Contents
- Basic therapy for rheumatoid arthritis
- Cytostatics: drugs that suppress the immune system
- Treatment of rheumatoid arthritis with antimalarial drugs
- Treatment of rheumatoid arthritis with sulfonamides
- Treatment of rheumatoid arthritis with D-penicillamine
- Basic therapy: main conclusions
- Treatment of rheumatoid arthritis with non-steroidal anti-inflammatory drugs
- Treatment of rheumatoid arthritis with selective anti-inflammatory drugs
- Treatment of rheumatoid arthritis with corticosteroids
- Physico-mechanical methods of treatment of rheumatoid arthritis
- Topical treatment of active rheumatoid arthritis
- Physiotherapy treatment of rheumatoid arthritis
- Dietary advice for patients with rheumatoid arthritis

Rheumatoid arthritis is a serious disease that a person has to deal with from the moment of diagnosis for the rest of his life.
Treatment is complex, and includes a number of drugs and techniques:
basic therapy;
Anti-inflammatory therapy of several types;
Selective anti-inflammatory drugs
Treatment with corticosteroids (hormones)
Physical, mechanical, physiotherapeutic effects;
Local treatment (injections, laser, cryotherapy);
Special diet.
Let’s start our conversation with basic therapy, since, as the name implies, it is the basis of the treatment of rheumatoid arthritis, and every patient with this serious disease has to deal with it.
Basic therapy for rheumatoid arthritis
Why is the word “basic” in the title? Mainly, not because it is the main method of treatment, but because drugs from this group affect the very essence of rheumatoid arthritis, that is, its “basis”. They do not cause relief of well-being after a few days or even weeks after the start of the reception. These drugs give a pronounced effect not earlier than after a few months, and they are taken in the hope of slowing down the course of the disease, or better, driving RA into deep remission.
A long wait for the result is not the only disadvantage of basic therapy. Each of the drugs included in it is effective in its own way. But the reaction of different patients is different, so when drawing up a treatment plan, a rheumatologist has to rely not only on medical statistics. You need to include your medical intuition and evaluate each patient as an individual.
Modern basic therapy includes five groups of drugs:
Immunosuppressants
Antimalarial;
Sulfonamides;
D-penicillamine;
Let’s consider in detail the pros and cons of each of the five components of basic therapy and try to understand how to achieve the best effectiveness and good tolerability of the treatment of rheumatoid arthritis.
Cytostatics: drugs that suppress the immune system

The shorter word “cytostatics” usually refers to drugs from the group of immunosuppressants (remicade, arava, methotrexate, cyclosporine, azathioprine, cyclophosphamide, and many others). All of these drugs suppress cellular activity, including the activity of immune cells. As you know, rheumatoid arthritis is autoimmune in nature, so it is not surprising that it is treated with cytostatics. And the technique itself was adopted by rheumatologists from oncologists who are fighting with the help of cytostatics with another terrible threat – cancer.
It was cytostatics, and primarily methotrexate, that moved gold from its leadership position in the treatment of RA. Immunosuppressants successfully treat not only rheumatoid arthritis, but also psoriatic arthritis. The drugs of this group currently form the basis of the basic therapy for RA. This fact itself often frightens patients, because it is scary to lose immunity almost completely. But keep in mind that much lower doses of cytostatics are used in rheumatology than in oncology, so you should not be afraid of such terrible side effects as are observed in cancer patients.
Advantages and disadvantages of immunosuppressants
The first advantage of cytostatics is their high efficiency at a relatively low dosage. Patients with rheumatoid arthritis are prescribed a 5-20 times lower dose of immunosuppressants than patients with oncology, but in almost 80% of cases this is enough to achieve an excellent therapeutic effect. Best of all, cytostatics have proven themselves in the treatment of severe rheumatoid arthritis with a high rate of progression of the disease.
The second undoubted plus in favor of taking cytostatics is the low frequency and low severity of side effects. Only a fifth of patients complain of unpleasant symptoms:
skin rash;
loose stools or constipation;
Difficulty urinating;
Sensation as if goosebumps run over the skin.
As soon as the drugs are discontinued or the dosage is adjusted, these side effects disappear by themselves. For prevention, once a month, blood and urine tests are taken from the patient in order to notice the problem in time. Possible failures in the work of the kidneys, liver and oppression of hematopoiesis. But usually cytostatics are well tolerated, and already a month after the start of therapy, improvements in the condition of a patient with rheumatoid arthritis are visible.
For the treatment of rheumatoid arthritis, modern rheumatologists use three immunosuppressant drugs: methotrexate, Arava and Remicade. Let’s look at the advantages and disadvantages of each of the drugs.
Methotrexate
Earlier, we have already mentioned methotrexate several times, and this is not accidental, because this cytostatic is the recognized leader in the basic therapy of RA. It is very convenient to take it: once a week, the patient needs to drink one capsule with a dosage of 10 mg. Usually the doctor and the patient agree on which day of the week they will now have “methotrexate” for many months. For example, on Mondays or Thursdays, the patient will now have to take these pills, so it is difficult to confuse or forget.
You can usually talk about improving well-being after 4-6 weeks from the start of taking the drug, and about persistent and pronounced progress in treatment – after 6-12 months. There is one important note: on the “methotrexate” day, you can not take NSAIDs, which in most cases are also included in the basic therapy for RA. On any other day of the week, you can safely continue treatment with non-steroidal anti-inflammatory drugs.
Arava (leflunomide)
Arava is considered a very promising immunosuppressant, and many rheumatologists are switching their patients to this new drug. But there are also doctors who consider Arava to be a heavier drug with worse tolerance than methotrexate. In general, it can be said that Arava is prescribed as an alternative to methotrexate if the latter caused side effects in the patient.
Arava is recommended for patients with a very rapid course and rapid development of rheumatoid arthritis, when serious joint problems appear already in the first year of the disease, up to loss of mobility. Approximately a month after the start of the reception, the first positive changes are usually visible, and after six months – a stable improvement in the condition of the bones.
Remicade (infliximab)
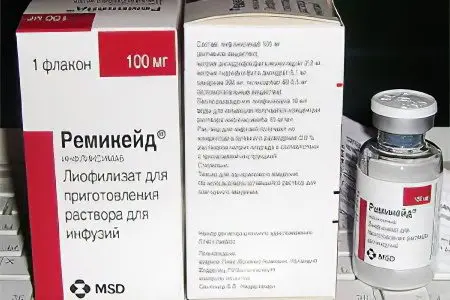
Another novelty in the arsenal of rheumatologists is Remicade.
It differs from methotrexate, Arava, and other immunosuppressants in two ways:
Amazing speed;
Very high cost.
Given the latter feature, remicade usually acts as something of a lifeline for patients with severe, rapidly progressive rheumatoid arthritis, who are absolutely not helped by methotrexate and other affordable cytostatics. Two more reasons for replacing methotrexate with remicade are poor tolerance and the need for an urgent reduction in the dose of corticosteroids, which are also part of the basic therapy for RA. As you can see, there are enough reasons for prescribing Remicade, but sometimes they are all outweighed by the high cost of the drug.
The high efficiency and speed of action of Remicade has a downside: this medicine has many side effects and contraindications. Before you start taking the drug, you need to carefully examine the patient and heal absolutely all the inflammatory processes found in him, even hidden and sluggish ones. Otherwise, after the start of therapy in conditions of depressed immunity, all these infections will “raise their heads” and lead to serious problems, up to sepsis.
With possible side effects, including an itchy rash, it is recommended to preventively deal with antihistamines. It is very important for women to carefully protect themselves while taking Remicade, since both pregnancy and breastfeeding are absolutely impossible during this period. Moreover, you can think about motherhood at least six months after the end of Remicade treatment.
Other cytostatics
Of course, there are other immunosuppressive drugs, including more affordable ones:
Cyclosporine;
Chlorbutin;
Azathioprine;
Cyclophosphane.
But all these drugs during clinical trials did not show their best side – the frequency of side effects is very high, moreover, complications, as a rule, are more serious than when taking the same methotrexate. Therefore, the rejection of the three most popular cytostatics in the basic therapy of RA is expedient only if they have no effect or are poorly tolerated.
Treatment of rheumatoid arthritis with antimalarial drugs

Delagil (Rezoquin, Chloroquine, Chingamine) and Plaquenil (Hydrochlorin, Hydroxychlorin) have long been used in medicine as a remedy for a tropical disease – malaria. But what about rheumatoid arthritis, you ask. The fact is that in the middle of the last century, scientists who were looking for at least some new and effective drug for the treatment of RA tried almost all types of anti-inflammatory drugs, because rheumatoid arthritis for a long time was considered just a special type of infection. One of these studies brought good news – delagil and plaquenil slow down the course of RA and reduce the severity of its manifestations.
Nevertheless, antimalarial drugs in the modern basic therapy of RA occupy, perhaps, the most modest place, since they have only one advantage – good tolerability. And they have one drawback, moreover, a very serious one – they act very slowly (improvement occurs only after six months or a year) and even if successful, they give a weak therapeutic effect.
Why didn’t doctors abandon antimalarial therapy?
A logical question, because there are drugs that act faster and work better. But medicine is one of those branches of science where prejudices and the elemental force of inertia are very strong. Thirty years ago, the basic therapy for RA was based on the following principle: first delagil and plaquenil, then gold, if it doesn’t help, D-penicillamine or immunosuppressants, and if nothing helps, corticosteroids. That is, the direction was chosen from the most harmless to the most potentially dangerous. But if you think about it, such a principle of building basic therapy is criminal in relation to the patient.
Suppose a person has acute, rapidly developing rheumatoid arthritis with severe pain and rapidly degrading joints. Is it reasonable to wait six months for antimalarial drugs to work (the question is, will they work?), if stronger and more effective drugs can be prescribed? Even if there are side effects, it’s better than just watching a person suffer, and how the condition of his joints deteriorates catastrophically every day.
But there are, nevertheless, cases when antimalarial drugs are still relevant:
The patient very poorly tolerates all other drugs from the basic therapy for RA;
Drugs considered more effective did not give any effect;
Rheumatoid arthritis is very mild and develops slowly, so there is no need to resort to the strongest, but dangerous remedies.
Treatment of rheumatoid arthritis with sulfonamides

Salazopyridazine and sulfasalazine are two sulfonamide drugs that have been successfully used in the treatment of rheumatoid arthritis.
If you try to create a certain hit parade in terms of effectiveness among drugs for basic therapy for RA, then it will look something like this:
In the first place – methotrexate;
On the second – gold salts;
On the third – sulfonamides and D-penicillamine;
Fourth, antimalarial drugs.
Thus, sulfonamides cannot be considered among the leaders in terms of efficiency, but they have huge advantages:
Good tolerability (incidence of side effects – 10-15%);
Low severity of complications, if any;
Доступная цена.
The disadvantage of sulfonamides is only one, but significant – they act slowly. The first improvements are visible only three months after the start of treatment, and stable progress is usually observed after a year.
Treatment of rheumatoid arthritis with D-penicillamine
D-penicillamine (distamine, kuprenil, artamine, trololol, metalcaptase) is almost never included in the basic therapy for RA if the patient tolerates methotrexate well. It is somewhat inferior to the listed drugs in terms of effectiveness, but significantly exceeds them in the number of possible side effects, the frequency of their occurrence and the severity of complications. Therefore, the only reason for prescribing D-penicillamine is the lack of progress in treatment with gold and methotrexate, or their poor tolerance.
D-penicillamine is a highly toxic substance that causes negative side effects in almost half of the cases of treatment of seropositive rheumatoid arthritis, and a third of cases of treatment of seronegative RA. Why is it still being used by doctors?
Because sometimes there is simply no other way out. Tried cytostatics, no result. Or had to be canceled due to poor portability. And the disease progresses quickly. Then the rheumatologist has only one, albeit dangerous, but, in fact, the only strong drug in his arsenal – D-penicillamine. This is exactly the situation when the end justifies the means. If there is a negative reaction of the body, the medicine can always be canceled. Therefore, it is better to appoint it after all than to do nothing at all.
D-penicillamine also has an ace up its sleeve – this drug helps well those patients in whom RA has given complications to the heart, kidneys or lungs – for example, amyloidosis has developed. With satisfactory tolerance, D-penicillamine is taken for 3-5 years in a row, then they take a break for a couple of years and repeat the course. In this case, the medicine does not lose its effectiveness, as, for example, gold salts, which are better not to cancel for a long period. Unfortunately, in a small part of patients (approximately 10%), after a temporary improvement in well-being, a sharp deterioration occurs.
Basic therapy: main conclusions

We have considered the pros and cons of all five groups of drugs included in the list of so-called basic therapy for rheumatoid arthritis. In this story, phrases about complications, side effects and dangers flashed so often that one involuntarily wants to ask – what kind of mandatory treatment for rheumatoid arthritis is it, if it heals on the one hand (and even then not always), and on the other hand cripples (almost always )?
Such a question, of course, visits the heads of all patients with rheumatoid arthritis immediately after making a disappointing diagnosis. Many sit on medical forums and listen to angry rebukes there, the essence of which can be formulated in one sentence: “I became a victim of a medical error, and in general, doctors themselves do not know how to treat rheumatoid arthritis.” This statement is not far from the truth in that part of it, which speaks of ignorance. Because to know exactly how to cure a person from a serious illness of an inexplicable nature, only the Lord God can know.
The selection of drugs for basic therapy for each individual patient with rheumatoid arthritis takes an average of about six months. Finding the most suitable medicine in a shorter period of time is almost impossible, no matter how professional the rheumatologist is, and no matter how brutal his instincts are. And to predict how the drugs will be transferred is generally not given to anyone.
So maybe not to start this basic therapy? Why torture a person? Well, yes, let the disease develop as quickly as possible so that the person dies early, then he will certainly stop suffering. Practice shows that if basic therapy is started immediately, immediately after the diagnosis, then there is more than a decent chance to slow down the course of the disease or even achieve a stable remission. But cases when a patient with rheumatoid arthritis did not receive any treatment and suddenly recovered, medicine does not know.
Think for yourself, if there is even a small chance to prolong your life or the life of a loved one, will you begin to think about side effects? The disease itself will arrange for you such side effects that the drugs never dreamed of, and very soon.
Treatment of rheumatoid arthritis with non-steroidal anti-inflammatory drugs

Non-steroidal anti-inflammatory drugs, we will further on the story call the abbreviation NSAIDs, it’s more convenient. This group includes:
Ibuprofen (nurofen);
Diclofenac;
Ketoprofen (ketorolac, Ketanov);
Indomethacin;
Butadione;
Piroxicam.
In the treatment of rheumatoid arthritis, these drugs act as an ambulance for joint pain. They reduce not only pain, but also inflammation in the articular and periarticular tissues, so their intake is advisable in any case. Why did we not include diclofenac or ibuprofen in the group of drugs for the basic therapy of RA? Because they do not treat the disease itself and do not slow down its development in any way. They act symptomatically, but at the same time qualitatively improve the life of a patient with rheumatoid arthritis.
Of course, you have to take NSAIDs constantly, and with long-term use, rarely any medicine does not give side effects. That is why it is important to choose the right NSAID for a particular patient and use the drug wisely without exceeding the dosage. We will talk about how to do this further.
Criteria for choosing NSAIDs
The first criterion is toxicity, therefore, first of all, RA patients are prescribed the least toxic NSAIDs, which are rapidly absorbed and rapidly excreted from the body. First of all, these are ibuprofen, ketoprofen and diclofenac, as well as the selective anti-inflammatory drug movalis, which we will discuss in detail below. Ketorolac, piroxicam and indomethacin are excreted from the body longer, in addition, the latter can cause mental disorders in elderly patients. That is why these three drugs are usually prescribed to young patients who do not have problems with the liver, kidneys, stomach and heart. Then the likelihood of side effects and complications is low.
The second criterion is the effectiveness of NSAIDs, and everything is very subjective. A patient with rheumatoid arthritis usually takes each of the drugs recommended by the doctor for a week in order to evaluate the result according to his feelings. If a person says that everything hurts from diclofenac, but ibuprofen helps well, the doctor usually agrees with this.
Speaking of subjectivity, one cannot fail to note the power of suggestion, which the usual instructions for the drug have. So, many patients, after reading the annotation for diclofenac, where all its possible side effects are honestly and frankly described, clutch their heads in horror and say that they will never drink such pills. In fact, diclofenac is no more dangerous than aspirin, which people drink almost handfuls for any reason. It’s just that aspirin doesn’t have a box with detailed instructions inside.
In summary, let’s say that when evaluating the effectiveness of NSAIDs, you need to take into account not only your feelings (helps / does not help), but also the data of regular examinations that demonstrate the general condition of your body and diseased joints in particular. If there are side effects (the work of the internal organs has worsened), and the joints become more and more inflamed, it makes sense to switch to another NSAID on the advice of a doctor.
Treatment of rheumatoid arthritis with selective anti-inflammatory drugs

This group of drugs includes movalis, a relatively new drug that was created specifically for long-term continuous use in order to minimize possible side effects. Returning to the subjectivity of assessments, let’s say that most RA patients find movalis no less, and sometimes even more effective pain reliever. At the same time, movalis is very well tolerated and rarely causes negative reactions of the body, which cannot be said about NSAIDs, which are often accompanied by digestive disorders.
Under the supervision of a physician, Movalis can be taken for several months or even years in a row, if necessary. It is also very convenient that one tablet is enough to relieve pain, which is drunk either in the morning or at bedtime. There is also movalis in the form of rectal suppositories. If the pain syndrome is very intense, you can resort to movalis injections. During an exacerbation of rheumatoid arthritis, the patient often has to take injections for a whole week, and only then switch to pills. But I am glad that Movalis, firstly, helps almost all patients, and secondly, it has almost no contraindications.
Treatment of rheumatoid arthritis with corticosteroids
Another “fire” and symptomatic method of alleviating the condition of patients with rheumatoid arthritis is taking corticosteroid hormonal preparations (hereinafter – corticosteroids).
These include:
Prednisolone (medopred);
Methylprednisolone (Medrol, Depo-Medrol, Metipred);
Triamcinolol (triamcinolol, polcortolone, kenalog, kenacort);
Betamethasone (Celeston, Flosteron, Diprospan);
Dexamethasone
Corticosteroids are very popular in the West, where they are prescribed to almost all patients with RA. But in our country, doctors are divided into two opposing camps: some advocate taking hormones, while others vehemently reject this technique, calling it extremely dangerous. Accordingly, patients who want to be aware of all the news from the world of medicine read interviews with American and Russian rheumatologists and are confused: who to believe? Let’s try to figure it out.
Taking corticosteroids causes a rapid improvement in well-being in patients with RA: pain disappears, stiffness of movements and chills in the morning disappear. Of course, this cannot but please a person, and he automatically assigns the status of a “professional” to the attending physician. The pills helped – the doctor is good, they did not help – the doctor is bad, everything is clear here. And in the West, a feeling of gratitude to a doctor is usually expressed in monetary terms. That is why there are many more “good” doctors than “bad” ones.
In our country, in conditions of free medical insurance, the doctor will think three times before prescribing hormones to his patient. Because time will pass, and the same doctor, most likely, will have to disentangle the consequences of such therapy.
The dangers of hormone therapy
Why is taking corticosteroids so dangerous? These are stress hormones that have a powerful negative effect on all organs. While a person takes them, he feels great, but one has only to stop, and the disease is activated with a triple force. If earlier the joints hurt so much that it was quite possible to endure, now they hurt unbearably, and nothing helps.
So maybe keep the patient on hormones all the time? This is absolutely excluded, because, firstly, over time, they will bring less and less effect, and secondly, the negative impact on the internal organs will accumulate and sum up until it leads to a serious failure.
Here are just a few of the likely consequences:
Itsenko-Cushing’s syndrome – terrible edema and hypertension as a result of too slow removal of sodium and fluid from the body;
An increase in blood sugar levels, and, as a result, diabetes mellitus;
Obesity;
Decreased protective properties of the body, frequent colds;
Development of peptic ulcer of the stomach and / or duodenum;
Thrombosis of veins and arteries;
Amenorrhea and dysmenorrhea;
Hemorrhagic pancreatitis;
Acne;
Moon-shaped oval of the face;
Convulsive seizures and psychoses;
Insomnia and uncontrolled excitement of the nervous system.
Terrible list, isn’t it? Usually, when at least one serious side effect appears, corticosteroids are immediately canceled, but here the worst begins – the body protests against the cancellation. This is expressed in a wave-like increase in the inflammatory process in the articular and periarticular tissues and severe pain that cannot be relieved by anything. Hormones try to cancel gradually to avoid such shock consequences.
To drink or not to drink hormones?
But how to drink them, if it threatens with such terrible consequences, you ask. Indeed, corticosteroids at some stage will necessarily cease to bring relief and begin to harm the patient. But there are situations when you have to choose the lesser of several evils. Sometimes the patient is worse than ever, and, moreover, only hormones can alleviate his condition. We are talking about patients with Still’s syndrome, Felty’s syndrome, polymyalgia rheumatica and other severe complications.
A reasonable and far-sighted specialist will prescribe hormones only to such a patient whose rheumatoid arthritis is at a very high stage of activity, ESR goes off scale, the level of C-reactive protein in the blood is outrageous, and the inflammatory process is not stopped with NSAIDs.
The conclusion is as follows: corticosteroids should be prescribed to a patient with rheumatoid arthritis if the expected benefit from the treatment outweighs the likely harm.
Physico-mechanical methods of treatment of rheumatoid arthritis

Such techniques include drainage of the thoracic lymphatic duct, lymphocytophoresis, plasmaphoresis, and irradiation of lymphoid tissue. Each of these procedures is quite effective, but has a number of disadvantages. Let’s consider them in detail.
Drainage of the thoracic lymphatic duct
This procedure requires sophisticated medical equipment. The doctor, using a drainage apparatus, penetrates the patient’s thoracic lymphatic duct, pumps out all the lymph from there, places it in a special centrifuge that rotates and separates the contents into pure lymph and cellular decay products, waste products of microbes and other “garbage”. Completely purified lymph is pumped back into the thoracic duct.
A couple of weeks after this procedure, the patient begins to feel much better, but this effect lasts only for a month. Then the purified lymph is again filled with harmful impurities, because the disease has not disappeared anywhere. That is why thoracic lymphatic duct drainage is almost never used in modern practice in the treatment of rheumatoid arthritis. The procedure is complex, expensive, but the effect of it remains for a too modest period of time.
Lymphocytophoresis
This procedure is also very expensive and is carried out on high-tech medical equipment in large medical centers. The doctor, as it were, “cuts” into the patient’s circulating bloodstream so that the blood passes through a special centrifuge, and there monocytes and lymphocytes are removed from it. For four hours, during which lymphocytophoresis is performed, approximately 12120 lymphocytes can be removed from the patient’s bloodstream.
Why is it needed, and what does it give? Lymphocytes, or cells of the immune system, are the companions of the inflammatory process. This is why a rheumatologist is never happy to see elevated lymphocyte levels in your blood test results. If at least some of these cells are removed from the bloodstream, the health of the RA patient will immediately improve. True, this effect, as in the previous case, will last only about a month. That is why lymphocytophoresis is used extremely rarely.
Plasmaphoresis
The plasmaphoresis procedure lasts about six hours, during which plasma containing harmful components is removed from a large volume of the patient’s blood: inflammatory mediators, aggressive immune cells, rheumatoid factor, waste products of bacteria. “Bad” plasma is replaced by donor or albulin. In just one procedure, it is possible to remove 40 ml of plasma from the body for each kg of the patient’s weight. Plasmaphoresis is carried out in courses of 15-20 procedures, the treatment takes about one and a half months.
Why such suffering? Plasmaphoresis greatly reduces the ESR and ROE, reduces the amount of immunoglobulins in the blood, and the patient begins to feel much better. True, negative consequences are also possible: edema, a decrease in hemoglobin, potassium deficiency. The side effects are manageable and the benefits outweigh the risks.
The main disadvantages of plasmaphoresis are its high cost and short duration of the therapeutic effect. A positive result persists for several months, and then the course has to be repeated. Nevertheless, plasmophoresis is often resorted to, especially in case of sudden acute development of rheumatoid arthritis and in the case when the choice of drugs for basic therapy is delayed. It is plasmophoresis that allows the attending physician to gain time and prevent a fatal deterioration in the patient’s condition.
Irradiation of lymphoid tissue
The technique of irradiating lymphoid tissue was first applied in 1980, and has been actively used since then. Its essence is to expose the lymph nodes, spleen and thymus of the patient to point irradiation. In one session, the patient receives from 150 to 220 rads, in total for the course of treatment – 4000 rads. In almost all cases, the treatment is effective and allows you to reduce the dose of corticosteroids and NSAIDs, or even stop them altogether. The effect persists for a long time – 1-2 years.
Like any radiation therapy, irradiation of lymphoid tissue has side effects. Some patients have general weakness, nausea, and a decrease in the level of leukocytes in the blood. Nevertheless, this procedure is successfully used for the treatment of rheumatoid arthritis, both in our country and in the West.
Topical treatment of active rheumatoid arthritis

It is possible to alleviate the condition of a patient with rheumatoid arthritis in the active stage with the help of hormonal injections into the joint capsule, laser therapy, cryotherapy, special ointments and creams. Consider the advantages and disadvantages of each method.
Intra-articular administration of corticosteroids
The essence of the technique lies in the injection into the joint cavity of hormonal drugs from the group of corticosteroids (we talked about them above). It can be prednisolone, celeston, hydrocortisone, depo-medrol, diprospan, flosteron or kenalog. After the procedure, a quick and pronounced positive effect is observed: the inflammation subsides, the pain decreases or even disappears completely.
Corticosteroid injections are a “first aid” for diseased joints. The introduction of hormones directly into the joint is done when the patient’s health is very deplorable, and no other measures, including taking NSAIDs and movalis, help relieve pain and reduce inflammation. Usually, after the injection, the patient feels well within a month, but in severe cases, the procedure has to be repeated every 10 days. More often it is impossible, otherwise corticosteroids will begin to adversely affect the body as a whole.
In addition, doctors strongly discourage hormonal injections into the same joint more than eight times. This can cause destructive changes in the cartilage, ligaments, and muscles around the joint. It turns out that for a temporary improvement in well-being, the patient will have to pay an exorbitant price.
Laser therapy
Laser beams have a beneficial effect on the body of a person suffering from rheumatoid arthritis at any stage of activity. If an exacerbation of the disease is currently observed, the patient’s elbow bends are irradiated with a laser. In this way, they improve the quality of blood, and also provide a more complete blood supply to organs and tissues. It is believed that laser beams also normalize the immune status of RA patients. This technique is successfully used both independently and in combination with basic therapy, which we wrote about above.
When the period of exacerbation of the disease has passed, an acute inflammatory process is not observed in the patient’s body, the body temperature is not elevated, it is possible to irradiate the area of u80buXNUMXbthe joints with a laser. In the first weeks after the procedures, there may be a temporary deterioration in well-being and an increase in pain. However, then in XNUMX% of patients there is an improvement, which persists for several months.
The course of treatment usually consists of 15-20 procedures, and they are carried out with an interval of one day. Laser irradiation will do little to help patients in the last stages of rheumatoid arthritis – paralyzed, with twisted joints. However, in the initial stages and during periods of remission, such an effect is very effective and simply useful.
There are several important contraindications to laser irradiation:
The presence in the body of any tumors, including benign ones;
Blood diseases, for example, poor clotting;
Infectious diseases (tuberculosis, syphilis);
Hypertensive crisis;
Myocardial infarction;
Cirrhosis of the liver;
Stroke.
Cryotherapy

Cryotherapy, or cold treatment, is successfully used not only in the treatment of arthritis (rheumatoid, reactive, psoriatic), but also in the treatment of ankylosing spondylitis. This method is good both at the stage of exacerbation and during periods of attenuation of the disease. Almost 80% of RA patients treated with cryotherapy notice a significant improvement in their well-being. The main thing is to be consistent, and undergo procedures regularly for a long time.
Cryotherapy can be dry, this is when the body is exposed to dry air of very low temperature, for example, in a special cryosauna. And maybe liquid cryotherapy – in this case, the patient is exposed to liquid nitrogen. Let’s start with the second option.
A jet of liquid nitrogen is released onto the diseased joint under high pressure, which immediately evaporates, but at the same time has time to deeply cool the tissues. Inflammation in them subsides, blood circulation increases, swelling decreases and pain disappears. Usually, 8-12 such procedures are carried out every day or every other day in order to achieve a lasting positive effect. Cryotherapy with liquid nitrogen has almost no contraindications, it can be used even in the treatment of elderly patients with RA. There are only a few restrictions – Raynaud’s syndrome, severe arrhythmia, a recent heart attack or stroke.
Now let’s talk about dry cryotherapy. The patient is completely undressed and placed in a cryosauna – a room filled with super-cold dry air. The principle of therapeutic effect here is the same as when blowing liquid nitrogen, however, cryosauna has a positive effect on the entire body, and not just on individual joints. Such a procedure is carried out in special medical centers, usually private, so it is not cheap. In addition, dry cryotherapy requires rare, expensive equipment, so even if public hospitals were equipped with cryosaunas, they would hardly be free to use.
Healing creams and ointments
Advertising promises us a miraculous relief from joint pain, but miracles do not happen. For rheumatoid arthritis, ointments and creams based on the same NSAIDs are recommended:
Butadion ointment;
Indomethacin ointment;
Fastum-gel;
Voltaren-emulgel;
Dolgit.
If you smear the diseased joint with such an ointment, about 5-7% of the active substance will penetrate through the pores of the skin. Will it bring great relief? Hardly. However, if you are taking NSAIDs by mouth, like most patients with rheumatoid arthritis, then the ointment can be used as a support, that is, just to enhance the effect. Creams and ointments for joint pain have only one indisputable advantage – they are almost harmless (I wanted to say, almost useless).
Physiotherapy treatment of rheumatoid arthritis
What is good for arthrosis is unacceptable for arthritis, so physiotherapy and massage are prescribed only during periods of remission, when there is no acute inflammatory process. If the patient has a high temperature and the joints literally burn, what kind of massage or warming can we talk about?
But when the inflammation has managed to stop, some sparing types of massage, as well as physiotherapy, can help improve the blood supply to the joints and restore their mobility.
In the treatment of rheumatoid arthritis in remission, the following physiotherapy procedures are used:
Diathermy;
infrared irradiation;
Applications with paraffin, ozocerite and therapeutic mud;
Phonophoresis with hydrocortisone;
X-ray therapy.
The doctor should choose the method of therapeutic therapeutic effect. It is absolutely unacceptable when a patient with rheumatoid arthritis goes to a private spa center to enjoy therapeutic mud there. The advice of various healers and natural healers is also absolutely impossible to follow. And massage at home should not be carried out by a person who does not have the appropriate qualifications and who does not know how to deal with joints affected by rheumatoid arthritis.
Dietary advice for patients with rheumatoid arthritis

Proper nutrition is simply of great importance for a patient with RA. Almost all patients note that the use of certain products that irritate the body leads to a sharp deterioration in well-being, exacerbation of inflammation and increased pain. And as soon as the harmful product is excluded, the situation immediately returns to normal.
What are these dangerous products? Here is the list:
Pork;
Citrus;
Some cereals (wheat, oats, corn, rye);
Milk and dairy products.
As you can see, the blacklist contains foods that are usually considered healthy (with the possible exception of pork). But do not be upset, patients with rheumatoid arthritis have a good alternative:
Fish and seafood;
Vegetables and fruits (with the exception of citrus fruits);
Chicken and quail eggs;
Buckwheat and barley porridge.
You need to cook food in a healthy way: in the oven or double boiler, you can boil or stew. It is recommended to eat often: 5-6 times a day, but in small portions. Don’t eat at night. It is advisable to exclude salt and sugar from the diet. Avoid smoked and fried foods. Some patients with rheumatoid arthritis even have to get special advice from a nutritionist and develop an individual diet to avoid complications caused by malnutrition.
[Video] Dr. Berg – 7 Remedies to Fight Rheumatoid Arthritis:









