Contents
What is tularemia?
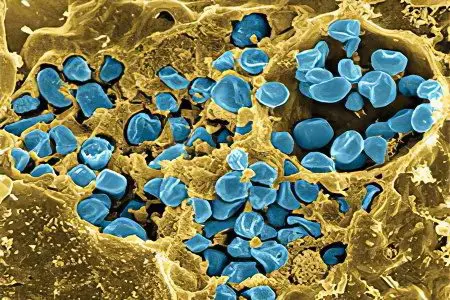
Tularemia is an infectious disease caused by the bacterium Francisella tularensis. It enters the human body in the case of a bite by a sick animal or after eating infected meat. Transmission routes are also known through untreated water and during the processing of the skins of slaughtered livestock.
Bacteria enter the human body through the skin, mucous membranes, respiratory tract and gastrointestinal tract, causing intoxication and, as a result, inflammation of the lymph nodes.
The disease proceeds in a rather severe form and affects mainly the lymphatic system, forms ulcers on the skin, in some cases the changes affect the eyes, throat and lungs of the patient. Complications of tularemia include diseases of the internal organs.
Both children and adults are susceptible to tularemia, but in most cases the disease was recorded in the latter. According to statistics, the incidence in men is twice as high as in women.
The main risk factor for infection is professional activity: fishing, hunting and agriculture, which are based on direct contact with potentially hazardous natural sources.
Tularemia has long been recognized as a disease of rural areas, but in the modern world there is a tendency for a steady increase in the incidence among urban residents. The infection is active all year round, but about 80% of cases are recorded in summer and autumn.
Symptoms of tularemia in humans
From the moment of infection to the appearance of the first symptoms of the disease, about five days pass, in some cases this period is delayed up to two weeks.
Turalemia has a standard set of the following symptoms:
body temperature of 39 degrees and above, which can last up to 14 days;
severe headache and dizziness up to fainting;
general malaise, accompanied by weakness and fatigue;
muscle pain;
loss of appetite and nausea.
Various forms of the disease have additional symptoms:
With ulcerative bubonic tularemia (after the bite of an infected tick):
an ulcer appears at the site of the bite;
located closest to the site of the bite, the lymph node becomes inflamed and becomes painful.
In the case of the bubonic form of the disease that develops after the bite of a sick animal:
lymph nodes become especially painful at the site of the bite;
after a while, the inflamed lymph node forms pus and opens.
Abdominal tularemia occurs after eating the meat of an infected animal.
Symptoms of this form are similar to those of food poisoning:
nausea;
vomiting;
decreased or complete lack of appetite;
diarrhea;
pain in the hypochondrium.
In the pulmonary form of tularemia, infection occurs by airborne droplets and proceeds along the bronchial type:
the bronchi are affected, and a dry cough appears;
there is pain behind the sternum;
a severe degree is characterized by symptoms of severe pneumonia: shortness of breath, cough with purulent sputum, chest pain.
Any form of tularemia requires immediate treatment, without which the likelihood of death occurs in 6 out of 10 cases.
Treatment of tularemia in humans

Comprehensive treatment of tularemia in humans involves therapy aimed at detoxifying the body and further relieving inflammation. The result obtained is fixed by the appointment of antihistamines, vitamin complexes and agents that normalize and support the work of the cardiovascular system. Local treatment of bubonic and ulcerative formations on the skin is the use of dressings with ointment, compresses, as well as the use of laser irradiation and diathermy. If the buboes contain a purulent mass, they are opened and drained.
Streptomycin has been proven to be highly effective in treating tularemia. The drug is administered intramuscularly every 12 hours. The course is from 7 to 14 days. If there is a possibility of developing tularemia meningitis, gentamicin is prescribed. The doctor may prescribe tetracycline or other drugs, focusing on the severity of the disease and the individual characteristics of the patient.
Treatment continues until the normal temperature stabilizes (usually necessary to control body temperature for 5 days).
A prolonged and complicated form of tularemia requires combined treatment, which includes antibiotic therapy with vaccination. The injection is administered intramuscularly, the dose is 1-15 million microbial bodies per procedure. The course of vaccination is 6-10 sessions every 3-5 days.
During treatment or after discharge, the doctor prescribes the use of vitamin complexes. In some cases, a blood transfusion may be required.
Discharge from the hospital is possible only after a complete clinical recovery.
Prevention of tularemia

The treatment of tularemia is a long and unpleasant procedure, so some measures must be taken to avoid getting it.
Prevention of infection is as follows:
The use of protective suits when going fishing, hunting. They will protect against bites of ticks, rodents and small insects. Clothing should be worn in such a way as to limit access to the body as much as possible: long sleeves, a turtleneck sweater, pants tucked into boots.
Acquisition of repellents – means that protect against the bites of ticks and horseflies.
On hikes, you need to take drinking water and in no case use unknown sources, because they can be contaminated.
Careful examination of the body after each visit to the forest areas for ticks. If it is present, you should immediately seek medical help and do not try to remove the tick yourself.
The risk of contracting tularemia increases in areas where wildlife populations are common and hunting for them is the main activity. In such places, vaccination against this disease is necessary.
The tularemia vaccine triggers the production of special antibodies, thus the human immune system, if the bacterium-causative agent of the disease enters the body, is able to destroy the harmful cell and stop the further development of the disease.
The vaccine preparation is dried live francisella tularensis bacteria. It is used in two ways: applied to the skin area or injected under the skin. Some time after the vaccination, swelling and redness form at the injection site. This is a normal reaction, indicating the process of formation of immunity to tularemia. If such a reaction is not observed, but there is a need for re-vaccination after 30 days.
Normally, one month after the introduction of the vaccine, a person becomes the owner of good immunity against the tularemia bacterium. The effect persists for 5 years, after which the vaccination is carried out again.
Tularemia is a disease transmitted from animals to humans. Cases when a person becomes infected from a person have not been established.
After a complete cure for tularemia, re-infection is impossible, because. immunity to such a disease is formed for life.









