Contents
Tumor of the pancreas is a neoplasm originating from the parenchyma of an organ or from the pancreatic ducts. The disease can not manifest itself for a long time, and people often confuse even late symptoms of a tumor with other lesions of the digestive system. The danger lies in the fact that a pancreatic tumor is prone to very rapid progression and metastasis to the lungs, lymph nodes, bones and liver.
Statistics indicate that every year about 10 people in the world out of every 100 of the population develop a pancreatic tumor. The disease itself ranks fourth in mortality among all oncopathologies and is 000 times more likely to be diagnosed in men. The risk of developing the disease increases after 1,5 years, and by the age of 30 it is gaining its maximum. Thus, 70% of all patients with a pancreatic tumor are people who have crossed the line of 63 years.
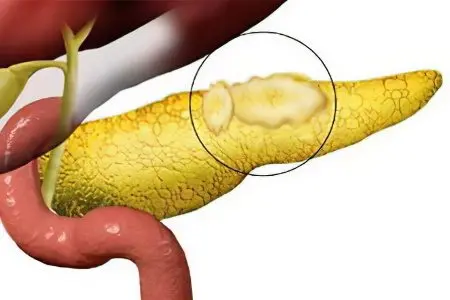
In 75% of cases, the tumor is located in the head of the gland, the tail and body are less often involved in the pathological process. In 95% of the pancreas, adenocarcinomas are formed – malignant glandular tumors.
Causes of pancreatic tumors
The causes of pancreatic tumors are still not exactly known to science. Therefore, only risk factors that can lead to this oncopathology are highlighted. However, up to 40% of cases of all tumors of the gland remain with an unexplained etiology.
All body cells are constantly dividing and periodically appear those that have a broken DNA structure. At this time, immune mechanisms are included in the work that destroy atypical cells. If the natural defense fails for some reason, then the mutated cells continue to divide and give rise to the formation of a tumor. In addition, as they accumulate, they trigger a special mechanism that allows them to hide from attacks by the immune system. When the body’s defense still recognizes the tumor, its own strength is no longer enough to completely eliminate it. However, as the body fights the pathology, early symptoms of the tumor can be suspected, which will be described later.
Risk factors that can provoke the development of a pancreatic tumor can be identified as follows:
Chronic pancreatitis. In this disease, iron is in a state of constant inflammation, which is the basis for cell mutation.
Pancreatitis, inherited.
Diabetes mellitus leads to the fact that a high level of glucose is constantly maintained in the blood, which increases the risk of developing a tumor of the gland.
Smoking, which contributes to permanent ischemia of the organ.
Overweight.
Cirrhosis of the liver.
A stomach ulcer that provokes a malfunction in the intestinal microflora. This, in turn, causes excessive production of toxic elements that lead to the development of a tumor.
Wrong nutrition. The risk of oncopathology of the pancreas increases with the use of meat that has undergone secondary processing (sausages, sausages, ham, bacon, etc.), coffee, carbonated drinks, fried red meat, foods containing a large amount of saturated fatty acids.
Crohn’s disease, ulcerative colitis.
Hypodynamia.
Diseases of an allergic nature.
Diseases of the oral cavity (pulpitis, carious lesions of tooth enamel, periodontitis).
Intoxication of the body with chemicals.
Age over 60 years.
Other oncopathologies of the body (tumors of the cervix, throat, intestines, stomach, etc.).
African race.
Genetic mutations in one’s own DNA structure.
Tumor of the pancreas in close relatives.
Male.
Transferred surgical interventions on the stomach.
Chronic pancreatitis, adenoma and cyst of the pancreas are considered by doctors as precancerous conditions.
Symptoms of pancreatic tumors

The symptom of pancreatic tumors at the initial stages of the development of oncopathology does not manifest themselves in any way.
However, as the malignancy grows, the patient begins to pay attention to the following signs:
Pain localized in the pancreas. Sometimes the pain can be girdle, sometimes it radiates to the back, or to the upper half of the abdomen. It is characterized by its strengthening when the body is tilted, and weakening when pressing the legs to the stomach. As the tumor grows, the pain will get worse.
If the tumor develops in the region of the head of the organ, then most patients are diagnosed with jaundice. Yellowing of the skin is accompanied by severe itching, while the urine becomes darker, and the feces lighter.
The stool acquires a fetid odor, in consistency it is predominantly oily and liquid.
Weight loss is a very common symptom indicating a malignant neoplastic lesion of the pancreas. It is observed in 92% of patients. The weight loss is explained by the fact that the normal process of fat absorption in the intestine is disturbed, since the pancreas does not secrete the enzymes necessary for this process.
Anorexia develops in 64% of patients in case of damage to the head of the gland. If the tumor is localized in other parts of the organ, anorexia will be detected only in 30% of patients.
Vomiting is a symptom that the tumor has compressed the duodenum or blocked the lumen of the stomach.
Secondary diabetes mellitus with an increase in the volume of urine excreted and with severe thirst is a common symptom of this oncopathology.
It is not excluded varicose veins of the esophagus and stomach, which provoke internal bleeding.
Sometimes the disease is manifested by symptoms of acute cholecystitis or pancreatitis.
Symptoms gradually increase, pain intensifies as the disease progresses. The tumor is prone to metastasis. It sends atypical cells to the lymph nodes (the nodes located next to the pancreas are the first to be affected), to the circulatory system (this is how other internal organs are affected), to the peritoneum (the intestines and pelvic organs suffer).
In addition, the tumor itself is able to grow into the bile ducts, into the stomach, into large vessels. This is the so-called tumor penetration.
Stages of pancreatic tumors
There are four stages of pancreatic tumors. However, the stage “cancer in situ” or the zero stage can be noted separately. A person does not experience symptoms of the disease, only a small number of gland cells undergo mutation. This stage can be detected only with the help of instrumental methods of examination (MRI, ultrasound, CT).
The main stages of pancreatic tumors are as follows:
The first stage divided into two substages – 1A and 1B. At stage 1A, the tumor is located only in the gland itself and does not exceed 2 cm in size. If it is not located near the exit to the duodenum 12 (in this case, nausea and diarrhea often occur), then no symptoms of the disease will be observed. In stage 1B, the tumor becomes larger and sometimes symptoms of jaundice, pain, nausea, and vomiting appear.
The second stage also divided into two substages – 2A and 2B. The first of them is characterized by the germination of the tumor in nearby organs, into the bile ducts, and the second by metastasis to the regional lymph nodes. In this case, severe abdominal pain may already occur, anorexia, vomiting and diarrhea may develop.
At the third stage disease occurs damage to large vessels (hepatic artery, superior mesenteric artery, celiac trunk, portal vein, veins of the large intestine and other organs).
For the fourth stage the disease is characterized by metastases of other organs, even far located, for example, the brain or ovaries. Symptoms are gaining their maximum and largely depend on what other organ is affected by daughter tumors.
Prognosis of the disease
The prognosis of the disease is most often extremely unfavorable. The average life expectancy of patients with pancreatic cancer is 4 to 6 months. Only 3% of people live five or more years. This is due to the fact that a tumor of the gland is most often diagnosed in the later stages, and the vast majority of patients are elderly people who can no longer undergo a radical operation. However, when a tumor of the zero stage is detected, the effectiveness of treatment reaches 99%.
Diagnosis of a pancreatic tumor

Diagnosis of pancreatic tumors presents certain difficulties, since the symptoms of the disease are most often blurred. No more than 30% of tumors are found before the age of 2 months.
The following laboratory tests allow suspecting oncopathology:
General blood analysis. The ESR and the number of platelets are growing, hemoglobin is falling.
A biochemical blood test indicates an increase in bilirubin in the blood, an increase in the number of liver enzymes.
Determination of tumor markers in the blood. The possibility of the operation is indicated by the CA-19-9 marker, which, in the early stages of tumor development, is not detected. In 50% of patients, the CA-125 marker is detected. For the later stages of the development of oncopathology, tests for markers CF-15, CA-494, etc. will be positive.
Instrumental diagnostic techniques make it possible to determine the presence of a tumor process with a greater degree of probability:
Ultrasound of the abdominal organs.
CT and MRI make it possible to visualize a tumor less than 1 cm, and also help to identify metastases.
PET helps to detect malignant tumors and their metastases.
Retrograde cholangiopancreatography refers to invasive techniques and can detect tumors larger than 2 cm.
A biopsy followed by a histological examination of the material is performed during diagnostic laparoscopy or directly during surgery.
Treatment of a pancreatic tumor
Treatment of a pancreatic tumor involves its surgical removal. To do this, the altered tissues of the organ are excised. If there are no contraindications to the operation, then it is desirable to perform a radical removal of the neoplasm and the pancreas itself. At the same time, the gallbladder, duodenum, part of the stomach and intestines are often removed from the body along with the gland. Within 5 years after such an operation, no more than 25% of patients live. In addition to complete resection, it is possible to perform distal and segmental resection.
In some cases, it is not possible to completely remove the tumor, but operations are still performed. Their goal is to make life easier for patients. For this, metastases can be removed, obstruction of the biliary tract or intestines is eliminated. It is possible to remove part of the tumor so that it stops pressing on the nerve endings and does not cause severe pain to the patient.
As for the drug treatment of pancreatic cancer, chemotherapy is used for this purpose. It is aimed at suppressing the growth of atypical cells. The drugs used for this purpose are Semustine, Fluorouracil, Streptozocin, etc. A combination of several drugs is possible.
Enzymatic deficiency is compensated by taking enzyme preparations – Creon, Pancitrate, Pancrease.
All patients with a pancreatic tumor should follow a diet with an increased content of proteins and fats in it, which will prevent the development of anorexia.
Radiation therapy may be given before surgery to reduce the size of the tumor, during surgery to prevent recurrence of the disease, or if surgery is not possible.
Hericium against pancreatic tumor

Hericium is a fungus that grows on stumps and dead tree trunks. Oriental medicine has been using Hericium pectinate (the scientific name for the fungus) since ancient times. Modern Chinese doctors prescribe it for the treatment of malignant tumors, equating the effect of its use with radiation therapy or chemotherapy. Hericium is also used if it is no longer possible to perform an operation to remove a pancreatic tumor.
Due to the inclusion of YA-2 fatty acids, phenols, beta-glucans and other polysaccharides in the composition of the fungus, it is possible to help the body in the fight against oncopathology. These same substances can enhance the effect of ongoing chemotherapy by 2-7 times.
Japanese scientists conducted an experiment with mice. The rodents were transplanted with cancer cells, and then the formed tumor was treated with hericium. As a result, tumor growth stopped in some mice, and in some of them it even decreased in size.
Hericium can be used in powder form, or as a tincture. You can buy it in an online store or from herbalists (they most often offer ready-made tinctures).
The ways to use the mushroom are as follows:
Mix powder (1 g) in a glass of warm water and leave for 12 hours. Then the resulting infusion is divided into three parts and drunk during the day, 30 minutes before meals.
You can prepare the remedy in a similar way, but use it in full right after a night’s rest on an empty stomach.
You can prepare an infusion of 150 ml of vodka and 10 g of powder. To withstand such an infusion should be in a cool place for 14 days. For prophylactic purposes, you should take a teaspoon of infusion 3 times a day, and for therapeutic purposes, a tablespoon 3 times a day.
Another way to use hericium: in 150 ml of vegetable or olive oil heated in a water bath, add 10 g of powder and mix well. After that, the mixture is removed from the fire and kept in a warm place for 3 hours. Then it is stored in the refrigerator for another 5 days. Take according to the scheme described in the third paragraph.









