop severe COVID-19 carry a specific type of genetic mutation that causes interferon I deficiency or have autoantibodies directed against this interferon.
- See more: How Do Genes Influence COVID-19?
In July, Public Health England published that a BMI of 35 to 40 could increase the risk of dying from COVID-19 by 40%, while a BMI greater than 40 could increase that risk by 90%.
Abdominal obesity is associated with impaired ventilation of the base of the lungs, which results in decreased oxygen saturation in the blood. Moreover, in abdominal obesity, chronic inflammation is common, due to inappropriate secretion of adipokines and cytokines, such as tumor necrosis factor alpha and interferon, resulting in impaired immune responses and effects on lung and bronchial parenchyma.
People with type 1 and type 2 diabetes had a 3,5 and 2 times higher risk of inpatient death from COVID-19, respectively, compared to those without diabetes. A relationship was also identified between the glycosylated hemoglobin index (HbA1c) and mortality from SARS-CoV-2 infection. The risk was significantly higher in type 1 diabetics with HbA1c above 86 mmol / mol and in type 2 diabetes above 59 mmol / mol.
It is known that hyperglycemia weakens the host’s defenses, including the functions of granulocytes and macrophages. Additionally, there have been reports of direct destruction of pancreatic β cells by SARS-CoV-2, which may contribute to worsening of glycaemia and, in some cases, lead to diabetic ketoacidosis.
It has been shown that people with cancer were at a higher risk of severe COVID-19, longer hospitalization and a greater risk of death, which a study in Wuhan found was particularly high among people with blood cancer. Patients receiving invasive therapies such as chemo-, radio- and immunotherapy are also at greater risk. Comparing biochemical indices between cancer patients and non-cancer patients, it was found that pro-inflammatory cytokines, including TNF-α, IL-6 and IL-2R, were higher in cancer patients, as were the inflammatory biomarkers procalcitonin and CRP.
As for the immune cells, there was a marked decrease in CD4 + T cells and CD8 + T cells. Moreover, the results of blood clotting studies, such as the decrease in platelet count, prothrombin time, and post-activation partial thromboplastin time, were also markedly worsened in cancer patients.
All these indicators are helpful in assessing the severity of the disease and should be intensively monitored during COVID-19 treatment.
Chronic respiratory diseases such as asthma, COPD, cystic fibrosis, and idiopathic pulmonary fibrosis significantly increase the risk of severe disease caused by COVID-19.
Hypertension is by far the most common comorbid disease in COVID-19 patients. Hypertension has been shown to increase the risk of death from SARS-CoV-3,5 by a factor of 2. It was speculated that the high incidence of infections might be due to the use of ACE inhibitors, but this hypothesis was quickly refuted. Other diseases that can affect the severe course of COVID-19 include: heart failure, coronary artery disease, cardiomyopathies, and pulmonary hypertension.
A meta-analysis of studies confirmed that pregnant women with SARS-CoV-2 infection are at greater risk of being admitted to the intensive care unit and mechanical ventilation. Death is also more frequent than in non-pregnant women. This may be related to physiological changes in pregnancy, including increased heart rate and oxygen consumption, decreased lung capacity, and increased risk of thromboembolism. Pregnant women with COVID-19 are also at increased risk of preterm labor.
People with risk factors may be at greater risk of hospitalization or death from infection. These include many other diseases, such as conditions of reduced immunity (caused by HIV or taking immunosuppressive drugs), hematological disorders or chronic kidney diseases.
SARS-CoV-2 can act as a factor in accelerating the deterioration of existing conditions, so it is important that all at-risk people take all measures to protect themselves from infection, including avoiding large amounts of social contact, wearing a face mask, and frequent hand washing. It is also important to constantly monitor the underlying disease and continue taking medications as prescribed by your doctor, and not delay in obtaining help in cases of deterioration of health.
Author: Magda Mazurek / Medexpress
This may interest you:
- This symptom is 70 percent. infected with coronavirus
- The doctor explains: such a cough is a symptom of coronavirus infection
- Epilepsy, stroke, brain damage. They can appear after passing COVID-19
The content of the medTvoiLokony website is intended to improve, not replace, the contact between the Website User and their doctor. The website is intended for informational and educational purposes only. Before following the specialist knowledge, in particular medical advice, contained on our Website, you must consult a doctor. The Administrator does not bear any consequences resulting from the use of information contained on the Website. Do you need a medical consultation or an e-prescription? Go to halodoctor.pl, where you will get online help – quickly, safely and without leaving your home.Now you can use e-consultation also free of charge under the National Health Fund.