Contents
In modern society, approximately 10-25% of families are infertile. Contrary to traditional opinion, a woman is not always “guilty” of the absence of children in the family. According to statistics, from 30 to 50% of couples cannot have a child due to male infertility. Such areas of medicine as andrology and urology deal with this problem.
How is the reproductive system in men

The male genital organs are located not only inside the small pelvis, but also outside it. The main male hormone testosterone is responsible for the formation of secondary genital organs. It is produced by the testicles located in the scrotum. They also produce sperm, which travels from the testicles to the epididymis for nourishment and maturation. After maturation, the sperm travels through the vas deferens to the seminal vesicles for storage. The cycle of formation of a full-fledged sperm takes about 72 hours. During ejaculation, it mixes with the secretion of the prostate gland, as a result of which an ejaculate is formed – seminal fluid containing spermatozoa.
The ability to produce offspring (fertility) of men depends on the quality of sperm, its full development and maturation.
This process occurs with the participation of hormones:
Testosterone;
Luteinizing hormone (LH) – stimulates spermatogenesis in Leydig cells;
Follicle-stimulating hormone (FSH) – stimulates spermatogenesis in Sertoli cells.
In Sertoli cells, immature sperm forms spermatozoa and matures. Giving sperm motility occurs in the epididymis. Sperm, ready for fertilization, is stored in the vas deferens until ejaculation.
Sperm characteristic
The amount of sperm depends on the age of the man, his sexual activity and individual characteristics. Frequent intercourse reduces the volume of sperm, but it is restored after 2-3 days of abstinence.
Normally, the volume of the ejaculate is 1-6 ml, the sperm has an alkaline reaction with a pH of 7-7,6. These indicators do not allow spermatozoa to lose their mobility in the acidic environment of the vagina. Without losing their properties, they reach the cervical canal of the cervix, whose pH is 7,5, and from there they penetrate into the uterus and into the fallopian tubes to fertilize a mature egg.
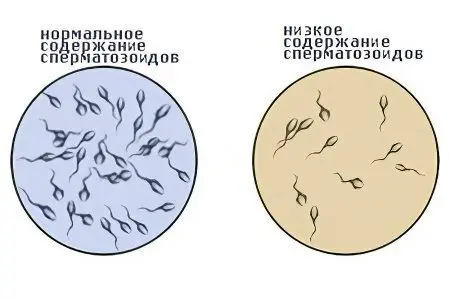
The spermatozoon consists of a head and a tail with an intermediate part (neck) between them. It makes rectilinear and translational movements to increase the possibility of meeting with the egg. One milliliter of ejaculate contains 40 to 120 million spermatozoa. Of these, about 60% are mobile, 15-20% are immobile. In the same ratio, mature and atypical forms of spermatozoa are present in the semen (60% – mature, 15-20% – atypical).
The study of the composition and quality of sperm (spermogram) is an analysis carried out primarily in the diagnosis of male infertility.
Classification of infertility in men

The variety of causes of male sterility makes it difficult to choose the basis for classification. Forms of infertility distinguished in andrology:
secretory infertility. Pathology consists in the production of sedentary or defective sperm by the testicles, as well as in the amount of motile sperm that is insufficient for fertilization. Infertility can be caused by congenital and acquired negative factors.
Obstructive or excretory infertility. With this form of infertility, sperm mature in sufficient quantities, but cannot get through the vas deferens into the urethra. The reason is an obstacle in the way of their transportation.
Combined infertility. The combination of several types of infertility (immunological, secretory, obstructive) with the addition of an inflammatory process.
immunological infertility. In the body of a man, the secretion of antibodies with anti-testicular functions is carried out, for which the testicular tissue is a foreign element. Antibodies penetrate into the cells of the testicles, violating the hematotesticular barrier, provoke the formation of antibodies to spermatozoa. The cause of this form of infertility is trauma to the testicles.
Relative infertility. Occurs against the background of the absolute health of both spouses, the problem of this form of infertility is little studied.
What causes male infertility?
The factors for the appearance of male infertility are conditionally divided into the main ones, which are more common than others, and additional ones, acting in combination with them. Secretory infertility (hypogonadism) is characterized by impaired spermatogenesis and testicular function. Hypogonadism can be primary or secondary. In the primary form of secretory infertility, there is an increased excretion of gonadotropins in the urine, leading to a decrease in the effect of the testicles on the functions of the pituitary gland. In the secondary form of hypogonadism, the affected pituitary gland negatively affects the release of gonadotropins, reducing their number. There are forms of secretory infertility that are not accompanied by hormonal disorders.
Causes of secretory infertility:
Varicocele. The most common cause of male infertility. Its appearance provokes varicose veins of the testicle and spermatic cord. These parts of the male reproductive system are responsible for the excretion of sperm. The result of varicocele is blood stasis, insufficient blood supply to testicular tissues, and disruption of its functioning. Factors provoking the development of pathology are an increase in the temperature of the external genital organs for a long time (visiting baths and saunas, wearing too warm trousers, synthetic underwear), vibration, as an occupational hazard (driver’s profession).
Testicular dropsy. In the scrotum, as a result of a number of reasons (for example, an inguinal hernia), an excess amount of fluid accumulates. This circumstance provokes compression of the testicle, a violation of its blood circulation, which reduces or completely stops the production of spermatozoa.
Cryptorchidism. In this violation of the development of the reproductive organs, the testicles do not descend into the scrotum, but remain in the abdominal cavity. It is diagnosed at an early age and must be treated surgically before the boy reaches the age of 7 years. If this is not done, the testicles will not be able to produce sperm due to the higher temperature inside the body than in the external environment. Even if the testicles produce a small amount of sperm, they will immediately die.
Mumps. Mumps, or mumps, is an infectious disease that affects the salivary glands. It is transmitted by airborne droplets, while the body is exposed to high intoxication. A complication of parotitis is orchitis, or inflammation of the testicles, in which the spermatogenic tissue of this organ (epithelium) is affected.
Other infectious diseases. Complications of sexually transmitted infectious diseases (syphilis, gonorrhea, chlamydia, etc.) lead to the destruction of testicular tissues, the impossibility of producing spermatozoa. Other infectious diseases (typhus, brucellosis, tuberculosis) have a similar effect, causing a toxic effect on the body and significant hyperthermia.
Hormonal disorders. With this type of infertility, spermatogenesis is disrupted due to an imbalance of testosterone and other sex hormones. The reason for this may be an excess of prolactin (hyperprolactinemia, tumor or inflammation of the pituitary gland, secondary hypogonadism. Pathologies of the endocrine system: thyroid, pancreas, adrenal glands, and obesity have a similar effect.
Genetic and hereditary diseases. There are a number of chromosomal anomalies (Shershnevsky-Turner syndrome, Klinefelter syndrome, Nuan syndrome, Kartagener syndrome), accompanied by gonadal dysgenesis, which makes a man infertile. Hereditary pathologies (polycystic kidney disease, cystic fibrosis) have a similar effect.
Injuries and tumors, testicular torsion. These causes include trauma, absence, testicular torsion, tumors of the prostate and other parts of the reproductive system.
The effect of external adverse factors. In this category are:

Side effects of drugs of certain pharmacological groups (nitrofurans, cytostatics, acetylsalicylic acid, narcotic analgesics, antibiotics, sulfonamides, hormonal preparations containing estrogens, androgens, cortisone);
Ionizing radiation;
Drinking alcohol, smoking;
Occupational hazards (exposure to lead, phosphorus, mercury, manganese compounds, ammonia, pesticides).
Hypovitaminosis adversely affects spermatogenesis, which can lead to unbalanced nutrition, starvation. Deficiency of vitamins of groups A, C, D, E disrupts potency and full spermatogenesis.
High temperatures. Visiting a sauna or a bath, cycling, wearing tight clothes or underwear made of synthetics, professions associated with staying in conditions of high ambient temperature (foundry, bakery, boiler room).
Chronic stress and age. The impact of these factors reduces the quality and motility of spermatozoa.
With one- or two-sided violation of the transport of spermatozoa through the vas deferens, we are talking about obstructive infertility.
Causes of obstructive (obstructive) infertility:
Epididymitis. The process is similar to the occurrence of obstruction of the fallopian tubes in women. Epididymitis is a complication of inflammation of the epididymis, when gluing and further obliteration of the vas deferens occurs.
Trauma and damage. Infertility occurs as a result of accidental injury during surgery on the ureters, prostate, bladder, rectum, and also as a result of trauma to the scrotum.
Tumors of the epididymis. Tissue hypertrophy as a result of the appearance of cysts and tumors leads to compression of the vas deferens.
congenital anomalies. These include hypospadias (excretion of the inflow of the urethra in the lower third of the penis), the absence of the epididymis, or the seed of the excretory canal.
Aspermatism. The essence of true aspermatism is an atypical effect of the cerebral cortex on the functioning of the reproductive centers. As a result, no semen is released during sexual contact of any duration. False aspermatism is characterized by the excretion of sperm not into the urethra, but into the bladder (retrograde ejaculation). The reason for this phenomenon is the consequences of diabetes mellitus, multiple sclerosis, inflammation of the reproductive organs, spinal cord injuries, bladder and prostate surgeries, side effects of antidepressants and tranquilizers.
Other reasons. Other causes of male infertility include:

Impotence (erectile dysfunction) – it is impossible to have a full-fledged sexual intercourse.
Premature ejaculation is the removal of semen before the penis is inserted into the vagina.
Irregular or infrequent sexual contact.
Excessively active sex life – with frequent sexual contacts with different partners, the risk of contracting STDs increases, immunity and body tone decrease, there is not enough time for the full maturation of active sperm.
Sexual illiteracy.
Psychological causes of male infertility:
Boys who grew up in a family where, as a result of authoritarian upbringing, they developed a complex of physical and mental inferiority, develop a subconscious “culling” complex in adulthood.
A man who grew up in conditions of overprotection, or in a family where his mother had unquestioned authority, often remains an infantile child who does not want to have competitors for his wife’s attention.
A man who has replaced his father in an incomplete family may have a “father complex” associated with an unwillingness to endure the difficulties associated with caring for children, subconsciously he does not want to have children.
Among the life values of a man who has raised the bar of priorities too high, there is no place for children.
Epidemiology of male infertility

Pathologies of the endocrine system – 19,8% of cases of male infertility;
Varicocele – 16%;
Extragenital pathologies, chronic diseases of the reproductive organs – 10%;
Infections – 9,7%;
Immunological factors – 4,5%;
Testicular tumors – 3%;
Idiopathic infertility (of unknown etiology) – 5%;
Other reasons – 5%.
clinical picture
There are no specific symptoms of male infertility, they depend on the cause that led to this condition. The main symptom is the absence of pregnancy in a sexual partner, which does not have any prerequisites for this in a woman. To clarify the possible factor of infertility, the woman is also examined.
If the cause of sterility is inflammation, a tumor, trauma to the male reproductive organs, manifestations of infertility can be urination disorders, pain in the scrotum and lower abdomen, one- and two-sided increase in the size of the scrotum, enlargement of the veins on her skin (with varicocele).
Hormonal disorders are manifested by gynecomastia (enlargement of the mammary glands), a decrease in sexual desire, and a decrease in the size of the testicles.
Diagnostics

Before establishing the diagnosis of “male infertility”, both spouses are offered to undergo a diagnostic examination. Couples begin their examination most often with a man. It includes the following items:
History taking. The doctor analyzes the patient’s complaints, the number of diseases and operations on the pelvic organs, possible occupational hazards and negative habits (smoking, alcohol). He will definitely be interested in the male sexual partners and the number of their pregnancies.
General inspection. The andrologist will visually assess the features of the development of secondary sexual characteristics. If the body hair is insignificant, the physique belongs to the eunuchoid type, there is gynecomastia, there is a lack of androgens. The presence of the testicles and their size are studied (normally they are approximately equal to 4,6×2,6 cm, the volume is about 18 ml), the consistency of the gonads (normally densely elastic), the condition of the veins of the spermatic cord and scrotum (varicocele is excluded). A rectal examination of the rectum is performed to exclude inflammation of the seminal vesicles and prostate.
Assessment of sexual and reproductive function. According to the patient, the doctor records in the medical history the number of sexual contacts (normally at least 2-3 per week), the quality of erection, the nature of ejaculation (normal, delayed, premature).
After the examination, the patient is sent for laboratory diagnostics. After 3 days of abstinence, he donates sperm for research.
Spermogram parameters are normal:
Ejaculate volume – 2 ml or more;
The number of spermatozoa in 1 ml is 20 million or more;
Ph-reaction – alkaline with an indicator of 7,2 or more;
Morphology – more than 30% of sperm must have the correct shape;
Motility – within an hour after ejaculation, more than 50% of spermatozoa move forward or 25% move with fast forward movements;
Viability – more than 50% of live spermatozoa;
Mar-test for the exclusion of immunological infertility – less than 50% of spermatozoa with adherent particles;
The presence of flora and agglutination – no;
Viscosity is normal;
Liquefaction – within 60 minutes;
The number of leukocytes in 1 ml is less than 1 million;
The amount of zinc is 2,4 µmol;
The amount of fructose is 13 µmol in total;
The amount of citric acid is 52 µmol in the entire ejaculate.
Possible violations:
Oligospermia – live sperm count less than 20 million per ml;
Leukospermia – an increased content of leukocytes (fixed in infections and inflammatory diseases);
Asthenozoospermia – the number of motile sperm is below normal;
Hypospermia – the volume of ejaculate is below normal;
Azoospermia – there are no spermatozoa in the ejaculate;
Polyspermia – the volume of sperm is above the norm (more than 10 ml), is recorded in the pathology of the organs of the reproductive system, with rare sexual intercourse;
Aspermia – no ejaculate, since ejaculation did not occur;
Teratozoospermia – more than half of the spermatozoa have structural defects (double head, abnormalities in the structure of the neck and tail).
If there is a suspicion of inflammatory processes in the reproductive organs or the presence of infections, the patient undergoes infectious screening:
PCR to exclude genital infections;
A smear from the urethra to determine STDs;
Sowing the ejaculate to determine the causative agent of infection (performed with an increase in the number of leukocytes);
Biochemical study of prostate secretion for glucose, alkaline phosphatase, ?-glycosidase, citric acid, zinc.
Hormonal research determines the level of the following hormones:
testosterone,
prolactin,
estradiol,
FSH and LH.
The level of free radicals in sperm cells is studied, since in the case of excessive production of reactive oxygen species, the fertilizing function of spermatozoa decreases, they become inactive, and the cell membrane of male germ cells is damaged. When studying the acrosomal reaction that occurs during the contact of the sperm with the egg, it is determined whether the sperm are able to dissolve the shell of the egg and penetrate inside. Only healthy spermatozoa with normal morphology are able to carry out specific chemical transformations on their head for such a reaction.
Microscopic examination of spermatozoa
Microscopic examination of spermatozoa using an electron microscope and cytogenetic analysis give an idea of:
About the number of chromosomes and their quality,
About the structure of the ejaculate plasma,
About a possible violation of the internal structure of the spermatozoon.
If this study reveals chromosomal abnormalities, the patient is consulted by a geneticist. A test for the detection of antisperm antibodies of class G, A, M is carried out in the diagnosis of immunological sterility. The Shuvarsky and Kutsrok-Miller tests will help identify an immune conflict at the level of the cervical canal.
Instrumental diagnosis of male infertility:
Ultrasound of the thyroid gland;
X-ray of the skull and “Turkish saddle” to exclude pituitary tumors;
Doppler ultrasound, transperitoneal ultrasound of the scrotum – for the diagnosis of varicocele, hydrocele, varicose veins of the small pelvis;
Transrectal and transabdominal ultrasound to examine the epididymis, prostate, size and structure of the testicles, detect changes in the seminal vesicles with obstruction or pathologies of the seminal ducts;
Thermography of the scrotum for the diagnosis of varicocele;
Testicular biopsy – with a refined diagnosis of idiopathic azoospermia with a normal testicle size and blood levels of FSH. The result of the study can be normospermatogenesis – there is a complete set of cells for the formation of sperm, hypospermatogenesis – an incomplete set of cells, aspermatogenesis – the complete absence of cells in the seminiferous tubules.
Vasography – x-ray of the seminal canals and vesicles to determine the focus of obstruction.
One of the methods for rapid diagnosis of infertility is a sperm chip for determining the number of spermatozoa, created by Californian scientists. It can be used at home with just a few drops of semen. The cost of the chip is about 40 €.
Male infertility test at home
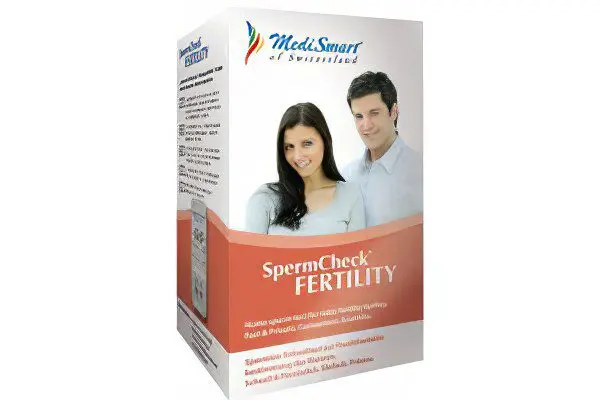
Today there is a unique opportunity to conduct a full-fledged procedure to identify infertility at home. The total cost will be about $25. It is much cheaper when compared to a full examination of the condition of the sperm, which is carried out by laboratory specialists.
The test is called SpermCheck fertility. Its developers are specialists from the University of Virginia (USA). The test was completed by a team of more than 200 male patients. Scientists claimed: the accuracy will be at least 96%. First, a variant suitable for clinical trials was released. It allowed to determine the effectiveness of vasectomy. The invention has been successfully used for a long time, since 2008.
Now anyone can carry out a procedure similar to a pregnancy test. As a result, using literally a few drops of sperm to draw conclusions about infertility. After that, you have to make a choice – whether to contact the appropriate specialists.
Normal indicators are 200-500 million spermatozoa per milliliter of semen. To draw the necessary conclusions, one must know about the criteria of the World Health Organization. According to them, infertility is obvious when this number decreases to 2 million. When the number of spermatozoa decreases to 2-20 million, the possibility of conception simultaneously decreases. The new method is built on a simple basis – the test is based on indicators – antibodies to sperm proteins. Their volume is determined by a biochemical method. Everything is done at home, close to comfortable.
Treatment of male infertility
Restorative treatment

The use of vitamins and minerals. To increase the production of steroids and improve spermatogenesis, vitamins of groups A, D, K, D, E (tocopherol) are used. Multivitamin complexes Aevit (vitamins A and E), Undevit, Gendevit, vitamin and mineral preparations Unicap, Centrum are used.
Sedatives and nootropics. Men with reduced fertility often show irritability and reduced activity, they suffer from depression and neuroses. To prevent overwork and exhaustion of the nervous system, to improve brain activity, drugs that have phosphorus in their composition (Lipocerebrin, Calcium glycerophosphate) are used. Bromine preparations, extracts of valerian, motherwort, tincture of Eleutherococcus are recommended as sedatives. More pronounced disorders of the central nervous system (psychological infertility) require the use of an individual treatment plan involving a neurologist and a psychotherapist.
Hepatoprotectors. These are drugs that improve liver function: Karsil, Hofitol, Methionine, Essentiale-Forte, Heptral, Ovesol. At the same time, it is advisable to follow diet No. 5 (according to Pevzner), which provides for a restriction in the diet of marinades, pickles, fatty foods, and the use of seasonings.
Biostimulants. To improve metabolism, activate the activity of the reproductive organs, normalize their blood supply, accelerate the regeneration of tissues and organs, biostimulants are used: aloe extract, Apilak, vitreous, FiBS, Splenin, Methyluracil, Pentoxyl.
Treatment of secretory infertility in men

Primary hypogonadism. For the treatment of primary (hypergonadotropic gonadism), androgens are used. Their function is to stimulate spermatogenesis and inhibit the production of gonadotropins FSH and LH. These are testosterone, methyltestosterone, etc. If the reserve androgenic functions of the testicles are preserved, the drugs are taken for 2-3 months. This is followed by a break for the same time, during which the luteinizing hormone choriogonin is taken.
To increase the number of spermatozoa and increase their mobility, androgens (Andriol, Proviron) are taken in minimal doses. Underweight men are recommended to take anabolic hormones (retabolil, nerobol).
To improve spermogram parameters, activate the pituitary gland, and improve spermatogenesis, replacement therapy with drugs containing long-acting testosterone (testenat) is used. Cancellation of the drug after a two-month course gives the opposite effect with a predictable reaction of the body.
With hyperlactinemia, prolactin production inhibitors (bromocriptine) are used to increase libido, stimulate potency, improve spermogram parameters, and also for the treatment of gynecomastia.
Secondary hypogonadism. With a lack of luteinizing hormone, testosterone synthesis decreases, spermatogenesis slows down. For the treatment of this condition, LH preparations (pregnal, choriogonin) are used for 1,5-2 months, combining them with testosterone. If there is not enough FSH, folistamine or anthrogon is prescribed to activate spermatogenesis for 1.5-2 months.
To stimulate the activity of the pituitary and hypothalamus, progestins (clomiphene) or antiestrogens (tamoxifen, zitosonium) are prescribed, the course intake (a month with a 10-day break) can be repeated up to 6 times.
Treatment of excretory infertility in men
Treatment of this type of male sterility begins with the correction of the cause that caused this condition. If infertility is caused by complications of prostatitis, vesiculitis, orchitis, urethritis, treatment with antibiotics and anti-inflammatory drugs is prescribed. Additionally, massage, physiotherapy, acupuncture and other methods are used. To normalize metabolism and stimulate spermatogenesis, hepatoprotectors, adaptogens, biostimulants, and vitamins are prescribed.
Surgical treatment of male infertility

Surgical intervention is indicated for obstructive aspermia.
The tactics of the operation to restore the patency of the seminal ducts depends on the structure of the pathology:
Vasovasostomy (the site of obstruction of the vas deferens is removed);
Vasoepididymostomy (vas deferens are connected to the tubules of the appendages);
Resection of the prostate through the urethra.
The age category for such operations is young men (under 30 years old).
If aspermia is diagnosed in older men, other methods of sperm retrieval are used for assisted fertilization technologies:
Percutaneous testicular puncture;
Percutaneous puncture of the epididymis;
Open puncture biopsy of the gonads;
Microsurgical intervention to obtain the contents of the epididymis.
With secretory infertility, the following surgical intervention is performed:
Embolization or sclerotherapy of the affected ovarian vein (with varicocele);
Puncture or sclerosing (with dropsy of the testicle);
Laparoscopy or the use of the classical method (with cryptorchidism, performed in childhood).
Treatment methods for autoimmune infertility:
Therapy with glucocorticoids (Hydrocortisone, Desamethosone) with anti-inflammatory, immunosuppressive and antihistamine effects, forms of application – tablets, ointments, physiotherapy.
Sperm capacitation (treatment and washing) in preparation for IVF or ICSI.
Assisted Reproductive Technologies
Alternative methods of male infertility compensation:
Artificial insemination. The essence of the method is as follows – pre-treated sperm is introduced into the cervical canal of a woman or directly into the uterine cavity. In cases of low concentration of active sperm in the sperm of the spouse or their complete absence, donor sperm is used. The method is used for cervical factor (production of antibodies to the spermatozoa of the spouse by the mucus of the cervical canal), with autoimmune infertility and sterility of unexplained etiology.
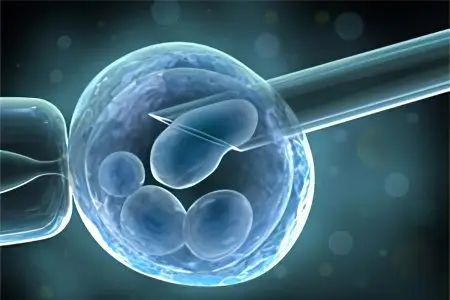
In vitro fertilization. In IVF, the fertilization of the egg takes place outside the female body. Several copies are removed after artificial stimulation of ovulation from the ovaries, in a Petri dish they are fertilized with the sperm of their spouse. A few days later, the most viable zygotes (fertilized eggs) are selected and transferred to the uterus.
ICSI. The ICSI method (intracytoplasmic sperm injection) is the introduction of the sperm into the egg using microsurgical manipulations. For the success of the procedure, one viable spermatozoon is enough. Male cells are obtained by masturbation or surgical aspiration.
Surrogacy or adoption. In the case of donor motherhood, the surrogate mother, within the framework of a previously concluded agreement, bears a child that develops from a zygote obtained from the germ cells of infertile spouses.
General recommendations

There are simple rules, following which you can significantly improve the quality of sperm. These recommendations are especially relevant for men planning the appearance of a child in the family.
Following the principles of healthy eating. It is advisable to limit the use of marinades, pickles, smoked meats, sweets, hot spices, fatty foods. Recommended products: red meat, legumes, walnuts, parsley, dill, basil, celery, fresh fruits and vegetables in large quantities, rosehip decoction or infusion. It is very useful to eat a tomato in any form due to the high content of such an antioxidant as lycopene.
Normalization of body weight and prevention of hypodynamia. A sedentary lifestyle provokes stagnation of blood in the pelvic organs. The consequence of this is a deterioration in the quality of sperm, a decrease in potency, the development of diseases such as varicose veins, hemorrhoids, dropsy of the testicle. An increase in body weight contributes to increased production of estrogen, a female hormone, by adipose tissue. Physical education, walking, and performing gymnastic complexes will help reduce this risk.
Wearing physiologically healthy underwear and clothing. In order not to disturb the blood circulation in the pelvic organs, in the scrotum, it is advisable to refuse to wear tight underwear (especially if it is made of synthetics), tight jeans.
Normalization of the regime of sexual life. Normally, sexual intercourse should be at least and not more often than once every 2-3 days. The result of too frequent contacts may be the production of sperm with a large number of immature spermatozoa, too rare – the aging of male germ cells. In addition, regular sexual intercourse protects a man from the appearance of prostatitis and prostate adenoma.
Prevention of overheating of the reproductive organs. Temporarily it is worth refusing to visit the sauna and bath.
The use of folk remedies. An excellent effect in the treatment of infertility is the use of bee products: bee pollen (pollen from bee honeycombs), flower pollen, honey, royal jelly. The norm for the use of flower pollen and bee bread is 1/2 tsp. in a day. Medicinal plants are used to normalize blood circulation in the pelvic organs, increase testosterone secretion and sperm quality. Plantain, Ivan tea, sage, knotweed are brewed and taken 3-4 tbsp. l. in a day.
Treatment of male infertility, its duration and effectiveness depends on the cause of the pathology, the thoroughness of following the recommendations of specialists, the chosen methods of therapy. About 45-50% of couples whose infertility is “guilty” of a man, as a result of treatment, find the happiness of being parents.









