Contents
Oligospermia: definition, causes, symptoms and treatments
Oligospermia is a sperm abnormality characterized by an abnormally low amount of sperm. Depending on its degree and other possibly associated spermatic abnormalities, it can have an impact on a man’s fertility and be responsible for difficulties in having a baby.
What is oligospermia
Oligospermia, or oligozoospermia, is a sperm abnormality characterized by a sperm concentration below normal values. A man’s fertility may be reduced, and the couple may have difficulty conceiving. However, if the sperm concentration is an important parameter, it is not a discriminating factor for male fertility, unlike azoospermia (total absence of spermatozoa). In theory, it only takes one sperm for fertilization to take place.
Oligospermia can exist in isolation, but it is often associated with other sperm abnormalities: asthenospermia (insufficient mobility of sperm) and teratozoospermia (too many abnormally shaped sperm). This is called oligo-astheno-teratozoospermia (OATS). The impact on fertility is in this case more important, because the fertilizing power of the spermatozoa (already less numerous) is altered due to their morphological defect and their reduced mobility.
The causes
As with all sperm abnormalities, different causes can be at the origin of oligospermia because many factors can alter the process of spermatogenesis:
- an infection that has resulted in obstruction of the vas deferens or inflammation of the seminal vesicles;
- a lack of hormonal stimulation (extreme oligospermia);
- lesion of a testicle following infection (orchitis), surgery, poorly managed testicular torsion;
- a genetic abnormality (severe oligospermia);
- a varicocele;
- certain drug treatments (chemotherapy, anabolic steroids, hypertension medications, gout medication, interferon prescribed for certain viral diseases, etc.);
- exposure to certain toxic substances: alcohol, drugs, tobacco (including for in utero exposure), and probably certain environmental pollutants (phthalates, pesticides);
- exposure of the testes to high temperature in certain high-risk occupations;
- general disease (liver, kidney).
Depending on its origin, oligospermia can be transient or irreversible. But often oligospermia remains of unknown origin.
Symptoms
Oligospermia is not manifested by any symptoms, other than a difficulty conceiving for the couple.
The diagnosis
Oligospermia is diagnosed during the spermogram systematically performed in men during an infertility assessment. During this semen analysis, various parameters are evaluated:
- the pH of the semen;
- the volume of the ejaculate;
- sperm concentration;
- sperm mobility;
- sperm morphology;
- sperm vitality.
The results are compared with the threshold values defined by the WHO (1). If the sperm concentration is less than 15 million / ml of ejaculate or 39 million / ejaculate, oligospermia is suspected.
A second or even a third spermogram will be performed 3 months apart (one cycle of spermatogenesis lasting 74 days) to confirm the diagnosis. The number of ejaculated sperm can indeed vary considerably from one ejaculation to another depending on different factors (length of abstinence before collection, fatigue, infection, stress, exposure to toxic substances, etc.), and oligospermia may in some cases only be transient.
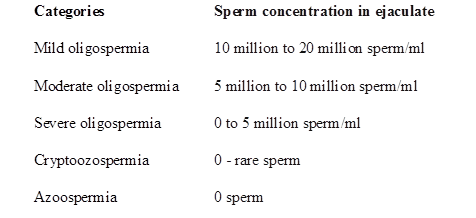
Depending on the results, different degrees of oligospermia are distinguished:
- mild oligospermia: between 5 and 14 million spermatozoa / ml;
- moderate oligospermia: between 1 and 5 million spermatozoa / ml;
- severe oligospermia: concentration less than 1 million / ml.
Other examinations may be prescribed to better assess the impact of oligospermia on the fertility of men, to detect the cause of this oligospermia and to guide the management:
- the migration-survival test (TMS) or selection-survival test, generally carried out after the spermogram and systematically before any MPA technique, allows, after centrifugation of the sperm which will select the “best spermatozoa”, to evaluate their number , their mobility and their survival at 24 hours and thus to estimate the number of spermatozoa able, in the end, to fertilize an oocyte;
- a hormonal assessment to detect a possible hormonal insufficiency;
- an ultrasound of the testicles,
- etc.
Treatment and prevention
The management of oligospermia depends on its cause, if it is found.
If a toxic cause is suspected (consumption of alcohol, drugs, etc.), humans should limit their exposure to the toxicant. A spermogram will be performed again to check the count. In case of varicocele, a varicocele cure may be offered. If the cause is hormonal, hormonal treatment allows, in certain situations, to restart spermatogenesis.
If oligospermia cannot be treated, different AMP techniques will be offered to the couple depending on the degree of oligospermia and the results of TMS:
- intrauterine insemination (IUI) if the MSD shows at least 500 to 000 million motile sperm. The simplest technique of ART, artificial insemination consists of depositing the most fertile spermatozoa in the uterus at the time of ovulation (induced in women after light stimulation);
- in vitro fertilization (IVF) may be offered in the event of failure of IUI, in the event of oligospermia or more severe OATS. IVF involves reproducing in the laboratory fertilization and the very first stages of embryonic development. For this, oocytes are collected from the woman after ovarian stimulation, then brought into contact with previously prepared spermatozoa;
- in vitro fertilization with microinjection (ICSI) is often offered in severe oligospermia. This technique consists of selecting and preparing a sperm to inject it directly into the mature oocyte, for “forced” fertilization.