Contents
What is vaginitis
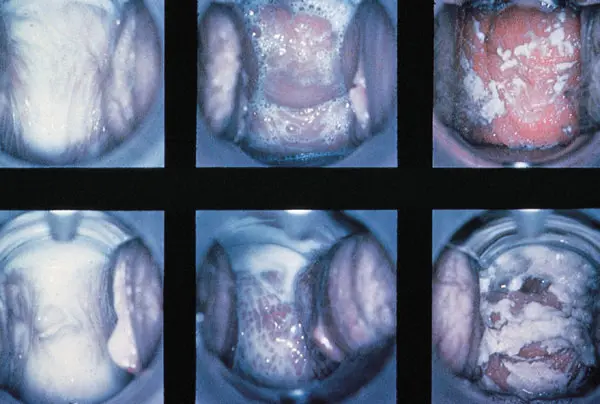
Vaginitis (colpitis) is an inflammatory process in the woman’s vagina, which gives her terrible discomfort. Moreover, if the inflammation affects only the vaginal mucosa, then we are talking about vaginitis, and if the external genital organs are also involved in the process, then this is already vulvovaginitis.
Vaginitis is a fairly common disease, and it can cause serious complications, for example, affect the reproductive health of a woman, if the infection goes up, goes to the uterus and ovaries. Subsequently, an ectopic pregnancy and even infertility may occur.
What you need to know about vaginitis in women
| Abundant discharge | Yes |
| Color and consistency | yellow green |
| Characteristic odor | no |
| Redness of the vaginal mucosa | Yes |
| Vaginal pH | > 6,5 |
| Leukocytes in a smear | > 10 |
Causes of vaginitis in women
Depending on the causative agent of the disease, two forms of vaginitis in women are distinguished – specific and nonspecific. Specific vaginitis includes gonorrheal, trichomonas, chlamydial, ureaplasma or mycoplasmal, syphilitic vaginitis. Sometimes several infections are detected simultaneously in a smear.
Nonspecific vaginitis arises from the woman’s own microflora, which becomes pathogenic under certain stressful conditions. These are gardnerella, streptococcus, Pseudomonas aeruginosa, Candida fungus and other microorganisms that are normally present in the microflora of the female vagina, but in negligible amounts and do not cause any unpleasant symptoms. We list the causes and factors under which the pathogenic microflora develops:
- non-observance of personal hygiene rules;
- low immunity;
- disruption of the endocrine system (diabetes mellitus, menopause, decreased ovarian function);
- overweight;
- frequent change of sexual partners and unprotected intercourse,
- prolonged mechanical irritation and damage to the vaginal mucosa (for example, during sexual intercourse without a sufficient amount of natural lubrication or lubricants);
- hypothermia;
- frequent (and often completely unnecessary) douching;
- deodorants and overly scented intimate hygiene products;
- taking antibiotics.
Symptoms of vaginitis in women
The main symptoms of vaginitis in women include:
- pain in the lower abdomen (may increase during / after sexual intercourse);
- severe itching in the genital area;
- copious, often frothy, yellowish or greenish discharge;
- bleeding between periods;
- redness and swelling of the external genital organs;
- pain and discomfort when urinating, sometimes the infection also affects the bladder, then cystitis occurs.
Also, vaginitis can occur in acute and chronic form. In the chronic form of vaginitis, most of the symptoms are in an erased form, and the woman notes only pathological discharge in herself. An exacerbation of the disease occurs with a decrease in immunity, hypothermia, dysbacteriosis and infectious diseases. In the chronic form, the infection can spread to the internal organs, including the uterus and kidneys.
Treatment of vaginitis in women
Treatment of vaginitis begins with a visit to a gynecologist who will prescribe the necessary tests and select therapy.
Diagnostics
During the appointment, the doctor collects an anamnesis of the disease, asks the patient how long ago the symptoms appeared, what kind of discharge, what preceded the onset of symptoms, does the patient have any chronic diseases, is she sexually active, are sexual intercourses protected, did she take antibiotics recently, etc. During a gynecological examination, a smear is taken for pathogens with the determination of their sensitivity to antibiotics. If a sexually transmitted infection is suspected, a PCR test is ordered to identify common STI pathogens. If necessary, the doctor may prescribe an ultrasound of the pelvic organs, if there is a suspicion that the inflammation has affected the internal organs.
Therapies
– The main treatment for vaginitis is the use of drugs, depending on the etiology of the disease. These can be modern antibiotics for specific vaginitis caused by pathogenic microorganisms, and local modern drugs for the treatment of aerobic vaginitis, clarifies obstetrician-gynecologist of the highest qualification category Natalya Belyaeva.
Thus, with bacterial vaginitis, antibiotics and local preparations are prescribed that relieve itching, inflammation, and relieve unpleasant discharge. With a fungal infection, antifungal drugs are prescribed in the form of tablets and suppositories based on Clotrimazole, Fluconazole, Miconazole, etc. If vaginitis is not infectious, it is necessary to eliminate the causes that caused it – change the intimate hygiene product, wear underwear made of breathable cotton fabrics, etc. d. It is also very important to restore your own immunity and the natural microflora of the vagina – for this, preparations containing useful lactobacilli are prescribed.
Prevention of vaginitis in women at home
Prevention of vaginitis in women includes:
- refusal of casual sexual relations and frequent change of partners;
- using condoms during intercourse;
- observance of personal hygiene;
- rejection of tight synthetic underwear;
- do not use panty liners;
- do not resort to douching without a doctor’s prescription, as this helps to wash out the beneficial microflora of the vagina;
- when taking antibiotics, additionally take probiotics to preserve the natural microflora in the intestines and vagina;
- regular preventive examinations at the gynecologist (twice a year).
Popular questions and answers
Answers to popular questions about vaginitis in women obstetrician-gynecologist of the highest qualification category Natalya Belyaeva.