Contents
Gammapathy
Monoclonal gammopathy (GM) is defined by the presence in the serum and / or urine of a monoclonal immunoglobulin. It can be associated with a malignant hemopathy, otherwise it is called monoclonal gammopathy of undetermined significance (GMSI).
For the diagnosis, microbiological examinations make it possible to identify the monoclonal immunoglobulin in overabundance. Clinical, biological and radiological manifestations can point to a hemopathy whereas the diagnosis of a GMSI is a differential diagnosis.
What is monoclonal gammopathy?
Definition
Monoclonal gammopathy (GM) is defined by the presence in the serum and / or urine of a monoclonal immunoglobulin. Immunoglobulins are proteins in human plasma that have immune properties. They are synthesized in plasma cells, cells of the lymphoid system formed in the spleen and lymph nodes. GM therefore testifies to the proliferation of a clone of plasma cells producing a monoclonal immunoglobulin.
Types
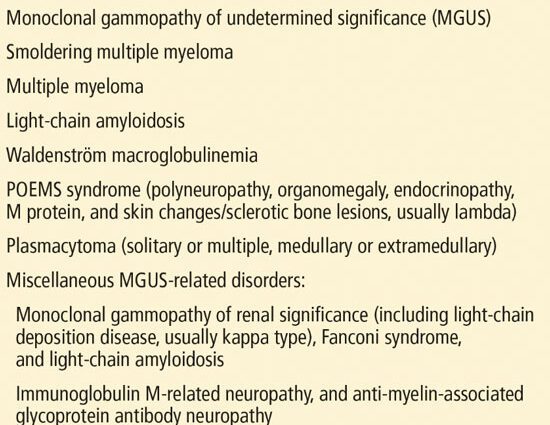
GMs can be classified into 2 categories:
- Monoclonal gammopathies associated with hematologic malignancies
- Monoclonal gammopathies of undetermined significance (GMSI)
Causes
For monoclonal gammopathies associated with malignant hemopathies, the main causes are:
- Multiple myeloma: tumor of the bone marrow formed from a proliferation of abnormal plasma cells
- Macroglobulinemia (Waldenström’s disease): presence in abnormal amounts in the plasma of macroglobulin
- B lymphoma
GMSI can be associated with various non-malignant pathologies:
- Autoimmune diseases (rheumatoid polyathritis, Sjögren’s syndrome, systemic lupus)
- Viral infections (mononucleosis, chickenpox, HIV, hepatitis C)
- Bacterial infections (endocarditis, osteomyelitis, tuberculosis)
- Parasitic infections (leishmaniasis, malaria, toxoplasmosis)
- Chronic diseases like chronic cholecystitis (inflammation of the gallbladder)
- Various other conditions such as familial hypercholesterolemia, Gaucher’s disease, Kaposi’s sarcoma, lichen, liver disease, myasthenia gravis (disorder of the transmission of nerve impulses from the nerve to the muscle), anemia or thyrotoxicosis
Diagnostic
GM is often detected incidentally, during laboratory tests performed for other reasons.
To identify the overabundant monoclonal agent, the most useful tests are:
- Electrophoresis of serum proteins: a technique allowing to identify and separate the proteins of a serum under the action of an electric field
- Immunofixation: a technique allowing the detection and typing of monoclonal immunoglobulins
- Immunoglobulin assay: a process that separates proteins from plasma and identifies them on the basis of detectable immunological reactions they produce
Then the diagnosis goes through looking for the cause of GM. Various clinical, biological or radiological manifestations should suggest multiple myeloma:
- Weight loss, inflammatory bone pain, pathological fractures
- Anemia, hypercalcemia, renal failure
Other manifestations immediately point to a hemopathy:
- Lymphadenopathy, splenomegaly
- Abnormalities in the blood count: anemia, thrombocytopenia, excessive lymphocytosis
- Syndrome d’hyperviscosité
GMSI is defined as GM without any clinical or laboratory signs of hematologic malignancy. In clinical routine, this is a diagnosis of exclusion. The criteria used to define a GMSI are:
- Monoclonal component rate <30 g / l
- Relative stability over time of the monoclonal component
- Normal serum level of other immunoglobulins
- Absence of destructive bone damage, anemia and kidney disorder
The incidence of GMSI increases with age from 1% at 25 years to more than 5% beyond 70 years.
Symptoms of monoclonal gammopathy
GMSI is usually asymptomatic. However, the monoclonal antibody can bind to nerves and cause numbness, tingling, and weakness. People with the condition are more likely to have destruction of bone tissue and fractures.
When GM is associated with another disease, the symptoms are those of the disease.
Furthermore, monoclonal immunoglobulins can cause relatively rare complications:
- Amyloidosis: deposits of fragments of monoclonal proteins in different organs (kidneys, heart, nerves, liver) which can be the cause of failure of these organs
- Plasma hyperviscosity syndrome: it is responsible for vision disorders, neurological signs (headache, dizziness, drowsiness, vigilance disorders) and hemorrhagic signs
- Cryoglobulinemia: diseases caused by the presence in the blood of immunoglobulins which precipitate when the temperature is below 37 °. They can cause skin manifestations (purpura, Raynaud’s phenomenon, extremity necrosis), polyarthralgia, neuritis and glomerular nephropathies.
Monoclonal gammopathy treatments
For IMGs, no treatment is recommended. Recent studies show that IMGTs with associated bone loss may benefit from treatment with bisphosphonates. Every 6 to 12 months, patients should undergo a clinical examination and perform serum and urine protein electrophoresis to assess disease progression.
In other cases, treatment is that of the cause.
Prevent monoclonal gammopathy
In a proportion of up to 25% of cases, the evolution of a GMSI towards a malignant hematologic disease is observed. People with GMSI are followed with a physical, blood and sometimes urine tests about twice a year to check for possible progression to a cancerous condition. If progression is discovered early, symptoms and complications can be prevented or treated earlier.