Contents
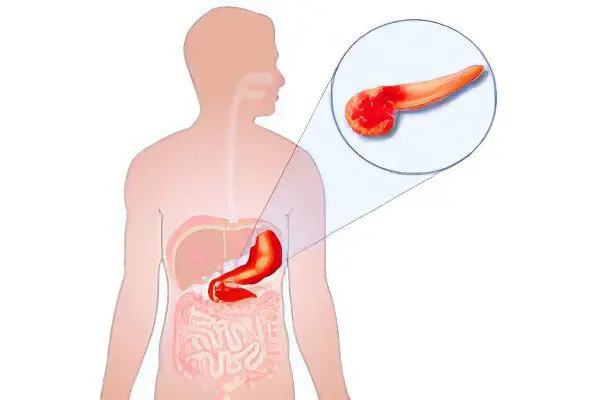
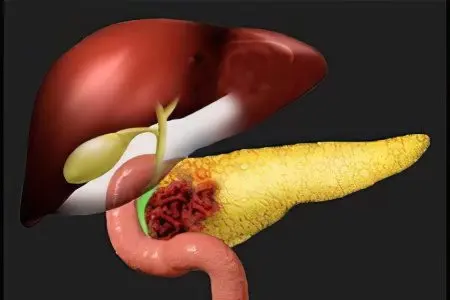
The pancreas is one of the most important secretory organs of the human body and plays a significant role in metabolic and digestive processes. The most common diseases associated with this organ are pancreatitis, pancreatic necrosis, cancer, cyst and diabetes. You will learn about the symptoms and methods for diagnosing all the major diseases of the pancreas below.
Acute pancreatitis
Acute inflammation of the pancreas is called acute pancreatitis.
Causes
About 70% of cases of acute pancreatitis are associated with alcohol addiction and alcohol poisoning.
Other causes of the development of the disease:
Improper nutrition (fatty foods, overeating);
Cholelithiasis;
Heredity;
Damage to the pancreas (surgery, accident);
Taking medications in toxic doses;
endocrine diseases;
Infections (hepatitis virus, mycoplasmosis).
Symptoms
The main symptom indicating acute pancreatitis is “drilling” pain. It begins in the epigastric zone, hypochondria (right and left), is able to take on a girdle character, capture the back, lower and lateral parts of the abdomen.
There are other manifestations:
Frequent vomiting causing dehydration;
Dry mouth, belching;
Increased body temperature (may reach 40 ° C);
Cardiopalmus;
drop in blood pressure;
Bloating and soreness of the abdomen;
Sudden weight loss;
Diarrhea.
Methods of diagnosis
Detection of acute pancreatitis is a difficult task, especially if the disease is in its early stages.
The diagnostic complex consists of the following studies and analyses:
General blood analysis. Allows you to find signs of an inflammatory process (for example, an increase in the number of leukocytes);
Blood chemistry. Sets an excessive concentration of the enzyme amylase (indicates the development of the disease);
Abdominal ultrasound. Detects changes in the pancreas and nearby organs. If gallstones are the cause of the disease, ultrasound helps to determine their location;
Analysis of urine. Detects amylase in the urine, confirming the presence of pancreatitis in the patient;
EGDS. Assesses the degree of involvement of the stomach in the inflammatory process.
Chronic pancreatitis

The development of chronic pancreatitis occurs as a result of a protracted inflammatory process occurring in the pancreas. Men over 40 are most susceptible to the disease, but in recent years there has been an increase in cases of chronic pancreatitis in women and in younger people.
Causes
The most common causes are the presence of gallstone disease in a patient and excessive consumption of alcoholic beverages.
Symptoms
Pain in chronic pancreatitis has a cutting character, the patient feels constant pressure in the affected area. The intensity of the pain increases if the patient does not adhere to a diet, eats fatty foods and carbonated drinks, and drinks alcohol.
Other symptoms of chronic pancreatitis are belching, vomiting, bloating, stool disorders (thick, profuse stools), lack of appetite. Also characterized by weight loss, despite the preservation of the usual diet.
Methods of diagnosis
As part of the diagnosis of chronic pancreatitis, the following studies and analyzes may be prescribed to the patient:
Blood analysis. With an exacerbation of chronic pancreatitis, an increased concentration of leukocytes in the blood is observed, the erythrocyte sedimentation rate increases, the amylase index increases (it is also detected in the urine);
ultrasound. The enlargement of the gland (full or partial), the correspondence of the size of the head, tail and body to the norm, the evenness of the contours are evaluated;
CT. Tomography establishes the foci of the disease and the presence of stones in the ducts.
Pancreatic necrosis
Approximately 20% of patients with acute pancreatitis have a severe course of the disease, against the background of which changes in the pancreatic parenchyma occur, which have a degenerative-destructive character. Pancreatic necrosis is more common at a young age, women are most susceptible to it.
Causes
Pancreatic necrosis can develop due to the following reasons:
Cholelithiasis, cholecystitis;
Improper nutrition (an abundance of carbohydrates and fats, overeating);
Complications after surgery;
Alcohol abuse, which destroys pancreatic tissue;
A number of infectious diseases (mononucleosis, parotitis).
Approximately 10% of patients cannot determine the cause of pancreatic necrosis.
Symptoms
The disease is characterized by the rapid development and rapid increase in symptoms:
Sharp pain, concentrating in the upper abdomen and having a girdle character. Pain on palpation of the affected area;
Repeated vomiting, bouts of nausea, constant dry mouth;
The formation of cyanosis spots on the abdominal wall, hyperemic skin of the face;
Attacks of tachycardia, persistence of shortness of breath even at rest;
The patient feels constant anxiety and tension, suffers from chronic weakness.
Methods of diagnosis
For the diagnosis of pancreatic necrosis, the same studies and analyzes are used as in pancreatitis.
Pancreas cancer
A rare disease characterized by the formation of malignant cells in the tissues of the pancreas is cancer.
Causes
Factors contributing to the occurrence of pancreatic cancer may include the following:
Cigarettes. The risk of developing the disease for smokers is about twice as high. The factor is characterized by reversibility, timely refusal of cigarettes reduces the risk of cancer;
Age. At risk are people who have crossed the threshold of 60 years;
Floor. The predisposition to pancreatic cancer is higher in men than in women. Some doctors attribute this to a lower percentage of women who smoke, but the hypothesis has not received evidence;
Obesity. Excess weight favors the development of pancreatic cancer;
Chronic diseases. Among them, pancreatitis and diabetes mellitus pose the greatest threat;
Unhealthy food. The threat of cancer is increased if a person’s diet contains an excess of animal fats and simple carbohydrates;
genetic factor. The presence in the pedigree of cases of pancreatic cancer should be the reason for a more attentive attitude to one’s health.
Symptoms
Among the main manifestations with which pancreatic cancer makes itself felt are the following:
Pain that is concentrated in the upper abdomen and radiates to the back. The pain is acute, girdle character;
Weight loss. Weight decreases, despite the preservation of eating habits;
Dry mouth, intense thirst;
Vomiting due to the squeezing effect of the tumor formation;
Jaundice. Yellowing of the skin and mucous membranes is possible. The symptom is associated with a violation of the outflow of bile, sometimes jaundice is accompanied by skin itching;
Feeling of heaviness in the area of the right hypochondrium. The symptom is associated with compression of the splenic vein;
Chair disorders. Lack of enzymes and poor absorption of fats lead to liquid, fatty stools, characterized by a pungent odor.
Methods of diagnosis
After a physical examination of the patient, the doctor may order the following tests and examinations:
ultrasound. Ultrasound examination of the abdominal cavity is indicated for jaundice and pain in the upper abdomen. Ultrasound can detect a tumor formation;
CT. Computed tomography reveals even microscopic tumors that go unnoticed during an ultrasound examination;
Biopsy. A tumor site is taken for analysis, the results of which confirm the benign or malignant nature of the neoplasm;
Blood analysis. Conducting a study is necessary to assess the level of concentration in the body of the CA19-9 antigen;
To accurately determine the stage at which pancreatic cancer is located, additional studies are prescribed – chest x-ray, liver ultrasound, and others.
pancreatic cyst
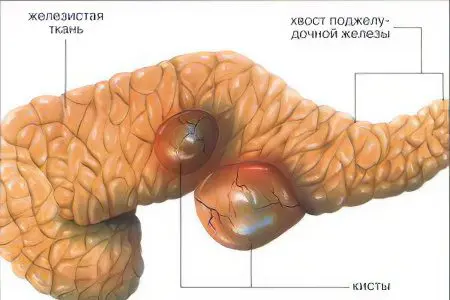
A fluid vesicle localized in the pancreatic parenchyma or nearby tissues is called a cyst.
Causes
A pancreatic cyst can be acquired or congenital. Congenital formations are associated with pathologies of tissue development.
Acquired cysts appear due to the following reasons:
Damage to the pancreas (surgery, accident);
Chronic or acute pancreatitis;
benign tumor;
malignant tumor;
parasitic infection;
An excess of cholesterol in the blood.
Factors favoring the formation of cysts are overeating, a large amount of fatty foods, excessive alcohol consumption, and chronic stress.
Symptoms
Symptoms of a pancreatic cyst are directly related to the location and size of the cavity. Signs of the disease may be absent if the size of the formation does not exceed 2 cm.
Larger capsules declare themselves with the following manifestations:
Pain that occurs in the area of the left or right hypochondrium. The pain can spread to the navel and radiate under the shoulder blade. In some cases, the pain takes on a girdle character. The intensity is determined by the onset of complications;
Seal, formed in the area of the abdominal cavity, which is easily detected by palpation. The swelling gradually increases in size;
Jaundice, which is the result of squeezing nearby organs and worsening the outflow of bile;
Indigestion, nausea and vomiting, alternating constipation and diarrhea;
Change in color of urine and feces;
Rapid weight loss associated with impaired bowel function;
Constant feeling of weakness and malaise.
If an infection joins the cyst, symptoms include fever, chills, headaches, and muscle pain.
Methods of diagnosis
Diagnosis of a pancreatic cyst begins with palpation, which reveals a bulge located in the upper abdomen.
The following diagnostic tools are also used:
ultrasound. The study reveals the presence of a neoplasm with reduced echogenicity, characterized by evenness of contours and roundness of forms;
Endoscopic ultrasound. Diagnoses a cyst and establishes its nature, on which treatment depends;
X-ray with the use of contrast agents. Determines the displacement of the stomach, which occurred under the influence of the cyst;
CT. Differentiates false and true cysts.
Diabetes
The development of diabetes in a patient is due to a violation of the production of insulin by the pancreas and the accumulation of sugar in the blood.
Causes
Genetic predisposition is considered a major factor in the development of diabetes in humans.
The following reasons are also possible:
Obesity. Persons with a genetic predisposition to diabetes should first of all keep their weight under control;
Diseases and injuries of the pancreas;
Emotional overstrain, a state of chronic stress;
Viral infections (flu, rubella);
Age. The elderly are most susceptible to the disease.
Symptoms
Diabetes mellitus can inform about itself by the following manifestations:
Frequent urination;
Constant feeling of hunger;
Sharp weight loss (if it cannot be explained by food restrictions);
Increased dryness of the skin, itching;
Numbness in the legs and arms;
Vomiting, nausea;
Pain in the abdomen;
Deterioration of vision;
Susceptibility to infections, poor wound healing.
Diagnostics
To diagnose diabetes, the doctor conducts a sugar test, a blood test for glucose, and a urine test. If necessary, other diagnostic methods are connected.
Diseases of the pancreas pose a threat to the life and health of the patient, are fraught with dangerous complications. If you find any of the above symptoms, be sure to visit a doctor.









