Contents
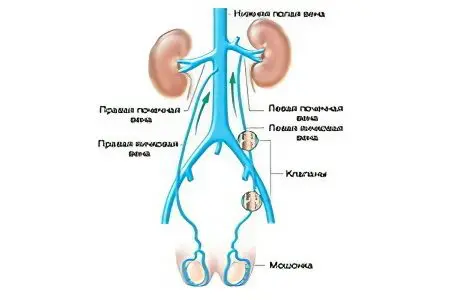
The inferior vena cava is one of the largest vessels of the human circulatory system. It delivers blood to the right atrium from the organs of the abdominal cavity, small pelvis, from the lower extremities. Despite the fact that the inferior vena cava has an impressive diameter, blood clots can form in its lumen, just like in any other vessel. Since the cessation of blood circulation in the main vessel carries the most severe consequences, thrombosis of the inferior vena cava often ends in death. It is this pathology that in 90% of cases causes pulmonary embolism.
Causes of
Most often, blood clots form in the vessels of the lower extremities and small pelvis. The reason for this is that a person is predominantly in an upright position. When walking, the load on the legs increases, because the blood has to develop an increased speed for circulating in the vertical direction.
Reasons for the formation of blood clots:
Mechanical, allergic, infectious damage to the vascular wall. Violation of the smoothness of the inner wall of the vein creates the preconditions for the accumulation of blood cells in this place. With an increased concentration of blood cells, a thrombus is formed.
Increased blood clotting. Heredity, bad habits, environmental influences, the consequences of past diseases can cause changes in the clotting index.
Slow circulation. Hypodynamia, diseases of the heart and blood vessels negatively affect the speed of blood flow. At the same time, blood cannot pass through the venous valves at an optimal speed, it moves in the opposite direction, stagnates.
The combination of these causes is called the Virchow triad. It is considered an important indicator for the diagnosis of thrombosis. Since the speed of blood flow and the diameter of the inferior vena cava do not create prerequisites for thrombosis, this pathology develops as a result of the migration of a thrombus into it from the lower extremities, vessels of the abdominal cavity, and small pelvis.
Risk Factors
Factors predisposing to thrombosis:
Injuries of the limbs and abdominal cavity;
The presence of a malignant tumor;
Surgical intervention in the abdominal cavity, on the organs of the genitourinary system, on the lower extremities;
Taking hormonal contraceptives;
Infections transmitted through the circulatory system;
Varicose veins in history;
Complicated course of pregnancy and childbirth;
Allergy, autoimmune pathology;
Hormonal imbalance;
Diseases of the endocrine system;
Prolonged bed rest.
At risk are the elderly, patients with chronic diseases, as well as those who are overweight, prone to bad habits, a profession that involves a static posture.
Clinical picture of thrombosis of the inferior vena cava

The classic signs of a thrombus being directly in a vein are protruding veins on the surface of the abdomen and chest, swelling of both lower extremities, genitals and abdomen, and pain in the lower body. Such a picture is rare, because a thrombus rarely forms in the vein itself, it migrates into the vessel from its other branches.
Segments of the inferior vena cava affected by thrombosis:
infrarenal,
Renal and suprarenal
Hepatic.
The clinical picture of the lesion occurs in the case of complete occlusion of the vessel. If a floating thrombus enters the inferior vena cava and its segments, or a parietal blood clot forms, the manifestations of the pathology are slightly expressed.
Thrombus in the infernal segment – symptoms:
Severe back pain;
Edema of the extremities, cyanosis;
Prominent veins in the lower abdomen.
Symptoms of thrombosis of the veins of the renal region are similar to the symptoms of a tumor of the kidney. In this case, the blood flow is rarely completely disturbed, since in this area it is quite powerful.
Thrombus in the renal and suprarenal segment – symptoms when blocking the renal venous outflow:
Severe lower back pain;
Microhematuria;
Macrohematuria;
A sharp decrease in the concentration and volume of urine;
Increase in the blood content of urea and creatinine;
Replacing oliguria with anuria (complete cessation of urine output);
Nausea and vomiting;
Symptoms of intoxication.
When the blood flow is restored, the symptoms change for the better, the patient’s well-being improves.
If the hepatic segment of the inferior vena cava is affected, the symptom complex appears immediately. Up to 1,5 liters of blood accumulates in the liver, its fibrous membrane is stretched.
Thrombus in the hepatic segment – symptoms:
Bursting pains in the right hypochondrium, extending under the scapula;
On palpation, the smoothness of the liver is felt, the roundness of its edge;
Ascites;
Change in skin color, jaundice;
Enlargement of the spleen;
Expansion of superficial veins at the top of the abdomen, in the lower part of the chest;
Cyanosis of the anterior wall of the peritoneum.
Thrombosis of the inferior vena cava should be distinguished from circulatory failure, heart failure, lymphostasis of the extremities, anaerobic phlegmon, traumatic edema, soft tissue hematoma, arthrosis and arthritis, dropsy of pregnant women, crushed tissue syndrome.
Diagnostics

Since in a certain part of patients the pathology is asymptomatic, or its manifestations are masked by the symptoms of another serious disease, instrumental diagnostics comes first in the diagnosis.
Purpose of the survey:
Confirmation of the presence or absence of thrombosis;
Determination of its location;
Identification of the risk of pulmonary thromboembolism;
Identification of an asymptomatic thrombus in other vessels;
Determine the cause of the thrombus.
When choosing a diagnostic method, the doctor focuses on its safety, information content, and economic feasibility. Priority is given to non-invasive methods of diagnosis.
Emergency diagnostic methods:
Rapid test for determining the level of D-dimer in blood plasma – an excessive amount of fibrin breakdown products is evaluated as a marker of intravascular thrombosis;
Radionuclide study with labeled fibrinogen – determines the hidden source of thrombosis, is not used in pregnant and lactating women, unable to assess the likelihood of embolism;
Duplex ultrasonic angioscanning – allows you to observe the processes of thrombus formation in dynamics, adjust the treatment;
X-ray contrast retrograde or ocavography – determines the proximal border of the thrombus and its nature, is limitedly used in pregnant women, is prohibited in the 1st trimester.
During angiography, it is possible to carry out therapeutic manipulations – implant a cava filter, perform catheter thrombectomy.
Treatment of thrombosis of the inferior vena cava
In the treatment of thrombosis of the inferior vena cava and its segment, conservative and surgical methods are used. The doctor’s goal is to prevent pulmonary embolism, prevent edema, restore vein patency, remove the thrombus, and prevent recurrent thrombosis. Treatment of any form of thrombosis begins in a hospital, to eliminate the risk of pulmonary embolism.
Conservative therapy
Until the risk of PE is ruled out, the patient must remain in bed. Prolonged stay in bed for more than 7-10 days lowers the rate of blood circulation, therefore, after removing the edema, eliminating the risk of floating thrombosis, dosed walking is recommended, performing therapeutic exercises to improve venous outflow.
An effective measure for the prevention of varicose veins is the use of elastic compression. The patient applies the imposition of a compression bandage.
The patient is prescribed anticoagulants, hemorheologically active agents. If required, then NSAIDs, with a high risk of sepsis – antibiotics, ointments for local treatment.
Therapy with drugs – groups of drugs:
It is forbidden to use warming ointments and compresses that increase blood flow.
Operative therapy

The goal of surgical intervention for thrombosis of the inferior vena cava is to restore the lumen of the vessel, preventing pulmonary embolism. Thrombectomy is used to solve these problems.
In cases where there are contraindications to radical surgery, palliative interventions are used to prevent PE:
Endovascular operations;
Ligation of deep veins;
Plication of the inferior vena cava;
Implantation of cava filters.
These methods can be combined or used in isolation, independently of each other. In a serious condition of the patient, aggravated by somatic diseases and age-related changes in the body, preference is given to minimally invasive interventions.
Thrombosis of the inferior vena cava is a complex pathology with an unpredictable prognosis. At the first signs of the disease, you should seek qualified medical help.









