Contents
- Thyroid cancer – types
- Thyroid cancer – symptoms
- Thyroid cancer – what tests should be performed?
- Characteristics of thyroid neoplasms
- Treatment of thyroid tumors
- Chemotherapy and radiotherapy in the treatment of thyroid cancer
- Complications related to the treatment of thyroid cancer
- The causes of thyroid cancer
- The incidence of thyroid cancer
- The prognosis for thyroid cancer
- Thyroid cancer and inheritance
- Thyroid cancer – an interesting fact
In line with its mission, the Editorial Board of MedTvoiLokony makes every effort to provide reliable medical content supported by the latest scientific knowledge. The additional flag “Checked Content” indicates that the article has been reviewed by or written directly by a physician. This two-step verification: a medical journalist and a doctor allows us to provide the highest quality content in line with current medical knowledge.
Our commitment in this area has been appreciated, among others, by by the Association of Journalists for Health, which awarded the Editorial Board of MedTvoiLokony with the honorary title of the Great Educator.
In Poland, nearly 2,5 thousand people develop thyroid cancer every year. people. The disease affects women four times more often than men. Although it mostly occurs in people in their 40s, it can also occur in people younger than 30 (around 20% of cases). How do you recognize the disease and what are the most common types of thyroid cancer?
Thyroid cancer – types
Thyroid neoplasms arise from cells of the follicular epithelium or C cells. Specialists distinguish:
- papillary cancer (papillary carcinoma),
- follicular cancer (carcinoma folliculare),
- anaplastic cancer (carcinoma anaplasticum),
- medullary cancer (medullary carcinoma).
Rarely do lymphomas and sarcomas or metastatic foci associated with breast, kidney or lung cancer develop in the tissues of the thyroid gland.
It is worth checking the condition of the thyroid gland regularly by performing preventive examinations. Remember about diagnostics. order your thyroid test package now.
Read also: Hashimoto’s disease – the Chernobyl effect?
Thyroid cancer – symptoms
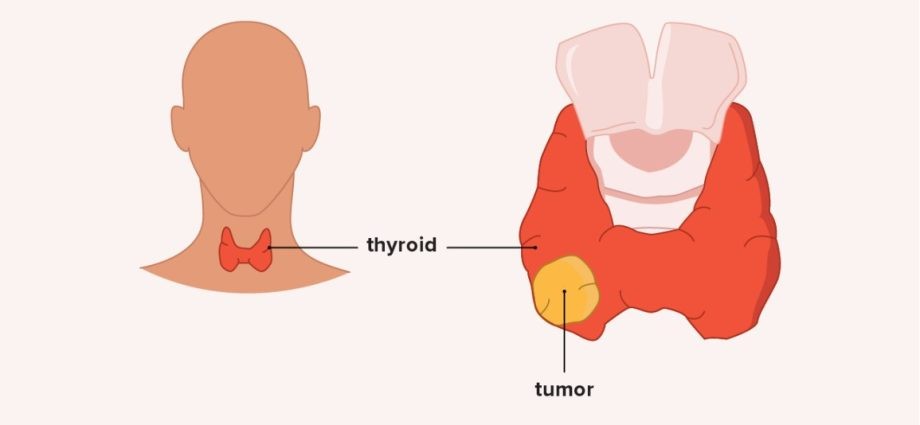
The earliest symptom of thyroid cancer is a lump that you can feel by examining the thyroid with your fingers. In papillary carcinomas, the first sign of a developing tumor may be an enlargement of the lymph node in the neck, despite the fact that the cancer itself grows in the thyroid gland and does not cause any symptoms. The developing neoplasm may affect part or all of the thyroid lobe. As a rule, the tumor has a hard and uneven structure and is not easy to move during examination.
In more advanced thyroid tumors, shortness of breath and wheezing may occur as a result of the movement and narrowing of the trachea. It also happens that the only symptom of an ongoing neoplastic process is hoarseness. It occurs when the cancer has attacked the retrograde laryngeal nerve, which is a branch of the vagus nerve.
Moreover, in the course of thyroid cancer, there are single or multiple thyroid tumors that grow rapidly. Sometimes the patient has difficulty swallowing or symptoms characteristic of Horner’s syndrome appear. a narrowing of the eyelid gap, narrowing of one pupil of the eye or brightening of the iris in one eye.
The causes of thyroid cancer are often genetically determined. These tumors also develop after irradiation of the neck area. It should be added here that a thyroid neoplasm in an early stage of development usually does not give any symptoms. The aforementioned symptoms, such as a tumor or hoarseness, are sporadic in the case of differentiated cancers and concern only the advanced stage of thyroid cancer.
Thyroid cancer – what tests should be performed?
The basic examination is an ultrasound of the thyroid gland. If it shows irregular areas of reduced echogenicity or the presence of microcalcifications, tumor development may be suspected.
Scintigraphy is another study. If the so-called cold nodules echoed on ultrasound should be further investigated to ensure that thyroid cancer is not developing. It should be added that the presence of warm and hot nodules does not exclude thyroid cancer.
People suspected of having thyroid cancer are also subjected to a fine needle biopsy (BAC) and blood serum levels of thyroglobulin and calcitonin (a hormone released by the C cells of the thyroid gland). Chest X-ray is also necessary to exclude or confirm the presence of lung metastases. Sometimes an X-ray of the abdominal cavity is also performed. There are also computer tomography or magnetic resonance examinations of the neck area.
In the case of fine-needle biopsy, the results prepared by the pathologist include a description of the characteristics of the tumor cells, as well as a code classifying the lesion into one of six groups:
- non-diagnostic biopsy – sometimes the collected material cannot be classified into any of the groups, and this is due to several factors, such as the issue of the examiner’s experience, improper storage of the material, method error and others, which may to some extent distort the result; in this case, the biopsy is usually repeated;
- benign lesion (e.g. hyperplastic nodule, colloidal nodule, nodular goiter, subacute thyroiditis) – such a result does not give rise to oncological concern;
- suspicion of a follicular tumor – this happens in the case of larger nodules that fall into this category; in such cases surgery is usually recommended, while if the nodules are smaller, a decision is often made for close surveillance using ultrasound;
- vesicular lesion unspecified – in this case, doctors recommend observation and a repeated biopsy after a few or several months; in this category, the degree of malignancy risk does not exceed 5%;
- suspicion of malignancy – in this case, surgery is usually required, sometimes preceded by another biopsy;
- malignant neoplasm – this result confirms the diagnosis and at the same time necessitates treatment.
Read also: It does not hurt, but the whole body suffers. Unusual symptoms that should worry you
Characteristics of thyroid neoplasms
Papillary cancer is the most common thyroid cancer. It usually progresses slowly, but it happens that the disease accelerates over time and is dynamic. In the first stage, the cancer is asymptomatic, but the disease spreads through the lymphatic vessels and may affect the lymph nodes in the neck, as well as those around the sternum, collarbones and nipples. This type of cancer shows a hormonal dependence on TSH.
Thyrotropin (TSH) is a hormone that is produced in the anterior pituitary gland. It works by stimulating the thyroid gland to produce and release the hormones thyroxine (T4) and triiodothyronine (T3). It remains in a negative feedback loop with circulating thyroid hormones, which means that high concentrations of thyroid hormones inhibit the synthesis and secretion of TSH, and low concentrations of T3 and T4 stimulate the production of TSH. Other hormones and drugs also influence the secretion of TSH.
The ultrasound of such a thyroid gland often shows microcalcifications. However, it is necessary to recognize that they are not caused by Hashimoto’s goiter. In Hashimoto’s disease, the altered cohesion most often affects the entire thyroid gland, but the diagnosis requires a fine-needle biopsy.
Papillary cancer accounts for 50-60 percent. of all thyroid cancers, and affects between 10 and 60 years of age. This type of cancer responds well to radioiodine treatment.
- Also read: Thyroid – the devil in the human body
Follicular cancer of the thyroid gland it occurs at different ages, also in very young people. It is composed of cancerous follicular cells and is hormonally active. It happens that in the course of this cancer the thyroid gland develops. The ultrasound image shows numerous calcifications. The cancer spreads through blood vessels and attacks the lungs and bones, which significantly worsens the prognosis of patients. This type of cancer accounts for 20-30 percent. all thyroid cancers and is more common in women over 40.
Anaplastic thyroid cancer is an extremely malignant form of thyroid cancer. It develops very quickly. It compresses and moves the trachea, making the patient feel very short of breath and suffer from hoarseness. It spreads through the body both through the lymphatic and blood vessels. The prognosis is poor because the average survival time of patients, despite the removal of the thyroid gland, is only half a year. This cancer most often affects the elderly and accounts for about 5-10 percent. all thyroid cancers. Radioiodine treatment is not used in therapy because the tumor is not susceptible to it. This is because cancerous cells do not absorb iodine.
Medullary thyroid cancer It is derived from the C cells of the thyroid gland, i.e. cells that are the source of calcitonin, a hormone that affects the calcium-phosphate balance in the entire body. Excessive secretion of calcitonin by the cancerous tumor tissue causes a compensatory increase in parathyroid hormone (PTH) synthesis by the parathyroid glands. As a rule, the calcium-phosphate balance is therefore maintained.
This type of thyroid cancer runs in families (15% of cases). Characteristically, it often occurs together with cancer of the adrenal medulla. It spreads to distant organs through the lymphatic vessels. This cancer also causes symptoms uncharacteristic for thyroid diseases in the form of paroxysmal diarrhea and arterial hypertension. Besides, it usually attacks both lobes of the thyroid gland. Not all forms of medullary thyroid cancer have an unfavorable prognosis. Some characters develop slowly and offer a chance for a long life. The disease develops most often in people over 45, but with a family burden, it may appear before the age of 35.
Treatment of thyroid tumors
The therapy always depends on the type of cancer and its stage.
Surgical treatment Its task is to remove nodules from the thyroid gland. Sometimes, during an operation, the doctor decides to remove not only the nodule, but also one or both of the thyroid lobes. The lymph nodes in the neck are also assessed during the procedure. If they are attacked by cancer cells, they must be removed.
If the therapeutic regimen provides for such an action, the patient will proceed approximately 4-6 weeks after the operation radioiodine therapy. It is given to destroy any leftover thyroid tissue. Iodine does not damage other tissues, not even those that are adjacent to the tissues of the thyroid gland.
After such treatment, the patient must remain in the hospital because iodine is active. Even the patient’s faeces and urine must be disposed of with special care. After administration of radioactive iodine, the patient should not contact other people, especially pregnant women, so as not to harm them.
The next stage of treatment is administration of thyroid hormones. Typically, such therapy is commenced about 1-2 weeks after the radioactive therapy. This procedure cannot be abandoned because thyroid hormones are needed for the proper functioning of the body. Medicines should be taken for the rest of your life. This is called substitution treatment.
In the case of the treatment of thyroid cancer, you can also talk about the so-called suppressive treatment. The idea is that some people with papillary and follicular cancer who have a good chance of relapse are given thyroid hormones in tablet form to stop any surviving cancer cells from growing.
In some cases, thyroid cancer is also used external irradiation of the neck and upper chest area. In rare forms of thyroid cancer, which include thyroid lymphomas, chemotherapy is the treatment of choice.
Every patient who is struggling with thyroid cancer must report to an oncologist or endocrinologist every six months. During the follow-up visits, the level of thyroid hormones in the blood is measured. Chest X-rays are also performed periodically.
Also get to know side effects of the administration of radioactive iodine
Chemotherapy and radiotherapy in the treatment of thyroid cancer
As for chemotherapy in the treatment of thyroid cancer, there are no scientifically documented indications so far. When it comes to radiotherapy, it plays a role in the treatment of thyroid cancer, but only in some cases. Radiotherapy has been used successfully in the treatment of incompletely resected differentiated cancer (assuming that radioactive iodine treatment and reoperation are not possible), incompletely resected medullary carcinoma and anaplastic thyroid carcinoma.
Among the complications resulting from the treatment of thyroid cancer, the most frequent is the paralysis of the recurrent laryngeal nervewhich is responsible for moving the vocal cords or, more simply, speech. This is due to the specific location of these nerves (they run directly behind the thyroid gland, sometimes tightly adjacent to the gland) and the difficulty in locating them, which causes my doctor to damage them during the surgery.
The doctor will inform the patient about possible complications during the visit qualifying for the surgery. You can find a specialist in your area on the website clinics.pl.
In extreme cases, it may lead to the loss of the ability to speak, loss of mobility of the strings and severe breathlessness. However, it should be noted that such situations are very rare. Another possible complication is hypoparathyroidism (hypocalcemia).
- Signs that the thyroid is sick. Don’t underestimate these symptoms!
The causes of thyroid cancer
One of the most studied factors in increasing the risk of developing thyroid cancer is the amount of iodine in the diet. Its deficiency contributes to more frequent occurrence of follicular thyroid cancer. In turn, too much iodine increases the incidence of papillary cancer.
The appropriate level of iodine will help provide the Kelp 630 mg dietary supplement. The preparation contributes to the proper functioning of the thyroid gland, maintaining proper energy metabolism and supporting the nervous system.
Another factor is the issue of inheritance, and it mainly concerns medullary carcinoma (therefore it is worthwhile for family members diagnosed with medullary thyroid cancer to perform genetic screening tests). What’s more, as much as 25% of all cases of thyroid cancer are accepted, it develops due to the presence of a genetically determined predisposition to the disease.
It is a mutation of the RET gene, with frequent occurrence of multi-neoplastic syndromes, e.g. MEN2A syndrome (including phaeochromocytoma, medullary thyroid cancer, parathyroid hyperplasia) or MEN2B syndrome (pheochromocytoma, medullary thyroid cancer, multiple neuromas).
Other factors that increase the risk of developing thyroid cancer include:
- exposure of the neck area to ionizing radiation (e.g. having had radiation therapy many years ago);
- extreme iodine intake;
- a familial history of multiple endocrine adenomatosis (FAP);
- female gender and age (<20 or> 50);
- syndromes: Pendred, Cowden, Gardner and familial adenomatous polyposis;
- RET protogen point mutation (medullary thyroid carcinoma).
The incidence of thyroid cancer
It should be noted that the most common cancer of the endocrine system (or endocrine or endocrine system) is thyroid cancer. In Poland, there are approximately 2500 new cases of thyroid cancer each year. Interestingly, women suffer from thyroid cancer 3 to 5 times more often than men (thyroid cancer is the number one cancer in women aged 15 to 29 and the second most common cancer after breast cancer in women aged 30 to 39). XNUMX years).
Some studies suggest that estrogen is a growth factor for both benign and malignant thyroid cells, further suggesting that gender plays a large role in the incidence of thyroid tumors and thyroid cancer, although more research is still needed to confirm this claim.
Most often, thyroid cancer appears around 40–50 years of age. age. About 2% of thyroid cancer cases occur in children and adolescents. Worldwide, the incidence of thyroid cancer is believed to have doubled since the 70s, but this is likely due to periodic testing and increased awareness.
The prognosis for thyroid cancer
As for the prognosis for thyroid cancer, they are unfavorable in poorly differentiated or undifferentiated varieties. The anaplastic form of thyroid cancer is very aggressive and grows rapidly, making recovery extremely difficult. However, it should be noted here that this variety is extremely rare.
In turn, in differentiated cases, as much as 90% of the cured patients were reported. In the case of medullary cancer, the level is slightly lower, reaching 70%. The key here is the early detection of the disease, so that the patient can be completely cured.
- It attacks women over 40. Obesity is the main risk factor
Thyroid cancer and inheritance
When it comes to the inheritance of thyroid cancer, in papillary thyroid cancer and follicular thyroid cancer, they are caused by the accumulation of inherited genetic changes as a result of exposure to unfavorable environmental factors. It should be added that specific genetic changes that predispose to the development of the above-mentioned types of thyroid neoplasms are still unknown. It is assumed that this is due to low penetration lesions which, when exposed to environmental factors, can initiate the process of carcinogenesis.
In turn, the situation is different in the case of medullary thyroid cancer (MTC), in which it is estimated that about 25 to 30% of cases are hereditary neoplasms, which are associated with the presence of mutations in the RET gene. Mutations in the RET gene are inherited autosomal dominantly and are usually punctual. They often lead to ligand-independent activation of the receptor, which promotes uncontrolled cell division and the neoplastic process.
For people with diagnosed medullary thyroid cancer, molecular tests of the RET gene are recommended. This is due to problems in differentiating sporadic and hereditary MTC. It is very important to find the genetic mutations that are responsible for the hereditary form of thyroid cancer as it is crucial for further medical follow-up and prognosis. Detection of the mutation also entails performing the same tests on the rest of the patient’s family. It should be added that if mutation carriers are detected, they are under medical care.
Being a carrier of the mutation is associated with frequent prophylactic examinations, which makes it possible to detect thyroid cancer at an early stage and, consequently, to apply a more effective treatment. In the case of determining a greater predisposition to developing thyroid cancer, they have genetic test kits including the multiplex CHEK2, CHEK 2 del5395 genes. The product of this pedestrian is one of the tumor suppressors, preventing uncontrolled division or too rapid growth of cells. Therefore, mutations that damage the CHEK2 gene favor the formation of tumors.
It should be mentioned here that there was an increased risk of developing CHEK2 mutation carriers: prostate cancer, breast cancer, papillary thyroid cancer, kidney cancer and colorectal cancer.
Thyroid cancer – an interesting fact
The disaster at the Chernobyl nuclear power plant in 1986 resulted in the release of a large amount of radioactive iodine into the atmosphere, which was the reason for a later and significant increase in the incidence of thyroid cancer among people living within a radius of several hundred kilometers from the explosion site.
We encourage you to listen to the latest episode of the RESET podcast. This time we devote it to the diet. Do you have to stick to it 100% to stay healthy and feel good? Do you really have to start every day with breakfast? What is it like with sipping meals and eating fruit? Listen:
For a long time you have not been able to find the cause of your ailments or are you still looking for it? Do you want to tell us your story or draw attention to a common health problem? Write to the address [email protected] #Together we can do more