Contents
What is a pulmonary embolism?
Although little known, this pathology is however more frequent than it seems. Pulmonary embolism occurs when clot that formed in the legs – phlebitis – goes back to the heart and mouth the pulmonary artery. Pregnant women are more likely to be affected by this disease, with one in 1 pregnancies affected by embolism. In 000% of cases, the outcome can be fatal: “It is still today the leading cause of death for pregnant women in Western countries, because the symptoms are difficult to spot », Reveals Dr Gilbert Pochmalicki.
>> To read also: Pregnancy and health, all you need to know
“Pulmonary embolism occurs when a clot that has formed in the legs – phlebitis – travels up to the heart and clogs the pulmonary artery.”
What are the causes of pulmonary embolism?
Why there pregnant woman is it more affected? The first explanation is that the uterus, by enlarging, compresses the veins and prevents blood from circulating correctly. Moreover, as Dr Gilbert Pochmalicki points out, the hormonal fluctuations suffered during pregnancy can be an aggravating factor: “Hormones, especially estrogen, damage the lining of the vein, which can also undergo a real trauma during childbirth. »Excluding pregnancy, hormonal treatments can also promote the development of a phlebitis, whether it is those which one undergoes within the framework of a stimulation of ovulation, or with 3rd and 4th pillsgenerations, which have been the subject of much controversy recently.
Finally, if there are cases of bleeding disorders in the family – in young people – you will have a greater risk of developing phlebitis yourself during your pregnancy: “The blood thickens naturally when you are pregnant in order to avoid bleeding, specifies Gilbert Pochmalicki, but if you have thicker blood correlated with hypercoagulability, this can promote pulmonary embolism. “Among the other contributing factors, the doctor cites obesity, immobilization, the tobacco, as well as pregnancies beyond 35 years.
>> To read also: How to stop smoking while pregnant?
Recognize the symptoms of pulmonary embolism
If pulmonary embolism is so complicated to detect during pregnancy, its symptoms are similar to those experienced by almost all pregnant women. For example, the sensation of heavy or swollen legs may well be a sign of phlebitis, as it may be a trivial side effect of pregnancy. Just like the weight gain, the feeling breathless at the slightest effort, or the heartbeat which is accelerating. These are not serious symptoms that are completely common for most pregnant women, but which can also alert your doctor. It is then necessary to compare the different symptoms and the family history in order to assess the risks and be able to make a diagnosis.
>> To read also: How many kilos during pregnancy?
Make a diagnosis of pulmonary embolism
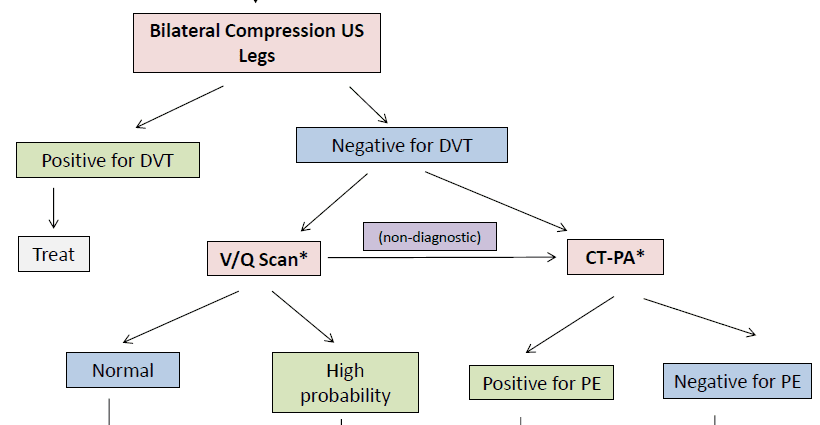
For Dr Gilbert Pochmalicki, the diagnostic pulmonary embolism must imperatively be placed or eliminated during pregnancy because “in pregnant women, doubt is not allowed”. The first analysis to do is a simple blood test which has only a negative value, that is to say that it only allows to eliminate the phlebitis. If the result is positive, further tests should be done to confirm the diagnosis. a doppler legs will first be used to observe the circulation in the veins “without risk for the mother and the fetus, and without any pain,” says the cardiologist. If nothing is found but a doubt remains, it is then necessary to undergo a CT angiography or a scintigraphy. “
These two methods ofmedical imaging are often the object of anguish for mothers-to-be who are worried about the danger of radiation for their baby. But for Gilbert Pochmalicki, “this risk is low, and it is negligible compared to missing out on a pulmonary embolism. You have to prioritize, and know with certainty. “
>> To read also: What do you know about pregnancy exams?
How is a pulmonary embolism treated?
As we have seen, if the clot is large, the pulmonary embolism can block the arteries and be fatal for the mother. This is why, as soon as the diagnosis is mentioned, the mother-to-be is immediately treated by anticoagulants. ” It is heparin shots, which work faster than tablets. It is prescribed throughout pregnancy, and usually up to six weeks after childbirth. The risk remains because the vessels were shaken during birth, ”explains Gilbert Pochmalicki. The mother is then followed by a pulmonologist or a cardiologist to check that everything is back to normal. And in a future pregnancy, the doctor will prescribe a preventive treatment in order to avoid the risk of recurrence.
“As soon as the diagnosis is mentioned, the mother-to-be is immediately treated with anticoagulants.”
Author: Tiphaine Lévy-Frébault