What are the risks of thromboembolic disease?
Thromboembolic disease is classically defined as the presence of a blood clot in a vein, either in one of the calves or in the lungs. But there are also other types of thrombosis in the arteries of the heart and the vessels of the brain.
What is thromboembolic disease?
Thromboembolic disease is linked to the occlusion of a deep vein by a blood clot (thrombus or thrombosis) which is typically located in one of the calves (phlebitis) or in the pulmonary vessels (pulmonary embolism). Pulmonary embolism is very often the consequence of a migration of a thrombus from a deep vein in the calf during phlebitis (7 times out of 10).
Venous thrombosis can be deep (DVT) or superficial (TVS). In both cases, this venous thrombosis requires a diagnosis for its localization by Doppler echo. TVS is usually milder than DVT.
Pulmonary embolism is the obstruction of one or more arteries leading to the lungs by a thrombus, most often from calf phlebitis. But it can also occur independently of phlebitis due to bleeding disorders. It is sometimes massive affecting a large part of the lung tissue, sometimes life-threatening. It can also be more modest and more easily absorbed with treatment.
Beyond venous thromboembolic disease, there are also other places of thrombosis, in particular the arteries of the heart (coronary) which are the cause of myocardial infarction. The vessels of the brain can also be the site of thrombosis (cerebral thrombosis as a possible and rare complication such as during a vaccination against Covid) and be the cause of serious neurological sequelae or even death.
Mortality from untreated thromboembolic disease is of the order of 30% of cases.
What are the causes of thromboembolic disease?
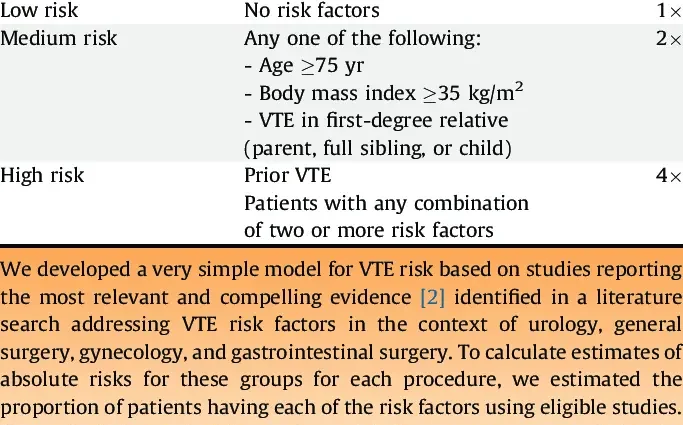
There are several causes or risk factors for developing venous thromboembolism:
- prolonged bed rest, more than four days, in hospitalized subjects for example;
- age over 40;
- obesity or overweight;
- sedentary lifestyle or lack of sport;
- taking certain hormones such as estrogen or the contraceptive pill;
- pregnancy due to abdominal hyperpressure which slows venous return to the heart;
- a cancerous disease which is associated with an overall inflammatory state of the organism facilitating thrombosis as well as chemotherapy;
- venous insufficiency of the lower limbs (varicose veins) and poor venous return;
- heart failure which slows blood flow;
- bleeding disorders related to a congenital disease or the taking of certain medications;
- trauma and surgery of the small pelvis, gynecological or digestive.
Arterial thromboembolic events such as myocardial infarction, or cerebrovascular accidents (stroke) are favored by altered arterial walls (atherosclerosis, atherosclerotic plaques, etc.). Emboli (thrombi) can form in the coronary arteries for myocardial infarction or migrate to the brain for stroke.
What are the symptoms of thromboembolic disease?
Symptoms of thromboembolic disease depend on the location of the thrombosis:
For phlebitis of the lower limb
Symptoms include pain, heaviness and swelling of the calf. Edema may also be present on the top of the foot.
For pulmonary embolism
The symptoms are a sudden pain on one side of the chest, a sudden difficulty in breathing (dyspnea with short and rapid breathing), sometimes bloody sputum, a cough …
For myocardial infarction
There is a sudden pain in the chest or pit of the stomach, with irradiation to the upper left limb and the neck to the jaws, associated with a feeling of crushing or tightness of the chest, sweating and a strong anxiety …
For stroke
It is a sudden paralysis of one of the limbs on one side only, on one side of the face, loss of sight in one eye, headaches, nausea, sometimes loss of consciousness or even a coma when the stroke is massive …
In all cases, these are medical emergencies to be taken care of as quickly as possible in the hospital.
The diagnosis is then confirmed by a Doppler ultrasound for phlebitis, a CT scan and a pulmonary scintigraphy for pulmonary embolism and D-dimer assay, an ECG and troponin assay for myocardial infarction and a CT scan for myocardial infarction. Stroke.
What are the treatments for thromboembolic disease?
For phlebitis, an anticoagulant treatment (low molecular weight heparin) must be implemented quickly with elevation of the leg and restraint of the calf with elastic stockings.
Pulmonary embolism should also benefit from anticoagulant therapy, oxygen therapy or surgery in the most severe cases.
Myocardial infarction may benefit from a catheter intervention for thrombolysis to dissolve the blood clot in the blocked coronaries associated with angioplasty to dilate these arteries of the heart.
Cerebrovascular accident (stroke) must be treated very quickly (within two to three hours after the onset of the accident) with a medicine that dissolves the clot (fibrinolytic) injected through the veins.
The prevention of these vascular accidents involves long-term coagulant treatments, the wearing of compression stockings for the risk of phlebitis, regular physical activity, stopping smoking, reducing overweight, stopping drugs that promote thrombosis (contraceptives, some anti-inflammatory drugs, etc.), varicose vein surgery, lowering of cholesterol, antiplatelet therapy such as long-term aspirin.