Contents
Thrombocytopenia is a general name for diseases that are characterized by a decrease in the number of platelets in the blood. Normally, this value is 180-400 * 109/ l. If the level of platelets is significantly reduced, then the person will experience nosebleeds, women suffer from prolonged menstruation, which is accompanied by copious bleeding. Also, bleeding gums, subcutaneous and internal hemorrhages indicate thrombocytopenia.
What are platelets responsible for in the body?
The site of platelet production is the bone marrow. They are produced from large megakaryocytes. Platelets are plate-like in shape, oval or rounded. The diameter of blood cells is 2-4 microns. Platelets can change the shape of a circle to a spherical shape, forming outgrowths on their outer membrane, which is possible due to the presence of receptors on their surface, which are based on glycoprotein complexes. With these outgrowths, they are connected to each other and to the vascular walls in the place where they are damaged. Fibrin threads allow platelets to attach to existing defects, after which these blood cells begin to secrete an enzyme called thrombostenin. Under its influence, the threads twist and become denser.
Platelets also produce enzymes responsible for normal blood clotting, as well as platelet fibrinogen, platelet growth factor, peroxidases, serotonin, immune complexes and other substances that play an important role in the normal functioning of the body.
So, platelets are necessary for a person to ensure his life, as they take part in many important processes, including:
The formation of a blood clot, which is necessary to stop bleeding at the site of damage to small vessels.
Maintenance of vascular spasm.
Nutrition of the vascular wall.
Production of immune complexes.
Dissolution of blood clots.
Platelet levels over 24 hours can fluctuate within no more than 10% of the normal level. If a woman is menstruating, then these fluctuations range from 20 to 50%. Therefore, when making a diagnosis of thrombocytopenia, it is necessary that the platelet level be less than 100 * 10 9 / L.
A new platelet, on average, exists for no more than 10 days. After that, it gets smaller. If platelets are less than 7.0 fl, then the person has either recently had their spleen removed or is suffering from Wiskott-Aldrich syndrome. This disease is accompanied not only by thrombocytopenia, but also by immunodeficiency and skin eczema. Therefore, during laboratory diagnostics, it is necessary to take into account the average size of platelets. This indicator is referred to in the analysis results as MPV. Its normal values are 7,4-10,4 fl.
Pathogenesis of thrombocytopenia
The level of falling platelets in the blood occurs for the following reasons:
A drop in the level of megakaryocytes, or their complete disappearance. Megakaryocytes can stop being synthesized by the body when a person develops pathologies of the blood, thyroid gland, and liver. Abuse of alcohol, intake of toxic substances, past viral infections, intake of antibacterial drugs, radiation exposure of the body, lack of vitamin B12 and folic acid negatively affect their numbers. Low levels of megakaryocytes are seen in people who are receiving HIV therapy or who develop HIV-associated infections.
Increased destruction of platelets. The reasons why platelets are destroyed at a high rate are very diverse, among them: Werlhof’s disease, DIC, a blood transfusion, undergoing therapy with antihistamines, sulfonamides, etc.
Failure in the distribution of platelets. If a person does not have any pathologies in the body, then about 45% of all platelets are in the spleen. If somewhere there is an increased need for these blood elements, then the supply is taken from this depot. Provided that a person suffers from tuberculosis, hepatitis, malaria or blood disease, the level of platelets in the spleen can rise up to 90%. This will lead to the fact that they will begin to become smaller in size and break down faster.
So, thrombocytopenia is often the result of exposure to drugs, but it can be both a symptom of hereditary pathologies and a sign of many diseases acquired during life.
Types of thrombocytopenia
Thrombocytopenia can be a congenital or acquired pathology. Congenital diseases include Wiskott syndrome, Fanconi syndrome, giant platelet syndrome, etc.
However, most often thrombocytopenia is a consequence of acquired diseases, or rather reduced immunity against their background.
In this regard, the following types of thrombocytopenia are distinguished:
Isoimmune, which develops due to the incompatibility of the blood groups of the mother and fetus.
Transimmune, when the autoantibodies of a mother suffering from autoimmune thrombocytopenia are transferred to the fetus.
Heteroimmune, which develops under the condition that platelets are damaged by a pathogenic agent, after which the body began to produce antibodies against them.
Autoimmune, when the body recognizes its own platelets as foreign substances and begins to destroy them. This condition may be accompanied by cancer, autoimmune processes, HIV, herpes infection, rubella, and may develop while taking medications.
Thrombocytopenic purpura

Purpura associated with low platelets in the blood can be due to hepatitis, systemic lupus erythematosus, lymphoma, and other diseases. If the cause of purpura remains unclear, then we can talk about the idiopathic nature of the disease.
Werlhof’s disease is a chronic form of thrombocytopenic purpura. In 5% of cases, the pathology ends in death, the cause of which is a hemorrhagic stroke, or open internal bleeding. The vast majority of patients with this diagnosis are young women. In childhood, idiopathic thrombocytopenia develops acutely, but in 75% of cases it ends safely, that is, with a full recovery.
Symptoms of thrombocytopenia

The symptoms of thrombocytopenia are as follows:
Multiple subcutaneous hemorrhages are found on the human body, which can be presented both in the form of small dots and in the form of large hematomas. Moreover, they are formed even with a slight impact or other physical impact.
The rash may be blue, brown, green or yellowish in color. This indicates that they did not appear at the same time, but at different times (some pass, others are quite fresh).
Hemorrhages are located on the arms and legs, on the abdomen, on the face, in the oral cavity, on the chest.
A person notices increased bleeding of the gums, he is worried about nosebleeds, which happen quite often.
In women, prolonged menstruation is observed, and bleeding from the vagina also occurs in between cycles.
Against the background of thrombocytopenia, bleeding after surgery is a danger to human life. And it is not necessary that the intervention will be global. We are talking even about the removal of teeth, or overgrown tissue of the tonsils.
Hemorrhages often occur also in the eyeball.
Bleeding of internal organs, including the brain, may develop.
Sometimes a symptom of thrombocytopenia is an increase in the size of the spleen.
Symptoms of thrombocytopenia are explained not only by the fact that the blood loses its ability to clot, but also by the fact that the permeability of the vessel wall increases. The blood cannot coagulate due to the fact that the production of an enzyme is disrupted, which is responsible for gluing platelets to the vascular wall, as well as for their normal size. The vessels lose their normal permeability due to the fact that the processes of their nutrition, for which platelets are responsible, are disturbed. The influence is exerted by a low level of serotonin, which is also produced by platelets and regulates the normal contractions of the vascular wall.
Thrombocytopenia in childhood and during pregnancy

Women bearing a fetus rarely experience an acute form of the disease that has a severe course. However, thrombocytopenia increases the risk of miscarriage in the first six months of pregnancy. In its second half, the threat of an early onset of labor increases, as well as the development of severe bleeding during childbirth.
Sometimes during pregnancy, a woman recovers from thrombocytopenia. However, in the chronic form of the disease with its frequent exacerbations, doctors recommend abandoning procreation.
In children, pathology occurs infrequently, from 100 to 000 babies are sick per 3 people. The main symptom of the disease in childhood are small subcutaneous hemorrhages.
How to detect thrombocytopenia?
The doctor may suspect a pathology based on the examination of the patient and the collection of anamnesis.
Blood donation is required to confirm the diagnosis:
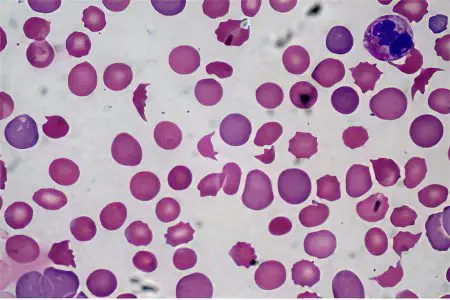
The level of platelets is low, or they are absent in the blood at all.
Platelets are reduced in size.
Blood taken from a vein will clot after 6 hours. Sometimes it can remain loose for several days.
Antibodies to platelets are found in the blood.
The granularity of platelets is reduced.
Platelets have different colors and different shapes.
The patient is diagnosed with anemia and leukopenia.
When taking a bone marrow puncture, multiple megakaryocytes without granules, with vacuoles, were found in it. Cells grow unevenly. When the disease recurs, the number of megakaryocytes decreases.
Treatment of thrombocytopenia
If the patient develops massive bleeding, then he needs a transfusion of plasma and blood with an increased content of platelets. However, it is necessary to ensure that antiplatelet antibodies do not begin to form in the patient’s own blood. If the transfusion is not stopped in time, the bleeding will only increase.
To stop blood loss, the patient is given the necessary drugs to stop him and improve his general condition. If bleeding increases, then a transfusion of plasma and red blood cells is indicated.
If thrombocytopenia is provoked by autoimmune processes, then the patient is shown systemic administration of corticosteroids. As bleeding decreases, the dosage of hormonal drugs is reduced. Treatment with glucocorticosteroids can last 1-3 months.
Operative therapy
If it is not possible to cope with the pathology with the help of medical correction, and the disease recurs, then the removal of the spleen is required. The efficiency of the operation is equal to 80%. Platelets cease to undergo massive decay, which leads to recovery.
If none of the methods allows you to achieve a result, then the patient is prescribed immunosuppressants. However, these drugs adversely affect the immune system and the function of hematopoiesis.
The prognosis for recovery from thrombocytopenic purpura is most often favorable.









