Contents
Medical treatments for ulcerative colitis (ulcerative colitis)
There is no medication to cure ulcerative colitis; on the other hand, several treatments make it possible to reduce inflammation and symptoms when the disease is active, and decrease their recurrence by maintaining remission.
pharmaceuticals
Anti-inflammatory. This is usually the first treatment prescribed for ulcerative colitis. They understand :
Aminosalicylates. These drugs are similar to aspirin and decrease inflammation in the colon. Commonly used aminosalicylates are sulfasalazine (Azulfidine®) and mesalazine or mesalamine (Pentasa®, Rowasa®, Fivasa® Canasa®, Asacol® Apriso ™, Lialda®). Newer drugs, balsalazide (Colazal®) and olsalazine (Dipentum®), are also used. They are administered by oralrectal or enema and are used both to calm relapses and to maintain remission. The most common side effects are nausea, vomiting and headache;
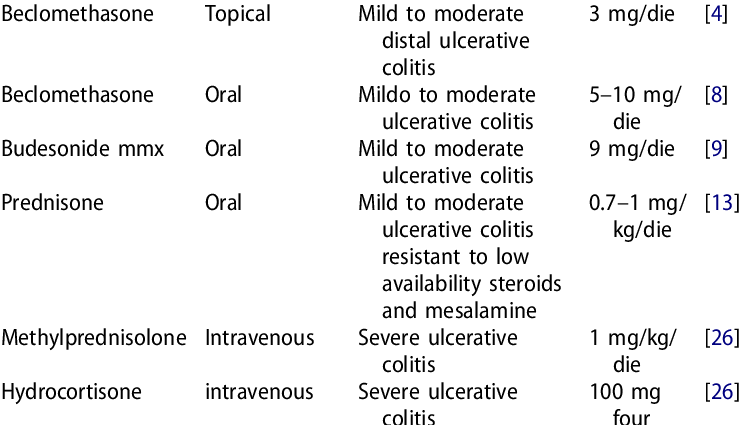
corticosteroids. Treatment almost essential to the treatment of UC, Corticosteroids stop inflammation, but have their share of side effects.
The most commonly prescribed corticosteroids for ulcerative colitis are prednisone, methylprednisolone, and hydrocortisone.
They are prescribed for patients with moderate or severe ulcerative colitis who do not respond to aminosalicylates.
They are administered either by voie digestive, oral or rectal (foam, suppositories, enema) in moderate seizures, left or rectal colic, either by intravenous route in the event of a serious crisis.
Their side effects are numerous, which limits their long-term use. They are generally prescribed for short periods: maximum dose over 10-15 days then the decrease must be gradual.
Rectally administered budesonide or beclomethasone dipropionate are corticosteroids that work almost exclusively in the colon. They are little or not absorbed by the mucosa, and therefore cause fewer side effects than other corticosteroids. They have no indication for induction therapy or maintenance of remission. They are used for milder cases of ulcerative colitis because they are a little less potent5,6.
Treatment should never be stopped abruptly.
Immunosuppressants. Immunosuppressants suppress inflammation by acting directly on the immune system, that is, by reducing the immune response that is the source of the inflammation. They are prescribed to sufferers who respond poorly to aminosalicylates and corticosteroids or to those who need to take high doses to maintain remission. The most common are azathioprine (Imuran® Imurel®) and 6-mercaptopurine (Purinethol®). Cyclosporine (Neoral®, Sandimmune®) is sometimes used in severe flare-ups. Immunosuppressants relieve symptoms of ulcerative colitis, but take a long time to work. It takes a minimum of 3 months before the molecule is fully effective. They also have their share of side effects, since they reduce resistance to infections and cancers. According to recent studies, other drugs, such as mycophenolate mofetil or tacrolimus, may also be effective.6.
Le Methotrexate may be effective in people who are resistant or intolerant to azathioprine. It is administered intramuscularly.
Agents anti-TNF alpha. Anti-TNF alpha agents are newer drugs that target a pro-inflammatory substance called tumor necrosis factor (TNF). The use of anti TNF alpha drugs has been shown to reduce the need for surgery, the number of hospitalizations, allow corticosteroid withdrawal, better mucosal healing and improve quality of life by maintaining remission of the disease. Infliximab (Remicade®) is used in people with a moderate to severe flare who are resistant to conventional treatments.
Symptomatic treatments
Antidiarrheals. These drugs should not be used without your doctor’s advice, as they may increase the risk of toxic megacolon. They slow down the transit of food through the intestine and therefore prevent diarrhea. Imodium® is effective but should be used with caution, under medical supervision.
Antispasmodics. These drugs can be used occasionally to relieve abdominal pain, but they are usually not very effective. Their action against spasms can be exerted on nerve fibers, muscle fibers, or both.
Contraindication : taking nonsteroidal anti-inflammatory drugs such as aspirin, ibuprofen (Advil®, Motrin®) or naproxen (Aleve®) can worsen symptoms of ulcerative colitis. To relieve mild abdominal pain, use acetaminophen (Tylenol®) instead. |
Experimental treatment: transdermal nicotine patches. This is an unvalidated treatment strategy! The idea for this treatment came from an observation: people with ulcerative colitis who start or resume smoking often see their condition improve. Several clinical studies have been carried out to assess the relevance of using nicotine (per patch) to control symptoms of ulcerative colitis and promote remission7. In 2004, a review of available studies concluded that nicotine patches were more effective than placebo at inducing remission, but that they were not superior to mesalamine or corticosteroids. Side effects (nausea and dizziness) were more numerous with nicotine patches than with other treatments8. Notes. Of course, doctors advise their patients not to smoke despite the beneficial effects of nicotine on ulcerative colitis, because tobacco has all the other side effects on the arteries and the risk of cancer. |
Support feeding
Supportive feeding aims to correct a possible malnutrition in terms of calories and micronutrients. Lack of appetite and frequent weight loss are the consequences of abdominal pain and diarrhea. In addition, ulcerative colitis and surgical procedures can lead to poor absorption of nutrients, which causes shortcomings in proteins, vitamins (A, B9, B12, C, D, E and K) and minerals (calcium, copper, iron, magnesium, selenium and zinc). These deficits are easily addressed by a balanced diet and rich in macro and micronutrients. The nutritional strategy will be developed in collaboration with the doctor.
In the event of anemia, treatment will be by mouth in the form of iron supplements, vitamin and mineral complexes or in the form of high calorie fluids. If the intestine is too irritated, in severe forms of the disease, the intravenous route will be used instead. Adequate nutrient intake is especially important in growing children.
surgery
Some people with ulcerative colitis will need to have surgery to remove the entire colon when medications are no longer able to control symptoms, in severe complicated acute colitis (colectasia, bleeding, perforation), or in patients at risk. of colorectal cancer.
- La colo-proctectomy, is surgery to remove the colon and rectum, the only way to cure ulcerative colitis. The surgeon proceeds to:
A ileoanale anastomosis, reference intervention during which the surgeon removes the colon and the diseased rectum, while preserving the anus and the external muscles of the rectum. It then connects the ileum (the last segment of the small intestine) to the anus, creating a pocket (the ileal reservoir) where the stool will collect before being evacuated almost normally. This intervention can lead to pouchite, that is, inflammation of the ileal reservoir, which is treated with antibiotics.
A ileorectal anastomosis can be proposed in the event of a conservable rectum in the elderly, with poor sphincter function, or in the event of doubtful diagnosis (the drug team does not know for sure whether it is ulcerative colitis or a disease de crohn) and in women wishing to become pregnant.