Contents
What is diffuse toxic goiter
The term “goiter” refers to an increase in thyroid tissue. If we are talking about diffuse goiter, this is a uniform growth of the entire gland without isolating individual sections (nodes). An increase in the size of the gland can be caused by various reasons, the most common of them all over the world is iodine deficiency in food. However, in second place are Graves’ disease and Hashimoto’s disease, and they are becoming more common.
Goiter is classified into different categories:
- morphology (nodular or diffuse);
- functional status (hyper-, hypo- or euthyroid);
- malignancy, etc.
By definition, “diffuse toxic” goiter refers to a dramatically enlarged thyroid gland that produces excessive amounts of thyroid hormones.
Causes of diffuse toxic goiter in adults
If we highlight the most common causes of goiter, the following categories are in the lead:
- iodine deficiency;
- autoimmune disorders;
- smoking;
- heredity (similar diseases in the family);
- drugs, eg lithium, iodides, interferon-alpha;
- radiation therapy;
- inflammation and various infections affecting the gland.
Diffuse toxic goiter (or DTG for short) is most often caused by autoimmune diseases such as Graves’ disease or autoimmune thyroiditis (at a certain stage of its development).
The most common cause of diffuse toxic goiter in our country is Graves’ disease (or Graves’ disease). This is the most common cause of hyperthyroidism, affecting 1 in 200 people.
It usually affects people between the ages of 30 and 50, but can occur in any age group. In women, DTG occurs 7-10 times more often than in men. There is also a marked increase in family morbidity.
Diffuse toxic goiter consists of a uniformly enlarged thyroid tissue of a rubbery consistency. Microscopically, the follicular cells are hypertrophied and hyperplastic with little colloid in them. Lymphocytes and plasma cells infiltrate the gland and may eventually aggregate into lymphoid follicles.
Not all cases of diffuse toxic goiter are provoked by Graves’ disease. They may have various non-autoimmune causative factors. But most cases are autoimmune in nature. In Graves disease, antibodies produced in the body are directed to the thyroid gland, more specifically to the stimulating hormone receptor (TSHr), which is present on follicular cells. Chronic stimulation of these receptors leads to the production of excess amounts of T3, T4 and, ultimately, to an enlargement of the thyroid gland, which leads to goiter.
Symptoms of diffuse toxic goiter in adults
It is not uncommon for patients to come to the doctor complaining of one or more of the effects of a hyperthyroid state (excess thyroid hormone). These include:
- weight loss without any dietary changes;
- heat intolerance, together with other symptoms associated with heat, such as polydipsia (increased thirst), sweating;
- tremor (trembling of the hands or the whole body);
- nervousness, anxiety, fatigue;
- cardiopalmus;
- dyspnea;
- frequent defecation, diarrhea;
- nausea, vomiting.
Patients may also complain of obvious swelling of the neck or feeling of a lump in the neck, difficulty swallowing, orthopnea (rapid breathing).
Patients with Graves’ disease may have these additional features:
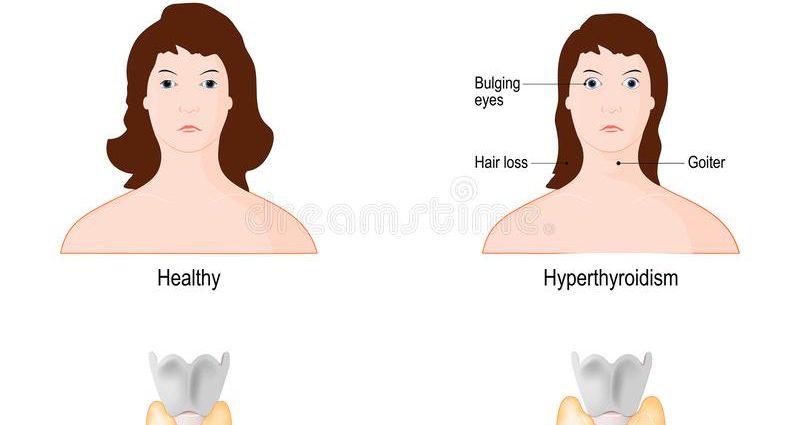
- ophthalmopathy or Graves’ orbitopathy (observed in 25% of patients) – the inability to close the eyelids, diplopia (double vision), periorbital edema, excessive lacrimation, etc.;
- thyroid dermatopathy (rare, occurs in 4% of patients and is usually associated with orbitopathy) – slightly thickened pigmented skin, especially in the pretibial region (on the anterior surface of the lower leg);
- the reproductive system suffers – women have frequent irregular menstruation.
Degrees of diffuse toxic goiter in adults
According to various classifications, the severity of diffuse toxic goiter among adult patients is divided into three or four categories. This largely depends on the severity of the enlargement of the thyroid gland itself and the severity of the symptoms present. The most common classification that divides the process into 4 categories:
1 severity – neurotic stage of the disease with a subtle increase in the gland, the predominance of psycho-emotional manifestations of hyperthyroidism.
2 degree – the so-called neurohormonal stage with a pronounced increase in the size of the thyroid gland and fairly pronounced symptoms of hyperthyroidism.
3 degree – it is also a visceropathic stage with an active increase in the gland and signs of damage to many internal organs.
4 degree with the cachectic stage of the disease – serious, sometimes irreversible damage develops in the tissues and organs of the body.
Treatment of diffuse toxic goiter in adults
In order to make an accurate diagnosis, an external examination of the patient, tests and diagnostic procedures are required, the results of which will prescribe one or another type of therapy.
Diagnostics
General physical examination findings in a patient with diffuse toxic goiter may show the following:
- uniform weight loss;
- swelling of the face, ears, neck, bulging eyes, eyelid lag, periorbital edema;
- cardiovascular system – tachycardia, irregular heartbeat, systolic hypertension;
- neuromuscular symptoms – tremor of the limbs, hyperreflexia, hyperactivity, muscle weakness;
- respiratory system – tachypnea.
- skin and extremities – moist, warm skin, pretibial myxedema.
The laboratory evaluation consists of a complete thyroid hormone profile, including serum T3, T4, and TSH levels. Serum TSH is the best screening test for assessing excess or deficiency of thyroid hormones.
In the case of diffuse toxic goiter, the above tests usually result in a low or normal TSH level with an elevated serum thyroid level. Additionally, a test is performed with the absorption of radioactive iodide, or a combination of ultrasound examination of the thyroid gland with the determination of antibodies to TSH receptors. High radioactive iodine uptake reflects Graves’ disease, as does an enlarged gland with positive TSH receptor antibodies (TRAb).
Modern treatments
Treatment options for diffuse toxic goiter include:
Antithyroid drugs (suppressing the work of the gland). There are two modes of drug administration, and the first is titration, in which the dose of drugs is reduced to the lowest possible dose when a euthyroid state is reached. The next regimen is block and replace, in which a high dose of antithyroid drugs is given along with thyroxine to maintain a euthyroid state.
The disadvantage of therapy is the risk of relapse, especially in the first year after stopping therapy. Studies show a 50% to 55% risk of recurrence with poor prognostic factors such as severe hyperthyroidism, large goiter, high T3:T4 ratio, persistent TSH suppression, and high baseline TRAb concentrations. Rare but serious side effects of ATD therapy include agranulocytosis, hepatotoxicity, and vasculitis.
Radioiodine therapy. It is the most common treatment for Graves’ disease and is a safe and effective treatment for DTG. Absolute contraindications for this therapy are pregnancy, lactation and severe uncontrolled thyrotoxicosis. Iodine can be administered in liquid or capsule form, and fixed dose therapy is just as effective as calculated dose therapy based on gland volume, iodine uptake, etc.
Patients should stop taking all iodine-containing drugs and follow an iodine-restricted diet to ensure efficient absorption. Therapy with antithyroid drugs should be stopped before the use of radioactive iodine and, if necessary, can be resumed a week after administration.
Possible side effects include the risk of developing hypothyroidism and, in rare cases, transient radiation hyperthyroidism or exacerbation of thyroid-related ophthalmopathy.
Operation. Thyroidectomy is the most successful form of treatment for diffuse toxic goiter, with total thyroidectomy being more successful than subtotal thyroidectomy with similar side effects.
Due to the side effects associated with the use of general anesthesia, recurrent laryngeal paralysis, hypothyroidism, this is usually the last line of treatment. It is preferred in patients who cannot tolerate antithyroid drugs or iodine, or in patients with symptoms of acute respiratory failure due to gland growth.
Prevention of diffuse toxic goiter in adults at home
Since the exact causes of DTG are unknown, it is impossible to develop clear schemes for the prevention of the disease. There are opportunities to prevent worsening of the condition before and after treatment.
Quitting smoking has a beneficial effect on the course of ophthalmopathy and the functioning of the thyroid gland in general.
The possibility of inheriting the disease requires that first-degree relatives, especially siblings and children, be aware of the increased risk of developing DTG or related disorders. Regular testing is not recommended, but if new symptoms appear, this risk should be considered and a doctor should be consulted.
Popular questions and answers
Issues related to diffuse toxic goiter, we discussed with general practitioner, endoscopist, head of the organizational and methodological office Lidia Golubenko.
● hyperthyroidism or thyroid crisis due to long-term untreated excess thyroid hormone;
● dermatopathy associated with Graves’ disease;
● Graves’ ophthalmopathy and vision problems, up to blindness.
Diffuse toxic goiter may present with strong hypermetabolic effects (eg, heat intolerance, persistent sweating, weight loss) and adrenergic symptoms (eg, palpitations, tremors, emotional lability, etc.). But older patients may not have adrenergic symptoms, rather lethargy, atrial fibrillation, and weight problems may also be a manifestation of depression, malignancy, or cardiac abnormalities.