Contents

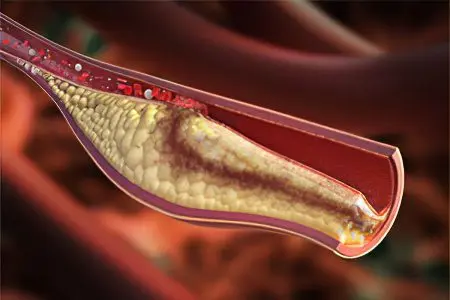
Thrombosis of the internal jugular vein is an acute disease of the main venous vessel, which is caused by the formation of a blood clot in its lumen. As a result of impaired blood flow, an increase in intravenous pressure occurs, transcapillary exchange is disturbed.
The internal jugular vein is located in the neck. Therefore, its thrombosis is always accompanied by the occurrence of pain in this area, the formation of edema, blue skin. Thrombosis of the jugular vein refers to pathological conditions that require emergency medical care.
In total, there are three pairs of jugular veins in the human body (internal, external and anterior). It is the internal pair of jugular veins that is the largest of all the others. She is responsible for supplying blood to the skull.
Thrombosis of this vein is not so common, however, this does not reduce the significance of the pathology. In the general system of thrombosis, the internal jugular vein suffers in 5% of cases. By itself, jugular vein thrombosis rarely leads to the death of the patient, but with the development of its complications in the form of thrombus embolism, this scenario is quite possible. Therefore, it is important to know the signs of the disease and seek medical help in a timely manner.
Causes of jugular vein thrombosis
The most common reason for the formation of jugular vein thrombosis is exogenous interventions, namely, the placement of a catheter during infusion therapy.
Thrombosis develops at a time when the patient is in a hospital, but sometimes the symptoms of this pathology are hidden. Indeed, during the course of therapy, most patients receive antiplatelet agents and anticoagulants. Therefore, acute thrombosis of the jugular vein is observed after discharge from the hospital.
Other reasons
Other causes of jugular vein thrombosis include:
Mechanical compression of the vein.
Features of the anatomical structure of the human skeleton.
Heavy physical activity.
Installing a pacemaker.
The patient undergoing radiation therapy.
Virchow’s triad as a cause of the formation of thrombosis of the internal jugular vein. It includes:
Damage to the inner layer of the vein, for example, when the catheter is in it for a long time. Sometimes these disorders are characteristic of people who inject drugs.
Slowing of blood flow in the vein, which may be due to the presence of a tumor that compresses the vein.
Violation of blood clotting, for example, against the background of chronic or acute diseases.
Risk Factors
In addition to the main causes of jugular vein thrombosis, there are additional risk factors that increase the likelihood of its occurrence. These include:
old age.
Overweight.
Infectious diseases that have the ability to damage the venous wall.
Bad habits: drug addiction, smoking, alcohol abuse.
Postponed surgical interventions on the neck.
Diseases of the cardiovascular system.
Kidney damage.
Menopause in women.
Uncontrolled intake of oral contraceptives.
Hypodynamia.
Systemic diseases of the body.
Symptoms of jugular vein thrombosis

Symptoms of thrombosis of the internal jugular vein depend on how pronounced the pathological process is.
If it develops acutely, then the manifestations will be as follows:
Increase in body temperature. Fever is an unfavorable prognostic sign, as it indicates the addition of an infection. In this case, the likelihood of developing fulminant sepsis increases.
Formation of painful swelling on the neck.
Head movements will respond with pain. The pain intensifies during the extension of the neck and during the rotation of the head in a healthy direction.
Subcutaneous veins increase in size, may respond with pain during palpation.
A person tends to take a sparing position for the head in order to reduce pain.
Swelling of the neck, which can extend to the chest, shoulder, shoulder blade. Often jugular vein thrombosis is combined with subclavian vein thrombosis.
Violation of the venous outflow from the cranial cavity is accompanied by the following symptoms: severe headache, tinnitus, blue nasolabial triangle, swelling of the veins and face, numbness of the extremities, discomfort in the eyes, temporary loss of consciousness.
With the spread of thrombosis to the veins located in the immediate vicinity (subclavian, brachial, axillary), there is an increase in the intensity of symptoms, increased edema. This entails the risk of developing gangrene.
Sometimes acute manifestations of the disease are able to resolve on their own. In this case, the reverse development of the clinical picture is observed. However, a complete regression does not occur in most patients, and the disease passes into a chronic stage. At the same time, the reporting subsides completely, or becomes much less, the pain decreases. With rotation and tilting of the head, neurological symptoms will intensify. A person will begin to notice discomfort that was previously absent. These manifestations are due to stagnant processes, tissue hypoxia, the presence of perivascular edema, and an increase in the level of CO2 in the venous blood. Another sign that may suggest chronic jugular vein thrombosis is the presence of a firm, slightly painful mass in the neck.
In the chronic course of thrombosis, the symptoms of venous outflow from the cranial cavity do not disappear completely, but become less pronounced. The patient will periodically experience headaches, suffer from bouts of dizziness. Puffiness of the face often increases in the morning, and in the evening it can disappear.
Diagnostics

Diagnosis of thrombosis of the internal jugular vein most often does not cause difficulties for the doctor. It is based on the listed symptoms, but must be supplemented by instrumental methods. Preference should be given to computed tomography or MRI, as the most informative diagnostic methods. Although most often the patient is performed ultrasound (duplex scanning, dopplerography). In principle, the jugular vein is well accessible for ultrasound, so most often, the diagnosis is correct. In this case, it is imperative to distinguish between thrombosis and abscess, necrotic tumor and inflamed lymph nodes.
To assess the prevalence of thrombosis and to clarify the location of the thrombus, you can use phlebography using a contrast agent. However, phlebography should only be used in patients who will receive thrombolytic therapy. After the procedure, a fibrinolytic agent is immediately injected into the vein.
Treatment of jugular vein thrombosis
Since with jugular vein thrombosis there is always a threat of pulmonary embolism, the patient must be hospitalized on an emergency basis.
Treatment is most often conservative. If there is no therapy, then after 2-3 weeks from the beginning of the formation of a blood clot, it begins to dissolve. However, this does not mean that the patient can wait for the pathological process to resolve itself, since all this time there is a threat to his life.
The main objectives of the treatment of jugular vein thrombosis:
Stop the process of further formation of a blood clot.
Fix the thrombus on the vein wall.
Eliminate spasm of the vessel.
Eliminate the inflammatory process.
During treatment, the patient must adhere to bed rest. He is administered antibacterial drugs with a wide spectrum of action. This is necessary in order to prevent the development of the inflammatory process, or get rid of it.
The basis of the therapeutic effect in jugular vein thrombosis is anticoagulant therapy. For this, the patient is administered blood-thinning drugs for 3-10 days. After 10 days from the start of treatment, the patient is transferred to indirect anticoagulants.
Immediately after the patient’s admission to the hospital, he is prescribed venotonics. They have a beneficial effect on metabolic processes in the venous wall and surrounding tissues. They also relieve inflammation and reduce the intensity of pain.
Operative therapy
Surgical intervention in the form of resection or ligation of the vein is rarely necessary. The operation is prescribed in the case when there is a risk of developing gangrene, with severe hemodynamic disorders. During phlebography, it is possible to use balloon angioplasty of a vein in parallel, or to perform its endoprosthetics.
Forecast
If a person has not been treated, and thrombosis has acquired a chronic course, then it will be more effective to eliminate the thrombus surgically. Therapy with medications in this case gives a minimal effect. Therefore, the vast majority of patients are prescribed reconstructive vascular surgery. Their goal will be to create bypass routes for venous outflow and unload the jugular vein.
As a rule, the prognosis for jugular vein thrombosis is favorable. However, a full recovery, even with timely therapy, is not always achieved.









