Contents
Plantar fasciitis
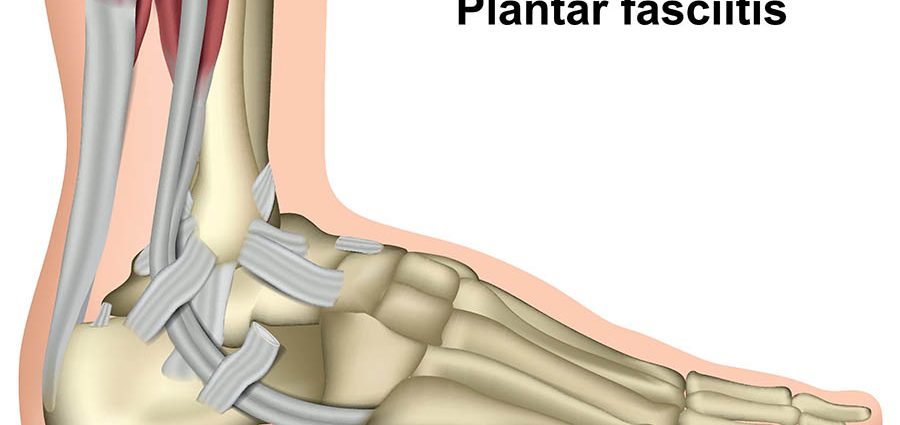
Fascia is pain resulting from trauma to the thick fibrous membrane called plantar aponeurosis: located under the foot, it extends from the heel to the base of the toes. Fascia more frequently affects athletes and the elderly. In 95% of cases, it can be treated without resorting to surgery.
What is aponeurosis?
Definition of fasciitis
Fascia is pain resulting from trauma to the thick fibrous membrane called plantar aponeurosis: located under the foot, it extends from the heel to the base of the toes. Thanks to its rigidity, the plantar fascia plays a supporting role for the foot. It absorbs shocks when resting on the ground and then when the foot unwinds. On the other hand, this lack of elasticity makes it not very resistant to repeated or unusual stresses.
Fascia mainly presents as an acute or chronic elongation of the plantar fascia and more rarely its tear. It should not be confused with plantar fasciitis which results from inflammation of the plantar fascia.
Types of fasciitis
Three types of fasciitis can be distinguished:
- Fascia related to the involvement of the back of the plantar fascia, causing pain under the heel bone;
- Fascia related to the involvement of the body of the plantar fascia, causing pain under the foot;
- The rupture of the plantar aponeurosis, which can occur suddenly following a violent effort (starting, pushing, receiving a jump) on a healthy or weakened plantar aponeurosis.
Causes of fascia
The most common cause of fasciitis is a shortening or retraction of the calf muscles, causing excessive mechanical stress on the plantar fascia.
Diagnosis of fascia
The attending physician can make the first diagnosis of fasciitis when examining the foot. It is confirmed when the pain is triggered by a strong pressure of the thumb under the heel at the back of the foot, when it is in hyperextension. The pain can also be on the inner edge of the foot.
The x-ray, which is not compulsory, may reveal the presence of a calcaneal spine or Lenoir’s spine, a calcified outgrowth under the heel bone. If contrary to the commonly accepted idea, it is not responsible for the pain, it testifies on the other hand to the chronic overwork of the region of the insertion of the plantar aponeurosis.
Other tests, such as magnetic resonance imaging (MRI), may be necessary if rupture of the plantar fascia is suspected.
People affected by fascia
Fascia represents approximately 11 to 15% of the reasons for consultation for foot pain. Athletes and the elderly are the first to be affected.
Factors favoring fascia
Many risk factors are responsible for fasciitis. Among the most common are:
- Mechanical imbalances of the foot such as hollow or flat feet;
- Thin calf muscles;
- An Achilles tendon, connecting the calf muscles to the heel bone, rigid;
- Wearing shoes that do not have good support, such as flip-flops, or high heels;
- Sudden weight gain, for example during pregnancy, or being overweight;
- A sudden increase in the number of steps walked or run;
- Poor posture of the feet in runners or regular dancers;
- Excessive weight on the foot due to prolonged and recurring standing.
Symptoms of fascia
Sensation of “nails in the heel”
Patients describe pain at the base of the heel, especially when getting up in the morning, when standing up. Described as a “nail in the heel” sensation, they usually subside after five to ten minutes only to return later in the day. Some patients may experience pain on the side of the foot when walking.
Intermittent pain
The pain can get worse at times. Symptoms worsen especially when walking, during prolonged standing or after periods of rest.
Acute heel pain
Sharp heel pain, sometimes accompanied by a slight local swelling, may indicate a tear.
Treatments for fascia
First, it is about putting your feet to rest and taking care of them:
- Take shorter steps;
- Reduce activities, especially those that cause pain;
- Avoid walking barefoot;
- Make massages;
- Apply ice to the sore spot, ten minutes every hour;
- Stretch the feet with a towel;
- Roll a ball under the soles of the feet without creating pain;
- Place a handkerchief on the floor and try to grab it with your toes.
- At the same time, treatments for fasciitis can consist of:
- Use adhesive straps or bandages supporting the arch of the foot;
- Use cushioning heels slipped into the shoes;
- Perform calf stretching exercises that can be associated with splints having the same effect to be worn at night;
- Wear foot orthotics which can ease fascia tension and symptoms.
Nonsteroidal anti-inflammatory drugs can provide inconstant and transient pain relief. Extracorporeal shock waves are frequently prescribed, but results vary. Infiltrations (steroids) are usually effective provided that the responsible physical activities are reduced over the long term.
In the event of a major rupture, immobilization in plaster for a period of 3 to 4 weeks is proposed.
If these measures are ineffective, surgery may be necessary to partially relieve the pressure on the fascia and remove the heel spines when they appear to be contributing to the pain.
Prevent fascia
In order to prevent plantar fasciitis or avoid recurrence, some tips are good to follow:
- Stop activities that increase pain;
- Recover between the different physical activities practiced;
- Stretch and get the right equipment for new activities;
- Maintain your line;
- Start walking or running again gradually;
- Do flexibility exercises after activities;
- Replace sports shoes regularly and make sure to adapt their quality according to the activity practiced.