Contents
Gastrostomy
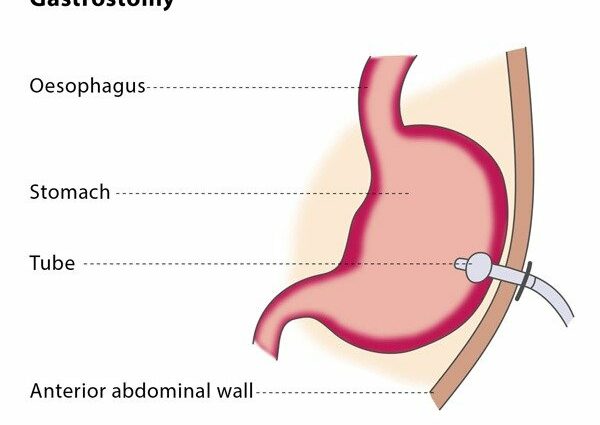
Sometimes some people can no longer eat orally, as in the case of swallowing disorders. Enteral nutrition can then be used to nourish them, thanks to an intervention: gastrostomy.
This allows the stomach to communicate with the outside, via an orifice made in the abdomen. A probe will then give the possibility of introducing food directly into the stomach: this is called enteral nutrition.
Complications can sometimes occur, but they are rare. This procedure, called more precisely percutaneous endoscopic gastrostomy, is widely used worldwide, this operation being well controlled, very safe, and effective in patients with a functional gastrointestinal system.
What is a gastrostomy?
The first expression of the concept of gastrostomy dates back to 1837, but it was not until 1876 that the first gastrostomy operations were successfully performed in humans. It was in 1980 that the most widely used technique in the world at present was established, by Gauderer et al: this is the so-called percutaneous endoscopic gastrostomy technique, or GPE. This operation consists of making an orifice in the stomach and adding a feeding tube to it. It will allow, by means of a tubing and nutrition bags, enteral nutrition, to be provided directly in the stomach of the patient who can no longer eat orally (by mouth).
The operation to insert the gastrostomy tube is done via endoscopy (using an endoscope, a flexible tube fitted with a lamp and a camera that allow visualization of the cavities of the organs), or by radiological imaging, or even through surgical techniques such as an opening or laparoscopy (also called laparoscopy, laparoscopy is a surgical technique that allows intervention on the viscera of the abdominal cavity with minimal opening of the abdominal wall ).
How is a gastrostomy performed?
Preparing for the gastrostomy
- Informed consent must be obtained from the patient, or his legal decision-making guardians. Informed consent aims to ensure that the care given to the patient is explained to him, giving him full information on the benefits and risks of enteral feeding, before the gastrostomy procedure.
- The patient should be on an empty stomach all night before the operation (for eight hours).
- The patient is given preventive antibiotics one hour before the gastrostomy tube is placed. The standard antibiotic therapy thus consists of administering 1 to 2 grams of cefazolin intravenously.
Course of the gastrostomy operation
In most cases, general anesthesia is not necessary, local anesthesia is sufficient. Several techniques have been developed to insert the gastrostomy tube. Generally, all of these methods share a common concept, that of inserting the gastrostomy tube through the abdominal wall, at a point where the stomach and the wall of the abdomen are in close contact. Here is a brief description of the three most common techniques in clinical practice:
- The method initially introduced by Gauderer et al is still the most widely used today to introduce a gastrostomy tube, or GPE tube. A cord is inserted with a needle through the abdominal wall inside the stomach, grasped with forceps via endoscopy and brought back through the esophagus and mouth. The cord is then attached to the terminal end of the feeding tube and the tube is brought from the mouth to the esophagus and stomach, then exits through the abdominal wall.
- A second technique starts in the same way. A wire used as a guide is inserted into the stomach and out through the mouth using the endoscope. The feeding tube is pushed over the guidewire into the stomach and out of the puncture site. There is no significant difference in terms of complication or efficacy with the first method.
- A third technique, called the Russell technique, uses the Seldinger method to place a guidewire in the stomach via endoscopy. Then an expanding catheter and sheath pass over the guidewire and after removal of the guidewire, the feed tube is advanced through the sheath, which is brought out.
Why do a gastrostomy?
Gastrostomy is indicated in patients who are unable to eat enough food by mouth, especially with swallowing disorders. Thus, enteral nutrition, that is, food arriving directly in the stomach via a gastrostomy tube and a tubing system, will allow them to ensure a sufficient nutritional intake, meeting their metabolic needs. It is therefore performed in patients at risk of severe to moderate malnutrition.
- When patients have a functional gastrointestinal system, this enteral route will be preferred to parenteral nutrition, or nutrition through the blood via an infusion: this intravenous route involves more risks and its cost is higher.
- Nasoenteric tubes, either passing through the nasal route (nasogastric, nasoduodenal and nasojejunal) are usually reserved for short-term enteral foods (less than thirty days) in patients with intact airway reflexes, especially as they also carry a greater risk of irritation, or oesophageal reflux, for example.
The aim of enteral nutrition is therefore not only to improve the survival of the patient with a swallowing disorder, as well as his nutritional status, but also to improve the quality of life. In fact, the conditions for which patients are brought to feed enterically are found, in some cases, as a result of these pathologies:
- neurological diseases and psychomotor retardation, such as: cerebrovascular disease with swallowing disorder, motor neuron disease (such as amyotrophic lateral sclerosis), multiple sclerosis, Parkinson’s disease, cerebral palsy, dementia, brain tumor, psychomotor retardation;
- reduced level of consciousness: head injury, intensive care patients, prolonged coma;
- cancer: head and neck cancer, esophageal cancer;
- miscellaneous: burns, congenital anomalies (such as fistulas of the esophageal trachea), fistulas, cystic fibrosis, intestinal syndromes (such as Crohn’s disease), facial surgery, multiple trauma, chronic renal failure, AIDS;
- abdominal malignancy.
The expected results
The days following the operation: care to be taken
Pain relief is essential following insertion of the gastrostomy tube. Many patients report abdominal discomfort, linked to the swelling of the stomach during the procedure. The stoma opening should be monitored and disinfected every other day.
Rare complications
Gastrostomy is usually considered to be a safe procedure. However, complications can arise, divided into minor or major complications. The mortality rate for the procedure is very low, but it may increase in patients with underlying comorbidities.
Among the minor complications:
- wound infection;
- leakage of the tube to the abdominal cavity;
- leaking stoma (the opening made);
- inadvertent removal of the gastrostomy tube;
- blockage of the tube;
- pneumoperitoneum (presence of air in the peritoneum);
- gastric obstruction;
- peritonitis.
Among the major complications:
- hemorrhage;
- toxic shock syndrome;
- perforation of the intestine;
- necrotizing fasciitis (infection that spreads quickly and affects the subcutaneous layers and the fat layer);
- metastatic swarming.
Expected result: prevent significant weight loss
There are a significant number of patients who can expect real medical benefit from the placement of a gastrostomy tube. Thus, a prospective study carried out over four years in 210 patients suffering from serious diseases or benign showed that they had lost around 11,35 kg (more or less 1,5 kg) during the three months preceding the operation; the mean weight gain at the end of twelve months of enteral food via a GPE tube was 3,5 kg (+/- 1,7 kg).
Thus, the major gain expected following a gastrostomy is that of preventing greater weight loss which was linked to the difficulty or inability to eat by mouth.