Contents
Genital prolapse
A genital prolapse refers to the abnormal descent of one or more organs located in the pelvic cavity. This phenomenon mainly concerns women after 45 years and mainly affects the bladder, uterus, or rectum. Prolapse results from weakening or stretching of muscles and / or ligaments that support these organs. About 11 in 100 women prolapse in their lifetime. The choice of treatment depends on the age, the severity of the disorder and the possible complications. Prevention is based on reduction of risk factors.
Description of genital prolapse
The organs contained in the pelvis (or pelvic cavity) are held in their place by muscles, ligaments and fibers. And the pelvic floor, or perineum, supports them from below. Sometimes the muscles and ligaments weaken, stretch and / or the pelvic floor, relaxes, causing the more or less pronounced sliding of part or all of one of these organs (rectum, bladder, uterus) downwards. We then speak of prolapse.
Types of genital prolapse
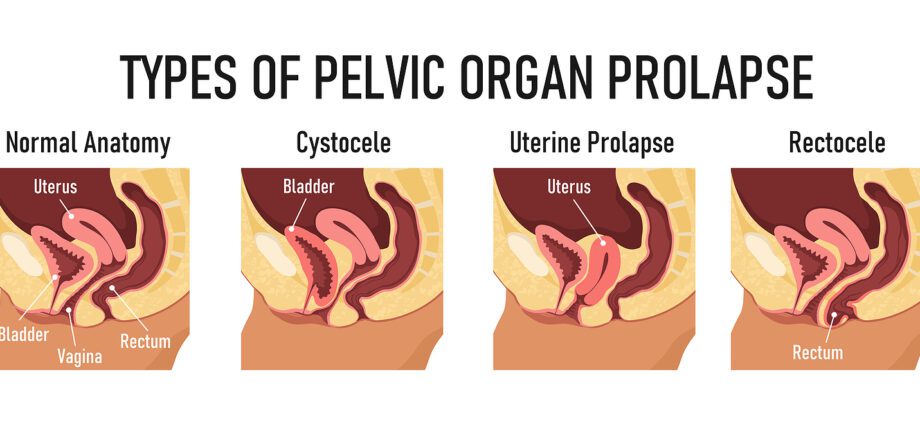
There are three types of prolapse:
- Le cystocèle or bladder prolapse: This is the most common prolapse which represents 4 out of 5 cases (ie 80% of cases). It is characterized by the fall of the bladder into the vagina.
- Hysterocele or prolapse of the uterus: This is the descent of the uterus into the vagina caused by the sagging of the vaginal walls
- Le rectocele or prolapse of the rectum: It is the descent of the rectum into the vagina. A complete rectal prolapse is the total descent of the rectum into the anal canal.
Genital prolapse: population at risk and risk factors
Populations at risk
Prolapse most commonly occurs in women between the ages of 45 and 85 after menopause due to loss of elasticity of muscles and fibers that support the organs.
Risk factors for genital prolapse
- Childbirth numerous and / or difficult
- Age
- Menopause
- Overweight /Obesity
- antecedents surgery in the pelvis area
- Professions or physical exercises involving a great strain on the pelvis (carrying or pulling heavy loads, etc.)
- Hereditary factor (family history)
- Constipation chronic
- In some athletes, the excessive development of the abdominal muscles
Symptoms of genital prolapse
Prolapse manifests itself mainly by feeling of heaviness in the pelvic cavity, discomfort sometimes accompanied by pain.
Prolapse can also be manifested by the presence of a soft ball in the vulva, especially when standing or during exertion.
In the event of a cystocele, it is common for a woman to have urinary disorders such as difficulty urinating, frequent or urgent urination (urination), cystitis (inflammation of the bladder)
In the event of rectocele, the evacuation of the stools can prove to be difficult, the affected subject sometimes goes so far as to use his fingers. In certain cases, the descent of the rectum generates on the contrary a anal incontinence (involuntary loss of stool).
Sexual disorders can also manifest as a sensation of gaping vulva, decreased sexual sensations, pain or discomfort during penetration.
Diagnosis of genital prolapse
First, the doctor asks the patient some questions about the discomfort felt and her antecedents (circumstances of childbirth, family history). Then it proceeds to a vaginal touch in order to estimate the descent of one or more organs. He may ask the patient to push while coughing in order to better perceive the prolapse. He examines the woman while lying down, but also standing or even squatting to better estimate the extent of the prolapse.
Additional examinations can be performed: urinary checkup, ultrasound or MRI of the pelvic cavity and kidneys to identify possible kidney damage.
If the prolapse involves the rectum, a straight copy (= exploration of the rectum) and a anorectal manometry (= measurement of the force of the sphincter) will be considered.
Treatments for genital prolapse
Several factors must be taken into account before adopting the appropriate treatment: age of the affected person, menopause, severity of the disorder, associated complications, history, etc.
In certain cases where the prolapse is not very important, the therapeutic abstention can be advised by the doctor. He may also suggest the use of pessaries which is the only medical, non-surgical treatment for prolapse. This involves inserting a device, often in the form of a ring, into the vagina, which keeps the organs that tend to descend.
Perineal rehabilitation helps to consolidate muscles pelvic cavity, but rather has a preventive or useful effect in early prolapse.
If there is an obvious risk factor such as obesity, it needs to be treated. A good hydration and a good diet (high fiber diet) are recommended. The hormone replacement therapy help fight the loss of tissue elasticity in postmenopausal women.
In the most severe cases of prolapse, the doctor offers surgery to fix the organ suffering from the prolapse. There are several techniques depending on the type and degree of prolapse.
How to prevent genital prolapse?
La reduction of risk factors helps prevent prolapse :
- systematic perineal rehabilitation after pregnancy,
- pay attention to the perineum during childbirth,
- treatment of obesity and constipation,
- hormone replacement therapy during menopause,
- protection of the muscles of the pelvic cavity during childbirth, …
This perineal rehabilitation is undoubtedly one of the effective methods to naturally improve the symptoms of early prolapse and prevent their deterioration. Thanks to perineal rehabilitation, some surgeries can be avoided.
In addition, if the surgical act has become necessary, perineal rehabilitation is still recommended in order to facilitate postoperative recovery.
Prescribed by a doctor and performed by a physiotherapist, this technique is the same as that which is routinely prescribed following childbirth in order to regain good bodybuilding requiring consolidation of the pelvic floor.
Complementary approaches to treat genital prolapse
Homeopathy
There are several homeopathic remedies available for prolapse, whether uterine or rectal.
Uterine prolapse:
- Helonias dioica in 5 CH to calm the pain
- but also Kalium bichromicum (if worsening in hot weather).
- You can also take Collinsonia canadensis or Calcarea phosphorica (one dose of 9 CH per week) in case of worsening with exertion.
Rectal prolapse:
- Podophyllum peltatum and if it follows a childbirth we will take Ruta graveolens. We can also turn to Hydrastis canadensis.
Phytotherapy
In herbal medicine, to fight against uterine prolapse, it is recommended to drink decoctions of white ash bark (Fraxinus americana).