Contents
Xerostomia, or dry mouth, can occur in two forms: true and pseudo-xerostomia. The first form is caused by the low secretory activity of the salivary glands, while the second is a disorder of the vegetative nervous system characterized by dryness and burning sensation in the mouth.
What is xerostomia and what are its types?
Xerostomia are symptoms of dry mouth that are subjective in nature. It is generally manifested by a reduced production of saliva by the salivary glands. This ailment may appear as a consequence of medication or constant stress. Saliva is very important to our body because it moisturizes the oral cavity and thus allows better swallowing and digestion of the food we eat. In addition, saliva supposedly leaches food debris from our teeth. Its deficiency for a longer period of time is called xerostomia. Xerostomy is not a dry mouth that occurs on hot days. It is estimated that about 10 percent. of the population suffers from xerostomia, including 25 percent. people who are 65 years of age or older. We divide xerostomia into two types: true and pseudo.
True xerostomia
it is the result of a decrease in the secretory activity of the salivary glands. In more advanced stages, it may be accompanied by atrophy of the oral mucosa.
Pseudo-xerostomia is a disorder of the vegetative nervous system, consisting in the feeling of dryness and burning sensation in the mouth, despite the proper function of the salivary glands.
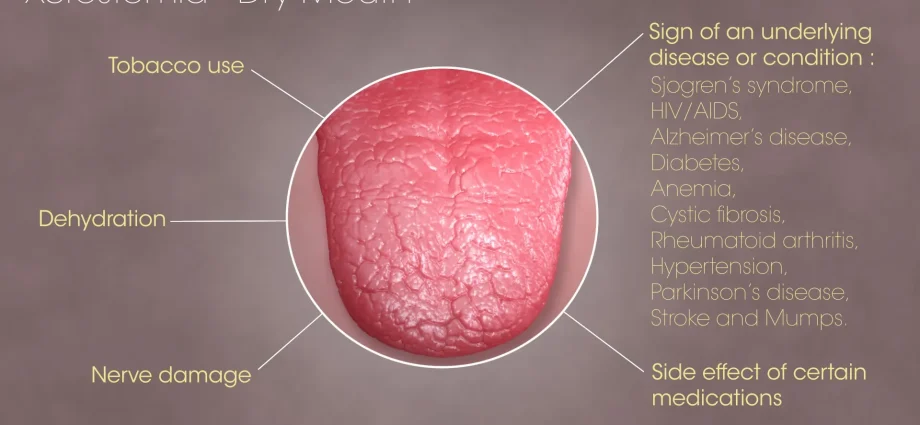
Xerostomia – causes
Xerostomia may be the primary condition or manifestation of a systemic disorder. Her appearance occurs, inter alia, as a result:
- the use of certain medications (including diuretics, antidepressants and anxiolytics, lowering blood pressure, antihistamines, cytostatics, some antibiotics and many others)
- overactive thyroid gland
- diabetes
- sarkoidozy
- amyloidozy
- deficiency of B vitamins
- microcytic anemia and iron deficiency
- AIDS
- some tumors of the central nervous system
- anxiety and depression
- certain connective tissue diseases
- oral mycosis
- certain allergic diseases
- dehydration
- radiotherapy of the head and neck area
- smoking
- psychogenic states (anxiety, endogenous depression)
- complete use of dentures
- mouth breathing.
Not so long ago, the patient’s age (advanced) was considered the main cause of xerostomia. It has been proven, however, that this type of ailment in elderly people is not only related to age, but also to the medications they take and the accompanying systemic ailments.
Xerostomia — pathogenesis
Impaired salivation increases the accumulation of plaque and caries. It has been proven that the saliva of people with xerostomia, which results from the medications taken, despite the proper concentration of protein saliva, differs significantly from the number and composition of microorganisms from the saliva of healthy people. In the saliva of people who took the medications, an increased number of microorganisms was demonstrated with a reduced proportion of α-haemolytic streptococci and an increase in the proportion of anaerobic bacteria.
Xerostomia – symptoms
In addition to dry mouth and its consequences (burning, difficult talking and eating, taste disturbances), the effects of xerostomia are also an increased susceptibility to oral infections (especially fungal infections) and the occurrence of ulcerations and atrophy of the mucosa. Due to the lack of neutralizing effect of saliva on acids formed in the mouth, people with xerostomia are also much more predisposed to the occurrence of caries. Physical examination of the patient shows the presence of a white and dry oral mucosa. Moreover, the patient’s tongue is cracked and inflamed, without warts; there are symptoms suggesting inflammation of the corners of the mouth or oral mucosa. The main disease changes are accompanied by:
- caries,
- oral candidiasis,
- greater predisposition to mouth ulcers,
- bad smell from the mouth,
- problems with the proper sense of taste,
- burning of the tongue and lip,
- change in the color of the lining of the mouth.
The above symptoms make everyday functioning very difficult. Patients have difficulties both speaking and using dentures. Often there is also a loss of appetite, and thus less fluid and food intake, which causes dehydration and exhaustion of the body
Diagnostics of xerostomia
Diagnosing true xerostomia involves not only assessing the symptoms present, but also carrying out sialometric tests. The conducted research concerns mainly:
- assessment of the level of secretion from the parotid glands,
- assessment of the level of unstimulated saliva,
- assessment of the amount of stimulated saliva,
- assessment of the secretion level of the palate glands.
Medical history, imaging tests and salivary gland biopsy are also important in the diagnosis of xerostomia.
Treatment of xerostomia
Treatment of xerostomia is primarily the therapy of the disease that causes it. Additionally, preparations that stimulate the secretion of saliva or its substitutes are used. Due to the increased susceptibility to diseases of the teeth and oral mucosa, patients with xerostomia should undergo regular dental check-ups.
Taking into account the fact that the causes of xerostomia are the most frequently taken preparation and their mutual interactions, it is often sufficient to change or abandon certain medications. The most important thing in causal treatment is:
1. administering to the patient preparations stimulating salivation, such as: a) acetylcholinesterase inhibitors, e.g. neostigmine, physostigmine; b) drugs that stimulate the secretion of bile e.g. anethole trithione; c) direct cholinomimetics, e.g. pilocarpine – prescribed in patients after radiotherapy of head and neck tumors, supports and promotes the regeneration of the functions of the palate glands,
2.physical exercise,
3.treatment of menopause,
4. intensive chewing gums / lozenges without sugar.
Sometimes the only treatment option is symptomatic therapy, which does not affect salivation but relieves the symptoms of the disease. The treatment methods include:
- the use of cute substitutes, whose task is to moisturize and soften the mucosa, e.g. mouthwash, mucin in combination with electrolytes or xylitol, lozenges, special sprays (Glandosane Spray – methylcellulose);
- consumption of cow’s milk, which not only nourishes and moisturizes, but also promotes remineralization of the enamel;
- drinking small amounts of water, but often;
- treatment of any fungal diseases in the oral cavity;
- rinsing the mouth with linseed;
- implementation of caries prophylaxis including: a sugar-free diet, personal oral hygiene, mouth rinsing with chlorhexidine.
Text: SzB
The content of the medTvoiLokony website is intended to improve, not replace, the contact between the Website User and their doctor. The website is intended for informational and educational purposes only. Before following the specialist knowledge, in particular medical advice, contained on our Website, you must consult a doctor. The Administrator does not bear any consequences resulting from the use of information contained on the Website.