Contents
Blood in the stool is a symptom of a large number of fairly serious diseases. Sometimes this is the only sign of trouble, but more often the appearance of bloody inclusions is accompanied by other manifestations that are not typical for the body in the norm. By comparing all the symptoms, the doctor will be able to determine the root cause of the alarming sign.
Bleeding in the gastrointestinal tract is the most common cause of blood in the stool. The length of the digestive tract is about 10 m, its mucous membrane is saturated with bacteria that can modify the type of blood we are used to. For these reasons, it rarely ends up in the feces unchanged. Fresh blood in them can be detected only when the source of bleeding is located near the anus. Most often, the localization of bleeding is the rectum or the lower sections of the large intestine. When bleeding from the upper parts of the digestive tract, the color of the blood in the feces changes, it becomes dark brown or black (melena).
With hemorrhoids, a malignant tumor of the lower intestines, an anal fissure, traces of blood appear not only in the feces, but also on toilet paper, on underwear. If bloody inclusions look like dark red clots or veins, this is a symptom of a chronic intestinal disease: ulcerative colitis, dysbacteriosis, Crohn’s disease. If, with diarrhea with bloody inclusions, the patient has significant hyperthermia, the stomach hurts, there is an intestinal infection (dysentery, salmonellosis).
Occult blood in the stool, a sign of serious gastrointestinal disease, cannot be seen. If occult blood is suspected, a special analysis is prescribed. The reason for a false alarm can give the use of beets, blueberries, currants, tomatoes. The products of their processing are similar to inclusions of blood in feces.
When blood appears in the feces, products that change the color of feces should be excluded from the diet for 2-3 days. If the alarm symptom persists, you should immediately consult a doctor. Pharmaceutical preparations – activated charcoal, iron preparations – can radically change the color of the stool.
Bright red, unclotting blood | The patient detects blood not only in the feces, but also on underwear, on toilet paper after defecation, the cause is bleeding due to an anal fissure, rectal tumor, internal hemorrhoids |
Diarrhea with bloody inclusions, hyperthermia | Intestinal infections – dysentery, salmonellosis |
Dark red blood clots or streaks | Inflammation of the upper intestines – ulcerative colitis, Crohn’s disease, dysbacteriosis |
Occult blood test positive | Colon polyps or cancer, complications of helminthic invasion, malignant tumors of the stomach, esophagus, rectum |
If blood is seen in the stool – the reasons

Fissures in the anus. Bright scarlet blood, not mixed with feces, is a symptom of an anal fissure. It is formed in chronic constipation, when the patient makes excessive muscular efforts during bowel movements. After the feces have left the rectal ampulla, there is a slight discomfort in the area of the anal fissure. Blood in the feces with this pathology is observed for several days, its volume is quite small.
It is possible to make a diagnosis with a visual examination by a surgeon or proctologist, as well as with a digital examination of the preanal region. Correction – the restoration of regular stools with the help of diet and the use of laxatives. Additionally, Anuzol or suppositories with sea buckthorn oil are used for 5-7 days.
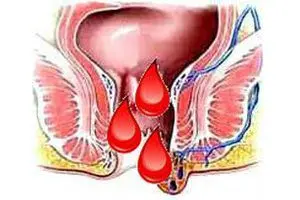
Hemorrhoids. Dark blood in the stool, regularly appearing on its surface, pain and itching in the rectum, accompanied by a feeling of fullness – symptoms indicating hemorrhoids (varicose veins of the rectum). There are a lot of reasons for the appearance of hemorrhoids, all of them are associated with an overstrain of intra-abdominal pressure, stretching. Damage to the vascular walls causes bleeding.
With external hemorrhoids, varicose nodes are visible during visual examination, with internal hemorrhoids, they are detected during sigmoidoscopy of the rectum. Treatment of hemorrhoids includes conservative therapy and surgical intervention. Therapy with drugs is used in the early stages of the disease. These are venotonics in the form of tablets (Troxerutin, Detralex, Ginkor forte, Venoruton, Venolan), drops and dragees (Aescusan), ointments and gels (Troxevasin, Antistax, Venitan), venosclerosing agents (Hepatrombin G in the form of suppositories, Ethoxysclerol). Additionally, NSAIDs, anticoagulants and laxatives are used.
The operation to remove hemorrhoids is carried out in advanced cases, at a late stage of the disease, or in emergency cases – with heavy bleeding from the venous hemorrhoid.
Nonspecific ulcerative colitis. This disease is the result of inflammation of the immune nature. In ulcerative colitis, destructive processes are observed in the mucosa and submucosa of the rectum and colon. Blood in the feces is not the only evidence of the disease; pus and mucus in the feces, abdominal pain, diarrhea, hyperthermia, symptoms of intoxication of the body appear against the background of intestinal inflammation. Complications of the pathology – peritonitis, intestinal perforation with bleeding, intestinal obstruction.
The diagnosis is made after FGDS and examination of intestinal tissues for histology. Treatment of ulcerative colitis is therapy with glucocorticosteroids, cytostatics and sulfalazine. Emergency surgery is indicated for complicated colitis.

Crohn’s disease. The disease is inherited or occurs as a result of inflammation of the immune nature. It develops in all parts of the digestive system as a complication of measles, food allergies, smoking or stress. It most commonly occurs in the colon and small intestine.
Symptoms of Crohn’s disease – frequent diarrhea, pus, mucus and blood in the stool, pain in the abdomen and joints, skin rash, fever, ulcers on the oral mucosa, decreased visual acuity. Diagnosis – FGDS and histological examination of tissues. Treatment of the disease – therapy with the use of Ciprofloxacin, Metasalazine, Metronidazole.
Intestinal infections. Blood in the feces can appear when pathogens of acute intestinal infections enter the body, caused by:
Viruses (enterovirus, rotavirus);
Bacteria (staphylococcus, salmonella, klebsiella, paratyphoid and dysentery bacilli, campylobacter);
Parasites (amoebiasis, schistosomiasis).
The consequence of these infections is the defeat of the small (enteritis) and large intestine (colitis).
Symptoms of infection – loose stools containing pus, mucus and blood in the stool, fever. With viral Omsk, Crimean and Central Asian hemorrhagic fevers, small vessels are affected. This leads to the appearance of a hemorrhagic rash on the skin and intestinal bleeding. When the large intestine is affected by cytomegalovirus, diarrhea with blood, fever and pain in the projection of the intestine are noted.
Diagnosis of infections – bacteriological culture of feces, microscopic and serological examination of blood to detect antigens to pathogens. Treatment of bacterial infections in the acute stage – therapy with Cephalosporin, Furazolidone, Enterofuril, Ciprofloxacin, probiotics. Treatment of viral intestinal infections – Arbidol, interferons (Viferon, Kipferon). Anthelmintic therapy – Tinidazole, Metronidazole, Praziquantel (for schistosomiasis).
Tumors of different parts of the intestine. Symptoms of an oncological lesion are intestinal obstruction, blood in the feces when the intestinal wall or blood vessels are destroyed, perforation with fecal peritonitis. Diagnosis – total x-ray examination of the abdominal cavity (symptom of gas bubbles, “Cloiber’s bowl”). Treatment – resection of part of the intestine, coagulation of the affected vessels or their suturing.
Dysbacteriosis. An alternative name is excessive bacterial colonization of the intestine. Dysbacteriosis provokes the use of antibiotics. Blood in the feces with this pathology appears when the intestinal mucosa is affected by Clostridium. Treatment – Metronidazole, Bactrim, Vancomycin.
STI. This abbreviation stands for sexually transmitted infections – rectal gonorrhea, anorectal syphilis, herpes, venereal granuloma. Symptoms – blood in the stool, or on its surface due to a violation of the integrity of the intestinal mucosa.
If infections are complicated by atherosclerotic damage to the arteries, ischemic colitis develops (oxygen starvation of one of the sections of the large intestine). Symptoms of ischemic colitis are acute pain in the intestinal area, bleeding due to erosion of the intestinal wall. First aid, it is also express diagnostics, is the intake of Nitroglycerin. With ischemia, it perfectly relieves pain.
Causes of occult blood in the stool

Blood in the stool from the upper gastrointestinal tract usually has a slightly different appearance. The reason for this is the breakdown of hemoglobin, its conversion into iron sulfate. As a result of this biochemical reaction, the blood acquires a black color, such a stool is called “melena”.
Bleeding from varicose veins of the esophagus. It is part of the portal hypertension syndrome that occurs with cirrhosis of the liver. Additional symptoms are tar-colored stools, retrosternal pain after eating, vomiting with blood, hypotension, palpitations, cold sweats, bitterness in the mouth, spider veins on the abdomen. The first emergency aid for ruptured varicose veins of the esophagus is the introduction of a balloon probe into it to stop the bleeding, squeezing the veins.
Mallory-Weiss syndrome. Manifestations of the syndrome are a deep bleeding defect in the mucous membrane of the esophagus or the cardia of the stomach, reaching the submucosa. It most often occurs during repeated vomiting in patients with perforated gastric ulcers or those suffering from alcoholism. The main symptoms are tar-black blood in the stool and severe pain. Treatment – bed rest, aminocaproic acid and Cerucal intramuscularly.
Bleeding from a stomach or duodenal ulcer. Symptoms – tar-black blood in the stool, acquiring a liquid consistency, nausea and vomiting with blood (“coffee grounds”), fainting, chills. Treatment – resection of the stomach or duodenum, possibly suturing the ulcer.
Perforation of duodenal ulcer. Complication – symmetrical ulcers on the opposite side of the intestine. Symptoms – acute pain of a dagger character on the right, loss of consciousness, cold sweat, chills, weakness, tachycardia. Emergency care – urgent laparotomy with resection of the duodenum 12.
Stomach cancer. Symptoms – aversion to food, especially meat, rapid satiety, anemia, weakness, sudden weight loss, bleeding as a result of tissue breakdown.
Bowel cancer. Symptoms – alternating diarrhea and constipation, rumbling in the intestines, false urge to empty, defecation that does not bring relief. There is a ribbon-like feces with an admixture of blood in the later stages of the disease, intestinal obstruction.
Tumors of the esophagus. Symptoms are similar, tissue breakdown causes bleeding and melena.
Intestinal tuberculosis
Stomatitis, periodontitis
Nose bleed
Blood in the feces can appear as a result of poisoning with rat poison or poisonous plants (clover, euonymus). Bleeding is possible – the result of a reduced function of blood clotting of a hereditary nature or side effects of drugs: NSAIDs (Aspirin, Diclofenac, Heparin, Xarepta). The appearance of blood during bowel movements while taking medication is a reason for discontinuing the drug and consulting a doctor.
Diagnosis of occult blood in the stool

With minimal blood loss during tooth extraction, wounds and ulcers in the mouth, minor bleeding in the digestive system, blood in the feces may not be visually noticeable. To verify its presence, a laboratory test called the “Gregersen reaction” is carried out.
For maximum reliability of the analysis, the patient should not eat meat, fish, brush his teeth, take iron preparations 3 days before it. The feces collected after preparation are treated with a solution of reagents in acetic acid, and the color change of the preparation is analyzed. If it turns blue or green, the test for occult blood is considered positive.
Causes of the presence of blood in the stool in a child

In childhood, almost all the pathologies of the digestive system described above are diagnosed, so blood in the feces in children can appear for the same reasons as in adults. However, in pediatric practice there are specific causes that are unique to childhood.
Dysbacteriosis. Malnutrition in infants, unjustified antibiotic treatment, weak immune defenses can lead to the following symptoms: bloating, mucus and blood in the stool, diarrhea, diathesis, decreased appetite. The reason for this is enterocolitis caused by staphylococcus or Klebsiella.
Differential diagnosis from helminthiases and acute intestinal infections with similar symptoms is carried out. Treatment of infants – bacteriophages according to the type of pathogen, children older than a year – Enterofuril. After the control analysis, a course of probiotics is carried out (Linex, Bifilux, Bifiform, Normoflorin, Bifikol).
In addition, children are offered an additional volume of liquid and a prophylactic dose of vitamin D. The consistency of the stool is regulated by diet, the use of Lactulose, Normaze, Dufalac, suppositories with sea buckthorn oil.
Intestinal obstruction. The most dangerous prerequisites for the fact that children under two years old have blood in the feces are intestinal obstruction or intussusception of the intestine. The reason for these conditions is a congenital anomaly in the development of the intestinal tube, overfeeding the child, feeding too early, changing the usual milk formula. Invagination – overlapping of the intestinal lumen with another part of it. This results in intestinal obstruction.
It all starts with anxiety and a strong cry of the baby after feeding, gushing vomiting. Then there is frequent loose stools and blood in the stool. This condition quickly worsens, within a few hours the child begins to defecate red mucus. Delay in medical attention leads to shock or collapse, which ends in death.
Diagnosis – plain x-ray or ultrasound of the abdominal cavity. In children under one year old, surgery can be avoided by giving a barium enema. In children older than a year, the condition is treated by performing a laparotomy.

Food allergy. Types of food allergies:
For cow’s milk protein
for citrus fruits,
on gluten,
For food additives, food colorings, flavorings.
Allergy symptoms – diarrhea, frothy stools, blood in the stool in the form of streaks, spotting, tearfulness, restless behavior, insufficient weight gain. If these symptoms appear, you should contact your pediatrician.
Immediate medical attention is required if children are diagnosed with the following symptoms:
hyperthermia,
Vomiting, regurgitation in the form of a fountain,
Frequent loose stools
Excessive excitement or inhibition of behavior.
With such manifestations, treatment in a children’s infectious diseases hospital is required.
Blood in stool in men
A specific cause of blood in the stool in men associated with gender differences is the advanced stages of prostate cancer. In an advanced stage, a prostate tumor grows through the wall of the large intestine and is injured during defecation.
Blood during bowel movements in women

The specific causes of blood in the feces in women are associated with the physiology of the female body:
Varicose veins of the perineum against the background of the last trimester of pregnancy;
intestinal endometriosis;
Side effects of radiation therapy for cancer of the reproductive organs.
At the end of pregnancy, the growing uterus has a mechanical effect on the pelvic organs and peritoneum. The lower sections of the intestines, the genitals are more intensively supplied with blood than usual, its clotting is slightly reduced within the physiological norm of the development of pregnancy. Therefore, with bowel movements accompanied by constipation, blood in the feces is occasionally possible. If it worsens, medical attention should be sought to differentiate it from vaginal bleeding. Prevention of the appearance of blood during bowel movements – the introduction of foods with vegetable fiber into the diet, the use of soft toilet paper.
With endometriosis in a woman, cells spread in various organs that function similarly to the cells of the mucous endometrium of the uterus. They are brought in with a current of lymph or blood. During menstruation, endometriosis foci bleed. If a woman is diagnosed with intestinal endometriosis, then the cells will produce blood with mucus. Most often, its amount is minimal, pathology is detected only when tested for occult blood, and only during menstruation.
Possible complications – with significant foci, intestinal obstruction, stenosis is possible. Treatment is hormone therapy.
Complications of radiation therapy can be radiation colitis. Its symptoms are alternating diarrhea and constipation, the appearance of mucus and blood in the stool. The treatment is symptomatic, over time, the mucous membrane regenerates.
What to do if you find blood in your stool?

When such a symptom appears, first of all, you need to seek the advice of a proctologist, and do it as soon as possible. The doctor will find out the details of the pathology, study the anamnesis and prescribe diagnostic measures.
If blood is found in the feces – the main laboratory and instrumental diagnostics:
Fecal analysis for worm eggs, occult blood, coprogram;
Visual examination of the condition of the anus by the proctologist;
Rectal examination of the lower rectum (state of tissues, sphincters, mucous membrane);
Sigmoidoscopy is an instrumental examination of the large intestine, its tissues and peristalsis at a distance of up to 40 cm.
When clarifying the diagnosis, additional diagnostics are carried out:
X-ray examination of the gastrointestinal tract;
Ultrasound of the large intestine;
Colonoscopy.
To examine the upper parts of the digestive system, a consultation with a gastroenterologist is necessary. The doctor will analyze the patient’s complaints, palpate the abdomen in the projection of the stomach and small intestine.
Possible studies:
Ultrasound of the stomach and small intestine;
FGDS, or gastroscopy (an auxiliary examination method).
In most cases, if there is blood in the stool, several studies are enough to clarify the diagnosis. It should be remembered that an early appeal to a specialist and a timely diagnostic examination will help preserve health and life, and shorten the period of recovery of health after treatment.









