Contents
Candida albicans: presence, function and treatments
Candida albicans is a fungus usually found in the flora of the mucous membranes. It is not pathogenic and contributes to the balance of our microbiota. However, an anarchic proliferation of this yeast is pathological: it is called candidiasis.
Candida albicans, what is it?
Candida albicans is a yeast-like fungus of the genus Candida and of the saccharomycetaceae family. Candida albicans is classified among the asexual fungi whose reproduction is predominantly clonal. Candida albicans is a diploid organism that has 8 pairs of chromosomes. Its heterozygosity gives it a great ability to adapt to various environments.
Candida albicans is naturally constitutive of the flora of the mucous membrane of the human being. Its presence is not pathological. We find this fungus in the digestive tract of 70% of healthy adults. However, a hormonal or immune imbalance can be responsible for an anarchic multiplication of this fungus which then causes certain symptoms. We are talking about candidiasis or even mycosis.
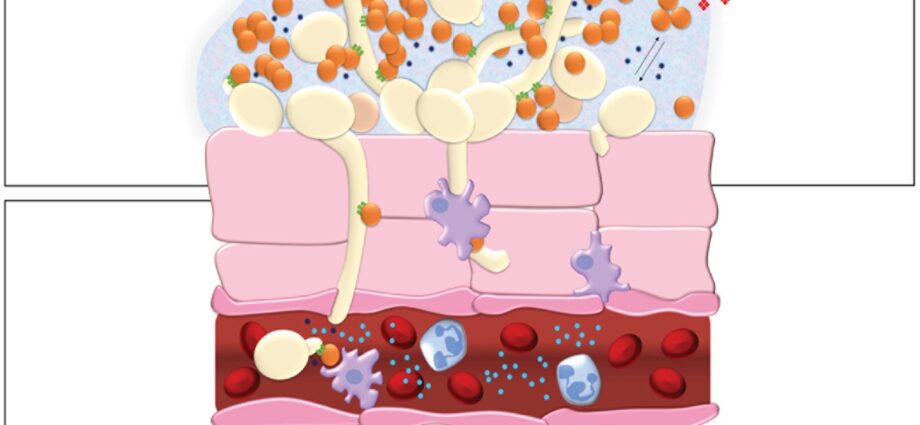
C. albicans virulence factors allow it to proliferate:
- dimorphism (transformation of yeast to fungus depending on the surrounding environment);
- adhesins (large number of surface receptors allowing C. albicans to easily adhere to the cells of its host);
- enzymatic secretions;
- etc.
C. albicans infections can be localized to the genital, oral or digestive mucosa. In addition, the overgrowth of Candida albicans on the skin is abnormal and causes skin signs. More rarely, in immunocompromised patients, C. albicans can colonize one or more organs or even the entire body: we speak of systemic candidiasis. In this case, the risk of death is around 40%.
Candida albicans: role and location
Candida albicans is a microorganism commensal to the microbial flora in humans and warm-blooded animals. It is present in the oral, digestive and genital mucous membranes, in the form of blastospores, considered to be the saprophytic form which lives in symbiosis with the host organism. In healthy subjects, the yeast is distributed differently depending on the sampling sites, the main reservoir remains the digestive tract:
- skin (3%);
- vagina (13%);
- tract ano-rectal (15%);
- oral cavity (18%);
- stomach and duodenum (36%);
- jejunum and ileum (41%).
However, these figures should be observed with caution insofar as the sampling techniques are not always identical and the sampling sites do not always present a homogeneous environment.
C.albicans is therefore necessary for the balance of the microbiota. However, when this balance in its commensal form and the immune defenses are broken, this symbiosis becomes parasitic. This results in an infectious disease called candidiasis.
What are the anomalies and pathologies caused by Candida albicans?
Candidiasis is a condition caused by the fungus Candida albicans. It is not a contagious disease: yeast is already present in the body, in the mucous membranes, mouth, digestive system and genitals. Candidiasis is linked to an anarchic proliferation of Candida albicans, itself caused by an immune or hormonal imbalance or a weakening of the microbial flora. In addition, genital yeast infections are not regarded as sexually transmitted infections (STIs), although sexual intercourse is a risk factor for yeast infections (the latter inducing a weakening of the genital flora).
However, human-to-human transmission of C. albicans is possible through contact with faeces, salivary secretions or through the hands. In hospitals, C. albicans represent the major cause of Nosocomial infections opportunistic.
Risk factors
Certain risk factors expose the development of candidiasis:
- repeated courses of antibiotics;
- taking treatments that impair immunity (corticosteroids, immunosuppressants, chemotherapy, etc.);
- a immunodépression (of congenital origin, linked to HIV or to a transplant).
Vaginal yeast infections are the most frequent candidiasis, affecting 10 to 20% of women during sexual activity. They are favored by:
- hormonal changes;
- taking estrogen-progestogen contraceptives;
- perspiration ;
- pants that are too tight;
- underwear that is not made of cotton (and especially thongs);
- wearing panty liners;
- poor hygiene;
- prolonged sexual intercourse.
Candidiasis and their treatments
Candidiasis | Symptoms and diagnosis | Treatments |
Cutaneous candidiasis |
|
|
Candidiasis of the nails |
|
|
Vaginal yeast infection |
|
|
Oral thrush |
|
|
Digestive candidiasis |
|
|
Systemic candidiasis |
|