Contents
Thrombophilie
Thrombophilia can be defined as an inherited or acquired defect that predisposes to the onset of thrombosis (blood clots). It constitutes a risk factor for partial or total obstruction of certain blood vessels.
Thrombophilia, what is it?
Definition of thrombophilia
Thrombophilia is a medical term that groups together several abnormalities that predispose to the formation of blood clots. These are abnormalities of hemostasis, that is to say abnormalities affecting the mechanisms contributing to stop bleeding in the event of a breach in a blood vessel.
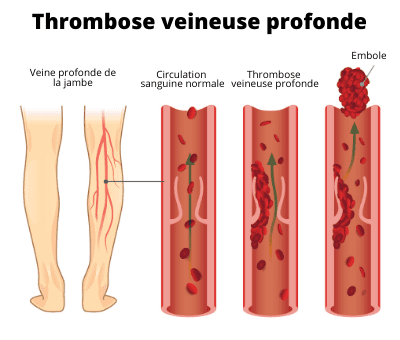
In other words, a person with thrombophilia has a bleeding disorder that promotes the formation of blood clots. A clot, blood clot, or thrombus is a small, slimy clump of blood cells. The development of blood clots can be the cause of serious complications because they can cause blockage of some blood vessels. The organs are no longer properly supplied and can no longer fulfill their roles.
Causes of thrombophilia
Thrombophilia can be congenital or acquired, that is, present from birth or occurring during life.
Congenital thrombophilia are most often hereditary (transmitted by parents). The main causes of congenital trombrophilia are:
- deficiencies in antithrombin, protein C or protein S, which are factors that inhibit coagulation;
- the factor V Leiden mutation resulting in resistance to protein C;
- the G 20210 A mutation on the prothrombin gene which is a coagulation protein;
- excess factor VIII involved in blood coagulation;
- hyperhomocysteinemia, which is high levels of homocysteine (a specific amino acid) in the blood.
Acquired thrombophilias are generally due to an anti-phospholipid syndrome. It is an autoimmune disease, that is, a disease caused by a dysfunction of the immune system. This produces abnormal antibodies (defense molecules of the body) which will attack essential constituents of the body. In the case of anti-phospholipid syndrome, these antibodies are directed against phospholipids (main constituents of the membranes of the body’s cells) or to elements linked to phospholipids.
Diagnosis of thrombophilia
Thrombophilia is diagnosed by a thrombophilia workup. This aims to look for congenital or acquired factors of thrombophilia. It consists in particular of:
- to assess the activity of coagulation inhibitor proteins;
- look for genetic mutations;
- test for anti-phospholipid syndrome antibodies.
Symptoms of thrombophillias
Formation of blood clots
Thrombophilia refers in a way to a state of predisposition to the occurrence of thrombosis (blood clots).
Risk of complications
A major risk of thrombophilia is the occurrence of venous thromboembolic disease. This brings together deep vein thrombosis (or deep phlebitis) and its immediate complication: pulmonary embolism. This corresponds to the obstruction of one or more arteries supplying the lungs. It causes damage to the affected lung and it can no longer provide oxygen to the body. Urgent care is essential because it is life-threatening.
Treatments for thrombophilia
The management of thrombophilia consists of preventing the risk of complications. It may in particular be based on:
- prescribing anticoagulants such as unfractionated heparins and low molecular weight heparins;
- elastic venous compression, in particular by wearing compression stockings or socks;
- the use of thrombolytics, medicines to dissolve blood clots.
Prevent thrombophilia
There are no preventive measures for thrombophilia. On the other hand, it is possible to prevent the risks of complications thanks to the preventive treatments mentioned above (anticoagulants, elastic venous compression, thrombolytics).