Contents
Among all sexually transmitted infections, trichomoniasis should be singled out separately. This is a disease that is provoked not by a virus or a bacterium, but by a special microorganism – a protozoan, in Latin called Trichomonas vaginalis. This is one of the most common STIs, both in our country and around the world. The high incidence of T. vaginalis infection worldwide is not the biggest problem, as the infection is relatively well treated. The most serious problem is that trichomoniasis often co-occurs with other sexually transmitted diseases, including syphilis and HIV. Studies have shown that T. vaginalis infection is associated with an increased risk of contracting several STIs, including gonorrhea, human papillomavirus (HPV), and herpes simplex virus (HSV). And in women, trichomoniasis is also associated with poor pregnancy outcomes, infertility, postoperative infections, and cervical neoplasia.
If the expectant mother is infected with trichomoniasis, then T. vaginalis can be transmitted vertically (through the placenta or at birth) to the newborn, causing vaginitis, a urinary tract infection, or a respiratory infection that can be life-threatening. Humans are the only known host of T. vaginalis – animals do not get this infection.
What is trichomoniasis
Trichomoniasis is a sexually transmitted infection. It belongs to the group of parasitic diseases, caused by a microscopic parasite – Trichomonas. Women can get this infection several times in their lives, and in almost half of the cases it is an asymptomatic infection.
Causes of trichomoniasis in women
The main cause of the disease is infection with Trichomonas. T. vaginalis are approximately the size of white blood cells (about 10–20 µm long and 2–14 µm wide), although size can vary. Trichomonas have 4 flagella that protrude from the front of the body and 1 flagellum that extends back through the middle of the body to form a wavy membrane. According to these features, pathogens are distinguished in smears from other cells and pathogens.
In women, T. vaginalis is excreted from the vagina, cervix, urethra, bladder, Bartholin glands, and Skene glands.
The parasite resides both in the lumen and on the surface of the mucous membrane of the genitourinary tract and uses flagella to move through the tissues of the vagina and urethra. T. vaginalis has also been isolated from the rectum and detected by molecular methods in the respiratory tract, although these are not typical areas of infection. In cases of vertical transmission, T. vaginalis can infect the respiratory system of infants, however, little is known about this condition.
The parasite is usually found in the lower parts of the female genital tract and in the urethra, where it reproduces by dividing in half. It does not appear to be cyst-shaped and does not survive well in the outdoor environment. T. vaginalis is transmitted among humans, mainly through sexual intercourse.
The risk of contracting T. vaginalis infection is higher if you have:
- new or several partners at once;
- sexual contact with an infected partner;
- intimacy without a condom.
Symptoms of trichomoniasis in women
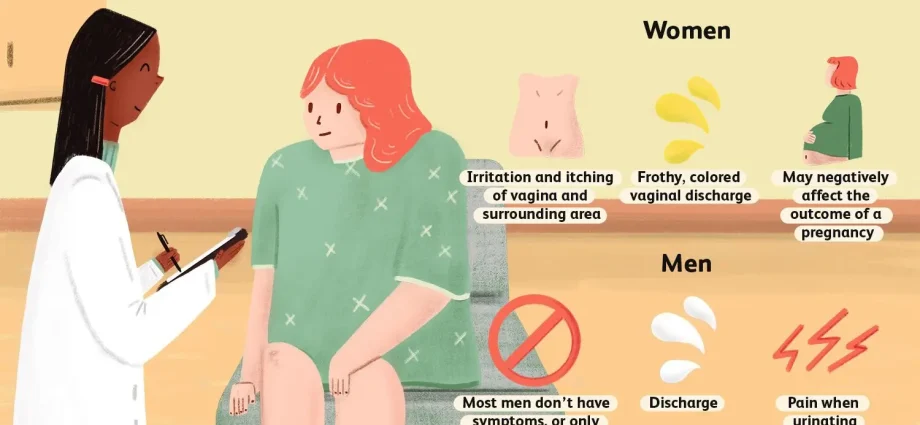
Women with trichomoniasis may be asymptomatic carriers of the infection, passing it on to their partners, or may experience a variety of symptoms that include vaginal discharge and vulvar irritation.
Despite the interaction of the immune system with T. vaginalis, infection creates immunity that is only partially protective at best, and there is little evidence that a healthy immune system prevents infection. Trichomoniasis symptoms usually occur after an incubation period of 4 to 28 days. The duration of asymptomatic infection in women is unknown. It was found that in mature women, the level of infection is significantly higher than in younger women, indicating that asymptomatic disease can continue in women for a long time.
In general, the symptoms of trichomoniasis in women vary significantly – from their complete absence to severe inflammatory diseases of the pelvic organs. Women with trichomoniasis often report abnormal vaginal discharge, which may be purulent, frothy, or bloody. Although frothy vaginal discharge is considered a classic manifestation of trichomoniasis, women with trichomoniasis also commonly complain to their doctor about:
- abnormal smell in the intimate area (often described as musty);
- vulvovaginal itching, burning, or soreness;
- dyspareunia (pain during intercourse), and often this is the main complaint;
- dysuria (pain when urinating);
- postcoital bleeding;
- pain in the lower abdomen.
In addition to the accompanying signs and symptoms, trichomoniasis can lead to cervicitis (inflammation of the cervix). It is characterized by two main features, namely:
- purulent discharge in the endocervical canal;
- easily occurring endocervical bleeding with spotting on linen.
T. vaginalis infection is also one of the top three causes of vaginitis. Vaginitis is usually characterized by vaginal discharge with one of the following:
- itching of the vulva;
- irritation;
- smell.
The other two most common causes of vaginal discharge are anaerobic bacterial overgrowth of normal flora (bacterial vaginosis) and candidiasis (Candida albicans infection).
Treatment of trichomoniasis in women
It is believed that trichomoniasis is poorly diagnosed due to various factors, including the lack of accurate testing, low sensitivity of the commonly used diagnostic method (wet mount microscopy), and non-specific symptoms. Self-diagnosis and self-medication or diagnosis by practitioners without adequate laboratory testing can also contribute to misdiagnosis.
Numerous molecular detection methods are currently being developed to diagnose trichomoniasis, including several validated nucleic acid amplification tests (NAATs) and an antigen detection test.
Diagnostics
Testing for T. vaginalis infection is recommended for all women who see a doctor with complaints of vaginal discharge. In addition, screening for T. vaginalis in women at high risk of STIs is indicated.
Modern treatments
Doctors recommend two oral drugs from the Nitroimidazole group for the treatment of trichomoniasis: Metronidazole and Tinidazole. Although tinidazole is generally more expensive, it causes fewer side effects than metronidazole and is equally effective or superior in suppressing T. vaginalis infection. When one prescribed drug is ineffective (and reinfection by the partner is ruled out), another Nitroimidazole or an alternative dosing regimen of Metronidazole can be used. Topical preparations of Metronidazole and other antimicrobials are not effective and should not be used to treat trichomoniasis.
Prevention of trichomoniasis in women at home
Sexual partners of an infected woman should also be treated with her. Both the patient and partners should abstain from sexual activity until pharmacological treatment is completed and they have no symptoms.
Infected women who are sexually active have a high rate of reinfection. Thus, rechecking 3 months after treatment is a way to rule out infection.
Trichomoniasis can usually be treated quickly and effectively. Single-dose regimens with Metronidazole resulted in cure rates of 90% to 95%, while single-dose regimens with Tinidazole resulted in cure rates of 86% to 100%.
Popular questions and answers
Regarding the diagnosis and treatment of trichomoniasis in women, the characteristics of the transmission of infection, we talked with urologist, specialist in ultrasound diagnostics, doctor of the highest category of the Center for Disaster Medicine Yuri Bakharev.
Is it possible to get trichomoniasis through everyday life?
Is it possible to treat trichomoniasis with folk remedies?
What are the complications of trichomoniasis in women?
T. vaginalis infection is also closely associated with the presence of other STIs, including gonorrhea, chlamydia, and sexually transmitted viruses. T. vaginalis infection has even been shown to increase a patient’s susceptibility to sexually transmitted viruses, including herpes simplex virus, human papillomavirus, and HIV. People with trichomoniasis are twice as likely to develop HIV infection than the general population.
Women can have various other complications associated with trichomoniasis. There is a known higher risk of pelvic inflammatory disease in women with trichomoniasis. The risk of tubal infertility doubles. Trichomoniasis may also play a role in cervical neoplasia and postoperative infections. Pregnant women with T. vaginalis infection are at particularly high risk for adverse outcomes, which may include the following:
● premature birth;
● low birth weight babies;
● premature rupture of membranes;
● intrauterine infection;
● Respiratory or genital infection with T. vaginalis in a newborn.
T. vaginalis infection may also increase the likelihood of vertical transmission of HIV due to destruction of the vaginal mucosa.