Causes of the disease
Necrosis is the irreversible cessation of the vital activity of cells, tissues or organs in a living organism, caused by the influence of pathogenic microbes. The cause of necrosis may be tissue destruction by a mechanical, thermal, chemical, infectious-toxic agent. This phenomenon occurs due to an allergic reaction, impaired innervation and blood circulation. The severity of necrosis depends on the general condition of the body and adverse local factors.
The development of necrosis is facilitated by the presence of pathogenic microorganisms, fungi, viruses. Also, cooling in the area where there is a violation of blood circulation has a negative effect, in such conditions, vasospasm increases and blood circulation is even more disturbed. Excessive overheating affects the increase in metabolism and with a lack of blood circulation, necrotic processes appear.
Symptoms of necrosis
Numbness, lack of sensitivity is the very first symptom that should be the reason for visiting a doctor. Paleness of the skin is observed as a result of improper blood circulation, gradually the skin color becomes cyanotic, then black or dark green. If necrosis occurs in the lower extremities, then at first it is manifested by rapid fatigue when walking, a feeling of cold, convulsions, the appearance of lameness, after which non-healing trophic ulcers form, necrotic over time.
The deterioration of the general condition of the body occurs from violations of the functions of the central nervous system, blood circulation, respiratory system, kidneys, liver. At the same time, there is a decrease in immunity due to the appearance of concomitant blood diseases and anemia. There is a metabolic disorder, exhaustion, hypovitaminosis and overwork.
Types of necrosis
Depending on what changes occur in the tissues, two forms of necrosis are distinguished:
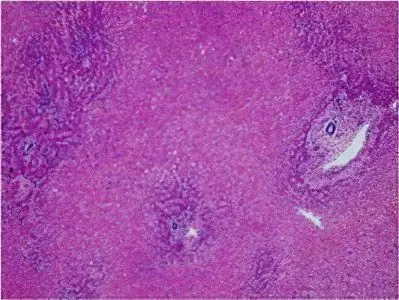
Coagulative (dry) necrosis – occurs when tissue protein folds, thickens, dries out and turns into a curdled mass. This is the result of the cessation of blood flow and the evaporation of moisture. At the same time, tissue areas are dry, brittle, dark brown or gray-yellow in color with a clear demarcation line. At the site of rejection of dead tissues, an ulcer occurs, a purulent process develops, an abscess is formed, and a fistula forms upon opening. Dry necrosis is formed in the spleen, kidneys, umbilical cord stump in newborns.
Colliquation (wet) necrosis – manifested by swelling, softening and liquefaction of dead tissues, the formation of a gray mass, the appearance of a putrid odor.
There are several types of necrosis:
Heart attack – occurs as a result of a sudden cessation of blood supply in the focus of a tissue or organ. The term ischemic necrosis means necrosis of a part of an internal organ – infarction of the brain, heart, intestines, lung, kidney, spleen. With a small infarction, autolytic melting or resorption and complete tissue repair occur. The unfavorable outcome of a heart attack is a violation of the vital activity of the tissue, complications or death.
Sequester – a dead area of bone tissue is located in the sequester cavity, separated from healthy tissue due to a purulent process (osteomyelitis).
Gangrene – necrosis of the skin, mucous surfaces, muscles. Its development is preceded by tissue necrosis.
Bedsores – occur in immobilized people due to prolonged compression of tissues or damage to the skin. All this leads to the formation of deep, purulent ulcers.
Diagnostics
Unfortunately, often patients are sent for an examination performed using x-rays, but this method does not allow to detect pathology at the very beginning of its development. Necrosis on x-rays is noticeable only in the second and third stages of the disease. Blood tests also do not give effective results in the study of this problem. Today, modern magnetic resonance imaging or computed tomography devices make it possible to timely and accurately determine changes in the tissue structure.
Outcome
The outcome of necrosis is favorable if there is an enzymatic melting of the tissue, the germination of the connective tissue in the remaining dead tissue, and a scar is formed. The area of necrosis can become overgrown with connective tissue – a capsule (encapsulation) is formed. Even in the area of dead tissue, bone can form (ossification).
With an unfavorable outcome, purulent fusion occurs, which is complicated by bleeding, the spread of the focus – sepsis develops.
Death is typical for ischemic strokes, myocardial infarction. Necrosis of the cortical layer of the kidneys, necrosis of the pancreas (pancreatic necrosis) and. etc. – lesions of vital organs lead to death.
Treatment
Treatment of any type of necrosis will be successful if the disease is detected at an early stage. There are many methods of conservative, sparing and functional treatment, only a highly qualified specialist can determine which one is best suited for the most effective result.









