Contents
Hyperparathyroidie
Hyperparathyroidism is an endocrine disease caused by disruption of the parathyroid glands and causing an abnormal increase in parathyroid hormone. This hormone regulates the levels of calcium and phosphorus in the blood plasma, with consequences on the bones, kidneys or intestines. Hyperparathyroidism may be due to external causes or to abnormalities of the parathyroid glands. In the latter case, the treatment of choice lies in the removal of the defective parathyroid gland (s).
Hyperparathyroidism, what is it?
Definition of hyperparathyroidism
Hyperparathyroidism is an endocrine disease caused by disruption of the parathyroid glands and causing an abnormal increase in the secreted hormone parathyroid hormone (PTH). Four in number, the parathyroids are located at the base of the neck, contiguous to the back of the thyroid. The secreted parathyroid hormone regulates the levels of calcium and phosphorus in the blood plasma, with consequences on the bones, kidneys or intestines.
Types d’hyperparathyroïdies
Hyperparathyroidism can be:
- Primary, when due to an abnormality of the parathyroid glands. The production of calcium by the parathyroids becomes too important: we speak of hypercalcemia;
- Secondary, when the cause is external to the glands. Hyperparathyroidism then corresponds to an overproduction of parathyroid hormone in compensation for pathologies leading to hypocalcemia;
- Tertiary, when, as a result of secondary hyperparathyroidism, the glands develop autonomic function.
Causes of hyperparathyroidism
Primary hyperparathyroidism is caused by:
- In 80% of cases to a benign tumor of one of the parathyroid glands;
- In 10 to 15% of cases, there is hyperplasia – an increase in the number of cells and therefore in the volume – of several of the glands, often all four;
- In 3 to 4% of cases with parathyroid cancer.
Secondary hyperparathyroidism is linked to an external cause:
- Kidney failure;
- Osteomalacia or bone decalcification induced by a defect in the mineralization of the protein framework of the skeleton;
- Malabsorption of nutrients or reduced calcium intake due to pathologies: celiac disease (chronic bowel disease), cystic fibrosis, Crohn’s disease…;
- Rickets;
- Tubulopathy or kidney disease that affects the renal tubule.
Diagnosis of hyperparathyroidism
The diagnosis of hyperparathyroidism is based on measuring the level of parathyroid hormone in relation to serum calcium (level of calcium in the blood). Secondary hyperparathyroidism is defined by a compensatory increase in parathyroid hormone associated with low (or low normal) serum calcium. Primary hyperparathyroidism is revealed by an elevated parathyroid hormone level associated with hypercalcemia.
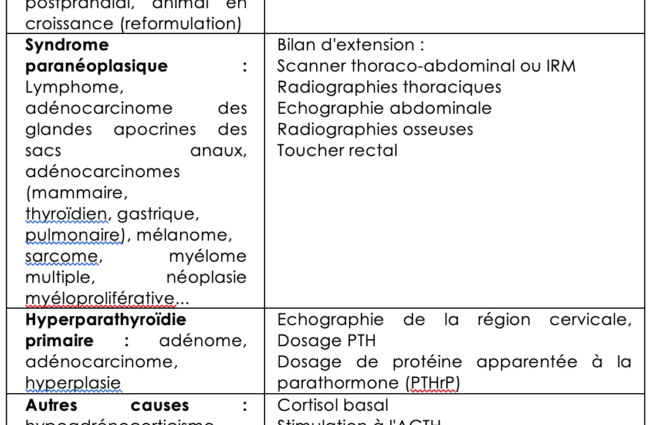
After ruling out a cause of secondary hyperparathyroidism, a primary hyperparathyroidism assessment is then performed via:
- A biological assessment of fasting plasma: measurement of the level of calcium, phosphate, alkaline phosphatase, urea, creatinine, vitamin D-25 (25-OH-vitamin D), parathyroid hormone;
- Bone densimetry;
- 24 hour urinalysis: calcium, creatinine, creatinine clearance, stone count;
- Abdominal imaging.
It is then a matter of locating the failing parathyroid (s) by:
- A parathyroid scan;
- An ultrasound;
- A CT scan or magnetic resonance imaging.
People affected by hyperparathyroidism
Hyperparathyroidism affects 25 in 100 people. Twice as common in women as in men, it occurs after 000 years in half of the cases.
Factors promoting hyperparathyroidism
Certain factors promote hyperparathyroidism:
- Postmenopausal osteoporosis;
- Certain drugs: bisphosphonates (indicated in the treatment of osteoporosis and certain cases of bone metastases), antiepileptic drugs, furosemide (diuretic), phosphorus…;
- Genetic factors.
Symptoms of hyperparathyroidism
Recurrent kidney stones
Symptoms of primary hyperparathyroidism include recurrent kidney stones due to hypercalcemia.
Loss of bone density
Primary hyperparathyroidism also leads to a progressive loss of bone density which can lead to pathological fractures or musculoskeletal disorders.
Bone pain
Secondary hyperparathyroidism contributes to renal osteodystrophy – a common complication of kidney failure causing joint pain.
Other symptoms
- Abdominal pain ;
- Tired ;
- Severe thirst;
- Nausea;
- Anxiety;
- Neurocognitive impairment;
- Depression.
Other symptoms of secondary hyperparathyroidism
- Chronic pruritus (skin condition);
- Atherosclerosis – accumulation of fatty substances in the arteries – accelerated.
Treatments for hyperparathyroidism
The hypercalcemia induced by primary hyperparathyroidism is difficult to control and is associated with significant mortality. The most effective treatments would be hydration, analogues of somatostatin (a protein hormone that inhibits growth hormone) and bisphosphonates (inhibitors of bone resorption by blocking the activity of osteoclasts).
But the treatment of choice for primary hyperparathyroidism remains parathyroidectomy, or the removal of the defective parathyroid gland (s). It is recommended when the plasma calcium level is 0,25 mmol / L above the upper standard in patients.
The different types of parathyroidectomies performed are as follows:
- Targeted parathyroidectomy when the adenoma is well localized;
- Bilateral cervical exploration: when the adenoma could not be located during medical imaging, the entire cervical region is then explored by the surgeon in order to identify and remove the pathological gland (s);
- Subtotal parathyroidectomy is indicated when all the glands increase the production of parathyroid hormone. This is called parathyroid hyperplasia. This situation is encountered in secondary and tertiary hyperparathyroidism and sometimes in primary hyperparathyroidism with multiple hyperplastic glands. The glands are then removed at 7 / 8ths, the remaining 1 / 8th is left in place or reimplanted.
- Total parathyroidectomy is a complete removal of the parathyroids and is only performed in the case of recurrent secondary hyperparathyroidism.
Prevent hyperparathyroidism
There are no specific measures capable of preventing the onset of hyperparathyroidism. But certain precautions can prevent the symptoms from worsening:
- Avoid drugs known to be responsible for hypercalcemia (calcium and vitamin D) and thiazide diuretics;
- Avoid risk factors for osteoporosis;
- Maintain physical activity.