Contents
- Causes and symptoms of urinary incontinence in women
- Diagnosis of urinary incontinence in women
- Urinary incontinence in older women over 50
- Treatment of urinary incontinence in women
- Vitafon for urinary incontinence
- Treatment of stress urinary incontinence
- Operative therapy
- Treatment of urinary incontinence with folk remedies
- 3 effective exercises for urinary incontinence

Urinary incontinence is a fairly common problem. More than half of all representatives of the weaker sex face it at least once in their lives. Incontinence can occur both in young women after childbirth or surgery, and in mature women after menopause. Statistics show that every fifth girl suffers from urinary incontinence in the reproductive age, every third woman faces this problem in the early period of menopause, and after 70 years – every second elderly woman.
Urinary incontinence is a serious problem that significantly impairs the quality of life, leads to disorders in the sexual and psychological sphere, can provoke depression, and becomes an obstacle to the successful building of a personal life and career. Enuresis should be considered from the point of view of not only a hygienic aspect – this disease also has medical and social significance, as it causes a wide variety of problems in women: sexual dysfunctions, neuroses, etc.
You can also come across such a term as incontinence, which also means urinary incontinence, but is more often used by urologists and gynecologists when making a diagnosis. Enuresis is the name given to a urinary incontinence that is accompanied by an inability to regulate the emptying of the bladder. Leakage volumes can vary from a few drops to almost the entire contents of the organ. Gynecologists, urologists, surgeons and psychotherapists are engaged in the treatment of the disease.
The problem of urinary incontinence is so global that even a special international medical organization has been created to study the causes of enuresis and develop new effective methods of treating this disease.
Causes and symptoms of urinary incontinence in women

There are the following types of urinary incontinence:
stressful;
Imperative (urgent);
iatrogenic;
mixed;
Other forms, for example, enuresis with overflow of the bladder, continuous leakage of urine, unconscious incontinence, etc.
In women, it is the first three types of urinary incontinence that are most common, so it is worth dwelling on them in more detail.
stress urinary incontinence

Stress urinary incontinence is the inability to control the process of emptying the bladder during stress. The word “stress” in this context means “load” or “effort”.
Symptoms of stress urinary incontinence:
Urine excretion with laughter, coughing, sneezing, physical exertion, sexual intimacy.
If there is no tension in the abdominal cavity, then urine is not excreted.
Not every cough or sneeze results in the involuntary release of urine. In the early stages of incontinence, this occurs only when the organ is full, and the amount of urine lost is equal to a few drops.
As the disease progresses, even minor physical activity, such as brisk walking, can lead to loss of urine.
Irresistible urge to urinate in a woman is absent.
Together with urine, involuntary excretion of feces and gases from the intestines can occur.
Normally, physical activity, as well as coughing and laughing, should not lead to the release of urine. This is prevented by the pelvic floor muscles and the sphincter. However, when they are weakened, they become unable to fully cope with their function. Urine overcomes their resistance and flows out.
The reasons can be several:
Difficult childbirth. In this regard, childbirth is especially dangerous, accompanied by the release of a large fetus, perineal incisions, the application of forceps and other manipulations. Women with a narrow pelvis are at risk.
Surgical interventions on the pelvic organs. Any intervention on the bladder, rectum, uterus can lead to stress urinary incontinence. Fistulas that form between organs are dangerous, since these defects also lead to urinary incontinence.
Hormonal changes in a woman’s body that occur with age. The less estrogen is produced, the worse the elasticity of the ligaments becomes and the lower the muscle tone will be.
In addition to the main causes that lead to stress urinary incontinence, the following risk factors can be additionally identified:
Overweight, especially in combination with diabetes;
Sharp weight loss;
Hard work associated with high physical exertion;
Passage of radiation therapy;
Prolapse and prolapse of the uterus;
Frequent cystitis and urethritis;
Weight lifting;
Burdened heredity;
Belonging to the Caucasian race;
Neurological diseases, including heart attacks, strokes, spinal injuries;
Bronchial asthma, obstructive pulmonary disease;
Chronic constipation;
Anemia;
Taking certain medications.
Urgent urinary incontinence

Urgent urinary incontinence is characterized by an unbearable urge to empty the bladder. These urges are imperative, and it is almost impossible to restrain them. Moreover, they occur when the bladder is only partially filled. While normally, a woman experiences an urge to urinate when a sufficiently impressive volume of urine accumulates in the bladder.
Symptoms of urge urinary incontinence include:
The urge to empty the bladder is very frequent and occurs more than 8 times a day.
They almost always appear suddenly.
The urge to urinate is irresistible.
There are frequent trips to the toilet at night.
The urge to urinate is often dictated by external factors, including, for example, the sound of running water from a tap, a bright light, a loud sound, etc.
When urge urinary incontinence occurs against the background of a prolapsed bladder, a woman may experience pain and discomfort in the lower abdomen.
Urine leakage may be accompanied by the development of dermatitis in the groin area, the occurrence of such genitourinary infections as vulvitis, vulvovaginitis, pyelonephritis, cystitis, etc.
The cause of urge urinary incontinence in women lies in the violation of neuromuscular transmission in the detrusor of the bladder (muscular frame), which leads to its increased activity. Therefore, even when a small amount of urine accumulates in the cavity of the organ, the woman experiences the urge to urinate. As for the risk factors that can lead to the development of urge urinary incontinence, they are similar to the risk factors for stress incontinence. Often these two types of incontinence are combined with each other.
iatrogenic urinary incontinence

Iatrogenic urinary incontinence is incontinence that develops while taking medications. As a rule, enuresis becomes a side effect of a particular medication.
You should be aware that medications such as:
Adrenomimetics (Pseudoephedrine), which are used to treat bronchial diseases. First, such drugs provoke urinary retention, and then cause her incontinence.
Any diuretic drugs.
Blockers.
Hormonal preparations containing estrogen in their composition.
Colchicine, which is used in the treatment of gout.
Antidepressants.
Sedative medicines.
When the course of treatment with the listed drugs is completed, urinary incontinence will pass on its own and will not require any therapeutic measures.
Diagnosis of urinary incontinence in women

Diagnosis of urinary incontinence should begin with keeping a diary. You need to fix the data in it for several days. At this time, a woman should write down how much liquid she drinks, how many times she goes to urinate. It is important to measure the amount of urine released, as well as display in the diary all episodes of urinary incontinence and what she was doing at that time. To understand exactly how much urine goes into episodes of incontinence, you can use the so-called PAD test. For a certain time, the patient wears urological pads, weighing them before and after use.
A conversation in the doctor’s office is of no small importance. It allows you to find out the symptoms of the disease, the time of its manifestation.
A woman must visit a gynecologist. During the examination on the chair, the doctor assesses the condition of the muscles and tissues of the pelvic floor, the presence or absence of prolapse of the vaginal walls and uterus.
A cough test is performed in the gynecologist’s office. The woman is asked to cough while her bladder is full. If urine is expelled during exertion, stress urinary incontinence may be suspected.
As a rule, the diagnosis is not difficult in most cases. However, additional tests may be required, such as:
Cystoscopy. This study involves examining the bladder from the inside. For this purpose, a thin cystoscope is inserted inside through the urethra. The procedure for a woman is painless, for which the doctor uses a special anesthetic gel. Cystoscopy makes it possible to assess the condition of the bladder, to exclude the presence of tumor formations.
Urodynamic examination evaluates the process of filling and emptying the bladder. To carry it out, special sensors are inserted into the bladder itself and into the vagina, which provide the information necessary for the doctor.
Ultrasound of the pelvic organs. This examination allows you to assess the state of the organs of the female reproductive system, which makes it possible to determine the further therapeutic tactics.
As for laboratory research methods, a woman is prescribed a general and bacterial analysis of urine, a microscopic examination of a smear. Thanks to the above methods of examination, the doctor will be able to make the most accurate diagnosis and prescribe the necessary treatment.
Urinary incontinence in older women over 50

Most often, in older women over the age of 50, a mixed form of urinary incontinence predominates, that is, there is both a stress and an urgent component.
There can be many reasons that lead to the disease, so the doctor during the examination must find out the following points:
Does the woman suffer from neurological pathologies.
Does she have mental disorders?
Does the woman have signs of Parkinson’s disease.
Does the woman suffer from diabetes?
Does she have problems with being overweight?
Whether there are herniated discs or other degenerative diseases of the spinal cord that can affect the functioning of the bladder.
Did the woman have a history of surgery on the pelvic organs. If there were any, then it is important to find out if they provoked the formation of adhesions and fistulas.
All these diseases can be the cause of urinary incontinence, as in one way or another they can affect the functionality of the bladder. It is possible that the woman has “overfilling incontinence”, that is, due to the reduced sensitivity of the organ, the signal to empty it is transmitted to the brain too weakly, or not at all.
It is important to find out which medications a woman is taking. Particular attention is paid to sedative and antihypertensive drugs, diuretics.
In elderly patients diagnosed with stress incontinence in 30% of cases, pelvic organ prolapse is detected, namely, prolapse of the bladder. Therefore, the approach to both diagnosing an existing problem and treating older women must necessarily be individualized. We should also not lose sight of the fact that urinary incontinence can develop against the background of relative health due to a lack of estrogen production in the postmenopausal period.
A comprehensive urodynamic examination for elderly women complaining of urinary incontinence is prescribed without fail.
Treatment of urinary incontinence in women

Therapeutic tactics largely depend on what exactly caused the urinary incontinence and how far the problem has gone. The disease is treated by gynecologists, urologists and surgeons (if surgery is required).
Treatment of any type of urinary incontinence should be started according to the principle “from simple to complex”.
First, you should definitely try the most accessible methods, including:
Getting rid of excess weight in the presence of obesity. The fact is that excess body weight affects the state of internal organs, which are subjected to excessive pressure. As a result, their location is disturbed, functioning suffers, which leads to problems with urination. Obesity can be treated with diet, medication, psychotherapy, or gastric surgery.
Any drinks that contain caffeine should be limited. This primarily applies to coffee and tea. The ban on caffeine is due to its diuretic effect on the body. With excessive intake of this substance, the risk of urinary incontinence increases significantly. As for the use of ordinary clean water, it cannot be limited, otherwise the situation can be aggravated.
Refusal of cigarettes. So far, no clear relationship has been established between smoking and the problem of urinary incontinence. However, it has been proven that women suffering from smoker’s bronchitis are many times more likely to develop stress urinary incontinence. In general, any diseases of the respiratory system must be treated in a timely manner.
Imperative urinary incontinence is perfectly treated when the patient manages to correct the urination regimen. The essence of this method boils down to the fact that you need to accustom your body to urinate by the hour. The initial interval can be set to 30 minutes and then increased to an hour or more.
In order to increase the tone of the pelvic floor muscles, you should exercise regularly. Special exercises will allow you to correct the work of the sphincter and the walls of the bladder.
All chronic diseases must be treated in a timely manner in order to prevent their exacerbation.
It is equally effective to create a psychological attitude that distracts from the desire to empty the bladder.
Kegel exercises
Kegel exercises are a gymnastic complex that is very easy to implement. First, a woman must decide what the pelvic floor muscles are and where they are located. To do this, you need to imagine the process of emptying the bladder and try to stop it with muscle power. It is these muscles that should be involved during training.
Three times a day you need to strain and relax the muscles of the pelvic floor. The tension time ranges from a few seconds at the initial stages of training to 3 minutes later. Kegel exercises can be performed almost anywhere and anytime, as they are completely invisible to others.
When the muscles are sufficiently trained, you can try to strain them during coughing and sneezing, during physical exertion. The more varied the exercises, the higher their effectiveness.
You can use techniques such as fast and slow contractions, pushing out like pushing during childbirth, holding the jet during emptying of the bladder.
biofeedback therapy
Exercises with biofeedback (BFB) are superior to Kegel exercises in that they allow you to strain only the right muscles. To implement the complex, specialized equipment is required. It is designed not only to control the process of muscle tension, but also to additionally stimulate them with the help of electrical impulses.
It has been proven that biofeedback training allows you to achieve control over urination in a fairly short time. However, exercises are prohibited for implementation in the presence of malignant tumors, inflammatory diseases in the acute stage, pathologies of the heart, liver and kidneys.
The use of simulators for the treatment of urinary incontinence
There are a lot of devices that allow you to train the muscles of the pelvic floor. Many of them are very compact and easy to use. For example, the PelvicToner simulator allows you to competently increase the load on the muscles, gradually strengthening them. The device is very easy to use, and its effectiveness has been proven in clinical studies.
Psychotechnics
When you have the urge to urinate, you can try to distract yourself from them by moving your thoughts in a different direction. For example, think about upcoming plans for life, read interesting literature, etc. The main task that a woman faces is to delay urination, at least for a short time.
Medications
Table of essential drugs for urinary incontinence
Candles Ovestin
Minirin
Driptan
Picamilon
Duloxetine
Melipramine
Pantocalcin
Pantogam
Vitafon for urinary incontinence

The Vitafon device is a vibroacoustic device that allows you to strengthen muscles and rejuvenate the body. Treatment with Vitafon refers to physiotherapeutic methods of exposure that can be used at home. The device is a housing block connected to the mains. Attached to it are two round diaphragms that emit acoustic vibration in several programmable ranges. It is these membranes that need to be applied to problem areas to provide a therapeutic effect.
Mechanism of action. Phosphonation with Vitafon allows you to massage the desired area, and the effect is carried out at the cellular level, which improves the nutrition of tissues, both muscle and nerve.
In case of urinary incontinence, phonation of the following zones is carried out:
Perineum area – 10 minutes;
The area of the muscular sphincter of the bladder (slightly above the pubis) – 10 minutes;
Kidney area – 10-30 minutes;
Liver area – up to 15 minutes;
Lumbo-sacral zone – 5 minutes.
Each zone is treated 1-3 times a day. The course of treatment continues until a stable result is obtained.
Vitafon is used to treat enuresis in children.
Contraindications:
Increased body temperature.
Malignant neoplasms in the affected area.
Atherosclerosis.
Thrombophlebitis.
Infectious diseases in the acute stage.
Pregnancy.
Reviews. Doctors speak of the Vitafon device as an effective device that allows you to get rid of urinary incontinence. However, you should not expect a miracle, so before you start using the device for the treatment of enuresis, you should consult a doctor and find out the causes of incontinence. Reviews of people who have used the device for the treatment of urinary incontinence are mostly positive. Often it is used to get rid of this problem in all family members.
Treatment of stress urinary incontinence

If a woman suffers from stress urinary incontinence, then consultation and medical assistance will be necessary for her. The fact is that with the help of conservative methods, it is most often not possible to achieve an effect in this type of disease.
Treatment with drugs is indicated when stress incontinence is mild, and the muscles and ligaments have not lost their integrity. Medical correction is possible with the following drugs:
Gutron (adrenomimetic). The drug increases the tone of the urethra and sphincter. It is prescribed quite rarely, as it has a negative effect on the state of the vascular wall and contributes to an increase in blood pressure.
Ubretide (anticholinesterase drug). The drug increases muscle tone. It is indicated for those patients who suffer from hypotension of the bladder.
Duloxetine or Cymbalta (antidepressant). The drug helps in 50% of cases, however, it has a negative effect on the digestive tract.
In general, drugs for the treatment of stress urinary incontinence are prescribed infrequently, as they have low efficacy, but a sufficient number of side effects.
Operative therapy

Operations are indicated in the case when it is not possible to achieve an effect by other methods of correction of urinary incontinence. The choice of a specific surgical technique depends on the characteristics of the female body, as well as on the degree of enuresis.
However, there are general contraindications to any type of operation, including:
Identified malignant tumor.
Inflammation in the pelvic organs, which is in the acute stage.
Decompensated diabetes mellitus.
Blood clotting disorders.
The following operations are possible:
Sling operations (TVT, TVT-O). These operations are less traumatic and quite effective. During their conduct, a special loop is carried out under the neck of the bladder, which is fixed in the desired position. This loop supports the urethra and prevents urine from flowing out. After such an intervention, the woman recovers very quickly, however, the risk of relapse remains.
> Read more: TVT sling operation
Bulk injections. This method of treatment boils down to the fact that a special substance is injected into the urethra, which is designed to fill the deficit of missing soft tissues and maintain the urethra in the desired position. The operation is performed in an outpatient setting and does not require general anesthesia. However, the risk of relapse remains.
> Read more: Periurethral injections of bulking agents
Colporrhaphy. This method boils down to the fact that the vagina is sutured with special threads. The procedure is indicated for prolapse of the pelvic organs and has a number of complications. It is possible that a relapse will occur after a few years.
> Read more: anterior colporrhaphy
Laparoscopic colposuspension according to Burch. This operation aims to suspend the tissues around the urethra from the inguinal ligaments. The procedure requires the introduction of general anesthesia, has many contraindications and more complications than sling operations. Therefore, colposuspension according to Birch is implemented only when the operation using the loop did not bring the desired effect.
> Read more: Burch laparoscopic colposuspension
Treatment of urinary incontinence with folk remedies

Clover plowed. An herb called plowed clover can be used to treat urinary incontinence. It should be brewed like tea and drunk as a weak solution. This herb can be purchased at a pharmacy.
Honey water. Honey has the ability to retain water. Therefore, traditional healers use it to treat enuresis. To get rid of urinary incontinence, before going to bed, you should drink half a glass of warm water, in which a teaspoon of honey is first diluted. The course of treatment is 3 days. Alternatively, you can drink 30 ml of honey water three times a day.
Dill seeds for enuresis in children. To save a child from enuresis, you can use dill seeds. You will need to take a tablespoon of seeds and pour them with a glass of boiling water, insist for an hour, strain. Use this infusion on an empty stomach. Children under 10 years old are given 1/2 cup, and children over 10 years old are given a whole glass of drink.
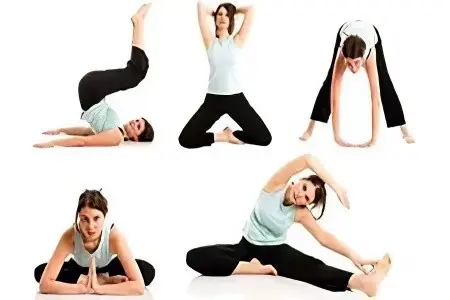
3 effective exercises for urinary incontinence
The following exercises can be used to treat urinary incontinence and should be done every day:
You need to squat down and connect your palms with each other at chest level. The back should be straight. Stay motionless in this position for at least 30 seconds.
It is necessary to lie on your back, spread your knees to the sides, while connecting the feet together. The arms are stretched along the body with palms up. In this position, you need to hold out for a minute.
You need to kneel and lower your buttocks to your feet. Stretch your arms forward, your face should look down. In this position, stretch the spine for a minute.









