Contents
Thyroid surgery
A gland of a few centimeters located at the base of the neck, the thyroid secretes hormones involved in many functions of the body. The presence of nodules, a cancerous tumor, a compressive goiter or a disease sometimes requires an operation of the thyroid, that is to say its partial or total removal.
What is thyroid surgery?
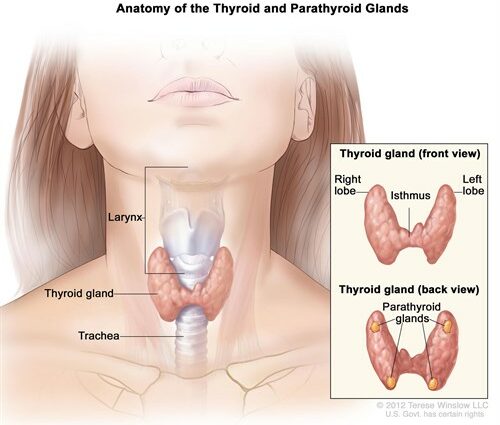
A butterfly-shaped gland located at the base of the neck, the thyroid regulates the rate of metabolism of many organs, via the T3 and T4 hormones it secretes. Too active or lazy, his activity can have repercussions on the whole organism. Nodules, goiter or cancer can also develop there, requiring in certain situations its removal, partial or total.
Thus, depending on the indication, different thyroid interventions exist:
- a simple resection of the nodule: only the nodule is removed, the rest of the thyroid is preserved;
- a lobectomy or lobo-isthmectomy: only one lobe of the thyroid is removed. It’s the most frequent case ;
- a “sub-total” thyroidectomy: the entire thyroid is removed, except for a small fragment on each side;
- a total thyroidectomy: the entire thyroid is removed with, in certain cases of thyroid cancer, lymph node dissection.
How is the thyroidectomy performed?
The thyroid operation is performed under general anesthesia. It lasts from 40 minutes to 1h30.
The patient is installed on the back, the head slightly extended. The surgeon makes a horizontal incision of a few centimeters (2 to 8 cm depending on the type of thyroidectomy) at the base of the neck. He then proceeds to resection of the thyroid, partial or total.
In the event of a simple nodule resection, a microscopic examination called an “extemporaneous examination” is performed during the operation in order to verify the exact nature of the removed nodule. Depending on the result, the surgeon may need to perform a more extensive ablation than that initially planned.
A small drain is left in place, then the incision is closed, most often with staples which give the best aesthetic results.
When to undergo thyroid surgery
Thyroid surgery is indicated in different thyroid diseases:
- a doubtful or cancerous thyroid nodule: tumor developing in the thyroid tissue, the thyroid nodule is common and most often benign, but in 5% of cases, it turns out to be cancerous. As recommended, a thyroid nodule less than 25 mm in diameter should be explored by fine needle aspiration. If the result is reassuring, regular ultrasound monitoring is sufficient. If the results show doubt, removal of the thyroid lobe is indicated;
- a benign nodule but whose large volume (more than 25 mm in diameter) makes it difficult to swallow, breathe and / or speak;
- compressive goiter, which ends up interfering with swallowing and breathing;
- thyroid cancer;
- multinodular goiter: multiple nodules develop in both thyroid lobes, within a thyroid that is itself enlarged (goiter). Thyroidectomy may be necessary if the nodules are large, if they are suspicious on fine needle aspiration, or if the size of the goiter makes it difficult to breathe or eat;
- certain so-called “hot” or “toxic” thyroid nodules, ie secreting a large amount of thyroid hormones causing hyperthyroidism;
- in Graves’ disease, an autoimmune disease causing hyperthyroidism. In the event of a relapse after a first drug treatment, thyroid surgery is sometimes offered.
After thyroid surgery
Operative suites
The postoperative effects are not very painful and easily calmed by analgesic treatment. The neck is swollen, however, and it can be difficult to turn your head for the first few days.
Feeding can be resumed the day after the operation. The first half of the staples is removed the next day, the other half before release. The scar is left in the open, without dressing, and it is not recommended to wet it for ten days. A blood test is taken 3 weeks after the operation to control the level of thyroid hormones as well as calcium.
A period of asthenia of 2 to 3 weeks is common after thyroid surgery. Depending on the extent of thyroid ablation, the possible replacement therapy and the nature of the professional activity, the sick leave may last up to 3 weeks.
The scar is located in the natural folds of the neck, so it is usually inconspicuous.
Management after thyroid surgery
In the event of total thyroid ablation, daily thyroid hormone replacement therapy is required for life. It is started during hospitalization and subsequently balanced by the attending physician or endocrinologist. This replacement therapy may also be necessary after partial ablation if the residual secretion is insufficient.
Risks and complications
Thyroidectomy is a fairly simple procedure, with rare complications: hematoma, hemorrhage, respiratory discomfort, infection.
After thyroid surgery, different disorders can appear. They are generally transient:
- discomfort when swallowing;
- dysphonia (modification of the pathway) due to the lesion of a recurrent nerve during the operation and which may require speech therapy;
- a disturbance in the regulation of calcium which can cause tingling and cramping, due to the involvement of one or more parathyroid glands (glands involved in the regulation of calcium) during the procedure. Calcium and vitamin D supplementation (necessary to fix calcium) is sometimes necessary.