Contents
- Vagal discomfort: a sign of worry?
Vagal discomfort: a sign of worry?
What is vagal discomfort?
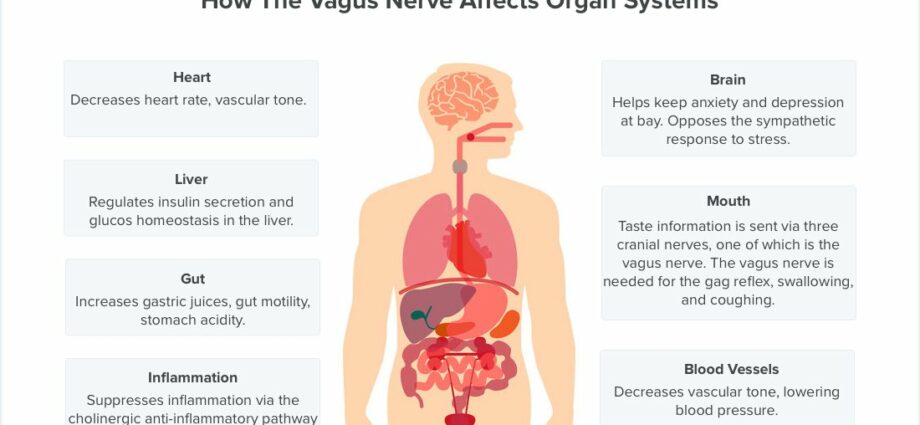
Vagal discomfort, also known as “syncope”, results in loss of consciousness for a few seconds. It is due to the sudden drop in blood pressure. The term “vagal” comes from the vagus nerve which crosses the body from the brain to the stomach, it is responsible for slowing down cardiac activity when it accelerates. In slow motion, the heart brings less blood to the arteries, the brain is then less oxygenated, which causes a spontaneous loss of consciousness, but usually very brief.
Vagal discomfort is the most common form of syncope or loss of consciousness. Clinically, the process and biological mechanisms involved in this type of discomfort are well known, but not exhaustive.
Discomfort is one of the common problems facing people today. cardiologists and general practitioners. Indeed, with an annual incidence (appearance of new cases of the pathology) of between 1,3 and 2,7 per 1 individuals, vagal discomfort should then be considered with attention.
Different forms of vagal discomfort exist:
- the mild form, resulting in a form of syncope;
- the more serious form, affecting patients with underlying pathologies, such as heart abnormalities, neurological diseases, etc.
Syncope, and therefore vagal discomfort, is defined as sudden and generally short-term loss of consciousness. The return to the “normal state” is spontaneous and rapid. It is also characterized by global cerebral hypoperfusion. Or by the decrease in vascularization in the brain.
What should be done in case of vagal discomfort?
Nausea, dizziness, pale face, blurred vision, sweating, dry mouth, hot flashes, hearing buzzing, general weakening … When a person has vagal discomfort, it is important to elevate their legs in order to oxygenate the brain to restore balance to the heart system.
- If the person is unconscious, they should be placed in the Lateral Safety Position (PLS). This first aid act is used to free the airways of the body.
- If the person has not quickly come to his senses, the emergency services must be alerted immediately.
When you feel that you are having this kind of discomfort, try lying down or squatting, if you are sitting it is better to stay there and not get up.
What are the warning signs of vagal discomfort?
Some clues can help recognize vagal discomfort:
- hot flashes;
- nausea ;
- extreme fatigue;
- blurred vision;
- sweats;
- pallor;
- diarrhea;
- successive yawns;
- hearing problems such as tinnitus.
Should we be worried about vagal discomfort?
In most cases the vagal discomfort is not serious, however the fall it causes is not without danger.
Vagal discomfort: a sign of worry? : understand everything in 2 min
The causes are various, linked to hypersensitivity of the vagal nerve or to other external factors:
- period of intense stress
- overwork
- sensitivity, anxiety
- emotional shock
- hot weather
- feeling of compartmentalization
- phobias (blood, crowd, etc.)
- after local anesthesia
- taking certain medications, such as isoproterenol, nitroglycerol or even clomipramine.
In other cases, the causes of vagal discomfort are not without seriousness. Neurobiological or cardiovascular disorders can occur.
In any case, a person prone to one or more vagal discomfort should consult a healthcare professional. A diagnosis and an evaluation of the clinical case will make it possible to specify the cause of the discomfort. The health professional will be particularly interested in the patient’s history, his lifestyle and his social context (family and professional situation, etc.).
What are the symptoms and treatment of vagal discomfort?
The biological mechanisms involved in vagal discomfort are still too little known. In addition, it has been shown that the brain is strongly involved.
Vagal discomfort is then a “reflex” activation of the cerebral cortex, the onset of which is rapid, inducing a decrease in the heart rate and a reduction in muscle tone.
The activation of these reflex mechanisms then provokes
- bradycardia, slow heart rate;
- vasodilation, an increase in the size of the blood vessels;
- hypotension, abnormally low blood pressure.
Most people with vagal discomfort report significant signs: feelings of imbalance when standing, dizziness, headaches, and “normalcy” after a few minutes.
In other cases, the discomfort may last longer. And in this context, the loss of consciousness, caused by cerebral hypoperfusion, then leads to convulsive movements or even epileptic seizures.
Signs may appear before the discomfort occurs, such as intense fatigue, muscle weakness, wet skin, visual disturbances or even tinnitus.
Diagnosis and treatment of vagal discomfort
The diagnosis of vagal discomfort is made beforehand by questioning the patient and through medical examinations. Questions are also to be asked in the context of this first phase of diagnosis, in particular if the loss of consciousness is really to be linked to a syncope, if the patient has an underlying heart disease or if there is clinical information on the individual. could possibly guide the diagnosis.
Vagal discomfort diagnostic tools allow early identification of these, for example recording systems to identify possible arrhythmias. After the first discomfort, an Electroencephalogram (ECG) is then performed.
As part of the management of vagal discomfort, short-term hospitalization is sometimes necessary.
The treatments associated with the vagal risk consist of limiting the recurrence of discomfort, and thus reducing the risk of mortality. Indeed, syncope can be additional risk factors for accidents at work, in the context of physical and / or sports practice or simply everyday accidents.
How to prevent vagal discomfort?
La a change. and patient education are part of the initial treatment for the disease. In fact, avoid “triggering” factors, such as places and times likely to trigger a situation of stress and risk of discomfort. But also the learning of the gestures to be implemented in the stopping of a syncopic episode.
Drug treatments are not necessarily prescribed in patients who have presented only one or two syncope. However, in the context of a greater frequency of discomfort, treatments are available. Among these are beta blockers, disopyramide, scopolamine, theophylline, and the like.
Finally, the doctor is held responsible for the prevention of driving in the context of the risk of syncope. Indeed, the syncopic risk can prove to be dangerous for automobile drivers, which can put the patient, himself, in danger but also others.
To prevent vagal discomfort, it’s best to eat a healthy, balanced diet, get enough sleep, and exercise regularly.
People at risk
The elderly as well as people with underlying pathologies are more concerned by the risk of syncope. Indeed, thehypertension, diabetes or aging interferes with the self-regulation of the cerebral vascularization. In this sense, the risk of syncope is greater.
The incidence and prevalence are all the more important with age (from 70 years). In France, nearly 1,2% of cases of vagal discomfort result in urgent care. 58% of patients with this type of discomfort are hospitalized.
Read also :
- Loss of consciousness