Contents
Hyponatremia: causes, people at risk and treatments
Hyponatremia occurs when the body contains too little sodium for the amount of fluids it contains. Common causes include use of diuretics, diarrhea, heart failure, and SIADH. Clinical manifestations are primarily neurological, following osmotic transfer of water into brain cells, particularly in acute hyponatremia, and include headache, confusion, and stupor. Seizures and coma can occur. The management depends on the symptoms and clinical signs, in particular the evaluation of the extracellular volume, and the underlying pathologies. Treatment is based on reducing fluid intake, increasing fluid outflow, supplementing sodium deficiency, and treating the underlying disorder.
What is hyponatremia?
Hyponatremia is an electrolyte disorder characterized by excess body water relative to total body sodium. We speak of hyponatremia when the sodium level is below 136 mmol / l. Most hyponatremias are greater than 125 mmol / L and are asymptomatic. Only severe hyponatremia, that is to say less than 125 mmol / l, or symptomatic, constitutes a diagnostic and therapeutic emergency.
The incidence of hyponatremia is:
- about 1,5 cases per 100 patients per day in the hospital;
- 10 to 25% in geriatric service;
- 4 to 5% in patients admitted to emergency departments, but this frequency can rise to 30% in patients with cirrhosis;
- nearly 4% in patients with tumor disease or hypothyroidism;
- 6 times greater in elderly patients on antidepressant treatment, such as selective serotonin reuptake inhibitors (SSRIs);
- more than 50% in hospitalized patients with AIDS.
What are the causes of hyponatremia?
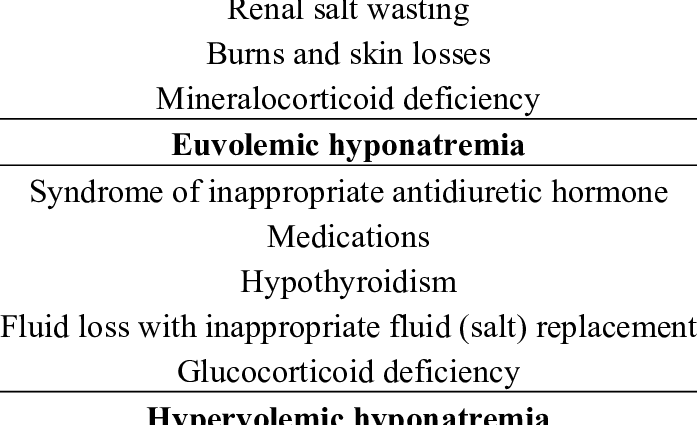
Hyponatremia can result from:
- sodium loss greater than water loss, with decreased body fluid volume (or extracellular volume);
- water retention with loss of sodium, accompanied by a conserved extracellular volume;
- water retention greater than sodium retention, resulting in an increase in extracellular volume.
In all cases, the sodium is diluted. Prolonged vomiting or severe diarrhea can lead to sodium loss. When liquid losses are compensated only with water, the sodium is diluted.
The loss of water and sodium is most often of renal origin, when the reabsorption capacities of the renal tubule are reduced, following the administration of thiazide diuretics. These drugs increase the excretion of sodium, which increases the excretion of water. These are generally well tolerated but can cause hyponatremia in people prone to low sodium, especially the elderly. Digestive or cutaneous losses are rarer.
Fluid retention is the result of an inappropriate increase in the secretion of antidiuretic hormone (ADH), also called vasopressin. In this case, we speak of SIADH or syndrome of inappropriate ADH secretion. Vasopressin helps regulate the amount of water present in the body by controlling the amount of water excreted by the kidneys. Excessive release of vasopressin results in decreased excretion of water by the kidneys, which leads to greater water retention in the body and dilutes sodium. The secretion of vasopressin by the pituitary gland can be stimulated by:
- pain ;
- the stress ;
- physical activity ;
- hypoglycemia;
- certain disorders of the heart, thyroid, kidneys or adrenals.
SIADH may be due to taking drugs or substances that stimulate the secretion of vasopressin or stimulate its action in the kidneys such as:
- chlorpropamide: drug that lowers blood sugar;
- carbamazepine: anticonvulsant;
- vincristine: drug used in chemotherapy;
- clofibrate: a drug that lowers cholesterol levels;
- antipsychotics and antidepressants;
- aspirin, ibuprofen;
- ecstasy (3,4-methylenedioxy-methamphetamine [MDMA]);
- vasopressin (synthetic antidiuretic hormone) and oxytocin used to induce labor during childbirth.
SIADH can also result from excessive consumption of fluids beyond the capacity of renal regulation or in cases of:
- potomanie ;
- polydipsie;
- Addison’s disease;
- hypothyroidism.
Finally, it may be the result of a decrease in circulating volume due to:
- heart failure;
- kidney failure;
- cirrhosis;
- nephrotic syndrome.
Sodium retention is the consequence of an increase in aldosterone secretion, following a decrease in circulating volume.
What are the symptoms of hyponatremia?
Most patients with natremia, i.e. a sodium concentration greater than 125 mmol / l, are asymptomatic. Between 125 and 130 mmol / l, the symptoms are mainly gastrointestinal: nausea and vomiting.
The brain is particularly sensitive to changes in the level of sodium in the blood. Also, for values below 120 mmol / l, neuropsychiatric symptoms appear such as:
- headaches ;
- lethargy;
- a confused state;
- stupor;
- muscle contractions and convulsions;
- epileptic seizures;
- a coma.
They are the consequence of cerebral edema, causing dysfunction, and the onset of which depends on the severity and speed of onset of hyponatremia.
Symptoms are likely to be more severe in older people with chronic conditions.
How to treat hyponatremia?
Hyponatremia can be life threatening. The degree, duration and symptoms of hyponatremia are used to determine how quickly it will be necessary to correct the blood serum. Symptomatic hyponatremia requires hospitalization in all cases.
In the absence of symptoms, hyponatremia is usually chronic and immediate correction is not always essential. However, hospitalization is recommended if the serum sodium level is less than 125 mmol / l. For asymptomatic hyponatremia or greater than 125 mmol / l, management may remain ambulatory. The doctor then assesses whether or not it is necessary to correct the hyponatremia and ensures that it does not worsen. Correcting the cause of hyponatremia is usually enough to normalize it. Indeed, stopping the offending drug, improving the treatment of heart failure or cirrhosis, or even the treatment of hypothyroidism are most often sufficient.
When correction of hyponatremia is indicated, it depends on the extracellular volume. If he’s :
- normal: restriction of water intake, below one liter per day, is recommended, especially in the case of SIADH, and treatment directed against the cause (hypothyroidism, adrenal insufficiency, taking diuretics) is implemented;
- increased: diuretics or a vasopressin antagonist, such as desmopressin, associated with a restriction of water intake, then constitute the main treatment, especially in cases of heart failure or cirrhosis;
- decreased, following digestive or renal losses: increased sodium intake associated with rehydration is indicated.
Some people, especially those with SIADH, require long-term treatment for hyponatremia. Fluid restriction alone is often not sufficient to prevent recurrence of hyponatremia. Sodium chloride tablets can be used in people with mild to moderate chronic hyponatremia.
Severe hyponatremia is an emergency. Treatment is to gradually increase the sodium level in the blood using intravenous fluids and sometimes a diuretic. Selective vasopressin receptor inhibitors, such as conivaptan or tolvaptan, are sometimes needed.