Contents
Tuberculosis is one of the oldest scourges known to mankind. In Rus’, it was called “dry disease”, and later – “consumption”. In ancient Greece, the disease became famous under the name phtisis, which means “exhaustion.” From this word comes the modern name of the medical branch that studies the problem of tuberculosis – phthisiology. And a doctor who specializes in the treatment of tuberculosis patients is known to everyone as a phthisiatrician.
Despite the outstanding successes of modern science in the development of diagnostic tools, the prevention of epidemics and the treatment of complex infections, tuberculosis has not yet been defeated. On the contrary, the problem of the incidence of this disease is becoming more acute in some countries of the world. The spread of tuberculosis is directly related to the processes of globalization and migration, behind which the medicine of developing countries simply does not keep up.
Russia is in 22nd place in the world in terms of incidence and mortality from tuberculosis, and this is a very sad figure. Although over the past ten years the Ministry of Health has managed to achieve impressive results in the fight against the spread of the disease, it is too early to talk about success. And in order to protect yourself and your loved ones, it is better to arm yourself with relevant and reliable information. From this article you will learn absolutely everything about tuberculosis: what it is, what causes it, how it is transmitted, what methods it is diagnosed and treated with.
What is tuberculosis?
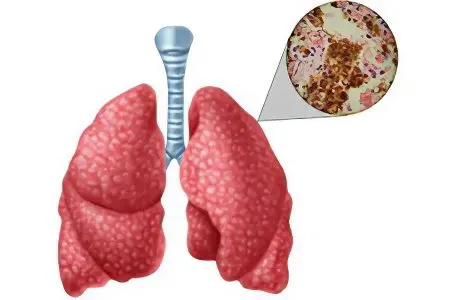
The term “tuberculosis” comes from the Latin word tuberculum (“tubercle”), because it looks like foci of inflammation – tuberculous granulomas. This disease is caused by mycobacteria of the species Mycobacterium tuberculosis complex, that is, directly by mycobacteria tuberculosis (MBT) and its closest relatives. The main lesion is the respiratory tract (lung bronchi), but sometimes mycobacteria cause inflammation in the lymphatic, nervous and genitourinary systems, the musculoskeletal system, on the skin, or even affect the entire body (miliary form).
The invincibility of tuberculosis is due to several reasons:
The causative agent of the disease often does not manifest itself for years, and even when the inflammatory process begins, the person is in no hurry to see a doctor. The early symptoms of tuberculosis are easily confused with the common cold or overwork. As a result, time is lost, and the patient has to undergo a long, complex treatment;
Tuberculous mycobacteria are extremely resistant to the aggressive influence of the external environment, remain viable for a very long time and infect more and more people in places where no one expects to meet them, and where it is impossible to get rid of them by any sanitary and hygienic methods;
The causative agent of tuberculosis mutates rapidly, becoming resistant to antibiotics. Moreover, the mutation can occur already in the body of a sick person in the course of the disease. This greatly complicates and prolongs the treatment, and in the absence of success, it can cost a person life. For example, in 2008 alone, according to the WHO, 9 million people fell ill with tuberculosis in the world, and a third of them died.
The first mention of tuberculosis
Modern archaeologists have more than once had to extract human remains from ancient burials with signs of tuberculous bone lesions, moreover, some skeletons belong to people who lived on Earth 3000 years before our era. Therefore, we can say with confidence that tuberculosis is the same age as humanity and its unchanging sad companion.
Although the contagious nature of this disease was not proven until the end of the nineteenth century, people have long guessed that tuberculosis is contagious. For example, the Babylonian “Laws of Hammurabi” allowed a husband to unilaterally terminate a marriage with his wife if she had signs of tuberculosis. And the ancient Indian “Laws of Manu” completely forbade men to marry such women. The ruler of Venice issued a law requiring citizens to report all tuberculosis patients “where they should be.”
The first scientific descriptions of tuberculosis were written by Hippocrates. Although the famous Greek healer was distinguished by a deep mind and incredible powers of observation, he was mistaken about tuberculosis. Hippocrates noticed that members of the same family usually suffer from this disease, and made a false conclusion about the hereditary nature of tuberculosis.
Another well-known healer, Avicenna, who lived later, pointed out in his notes a direct connection between tuberculosis and pleurisy, as well as the fact that an unfavorable environment and low social status contribute to the onset of the disease: poor people who are malnourished, live in dirt and hard labor. Avicenna was sure that the disease was contagious, but did not know how to cure it.
In ancient Russian chronicles there are references to tuberculosis of the lymphatic system. The Kyiv prince Svyatoslav Yaroslavich suffered from this disease in 1076. The treatment in those days was surgical: the foci of inflammation were cut out, and then the places were cauterized. Of course, this technique did not help the healers heal the prince.
History of tuberculosis research
The disease acquired the character of an epidemic in the 20th-XNUMXth centuries, when the active construction of cities, the development of industry, trade and transport began. People traveled, went to work, and along the way spread the deadly bacteria. In the middle of the seventeenth century, in the British Peninsula alone, approximately XNUMX% of deaths were due to tuberculosis. The situation in the rest of Old Europe was no better.
At the same time, the first medical research began, aimed at establishing the nature of tuberculosis and finding methods of treatment. Dr. Francis Silvius, who lived in the 1761th century, first discovered tuberculous granulomas at the autopsy of a patient who died of consumption, but mistakenly took them for enlarged lymph nodes. However, then M. Bailey (1821-XNUMX) got to the bottom of the truth and realized that the tubercles are a form of manifestation of the disease and the basis for the further spread of inflammation.
A follower of Dr. Bailly, the French scientist Rene Laennec (1781-1826), first introduced the term “tuberculosis”, and also described several types of this disease. He also suggested the use of lung auscultation, which was a breakthrough in diagnosis. Russian doctor G.I. Sokolsky (1807-1886) was familiar with the works of Laennec and relied on them in his scientific work. The result was the book “The Doctrine of Chest Diseases”, which was published in 1838. In it, Sokolsky for the first time describes the cavernous, infiltrative and disseminated forms of tuberculosis, however, under different terms.
A great contribution to unraveling the nature of tuberculosis was made by the French ship’s doctor Jean-Antoine Villemain. In 1865, while on a voyage, he discovered that one of the sailors was ill with tuberculosis, and witnessed how the same symptoms gradually appeared in other crew members. To confirm the contagiousness of the disease, the doctor collected infected sputum and soaked it in the bedding on which the guinea pigs lived. Animals contracted tuberculosis and died.
In 1879, the German pathologist Julius Konheim confirmed Wilmen’s hypothesis with the help of another animal experiment: he introduced fragments of a human lung infected with tuberculosis into the eye chamber of rabbits, after which he observed the development of tuberculous granulomas there.
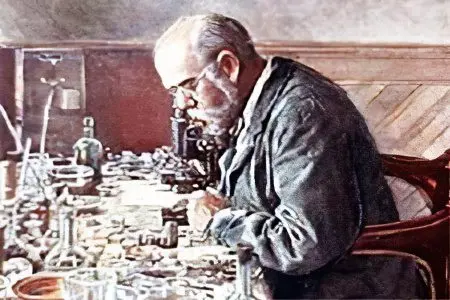
However, it was only in 1882 that it became known for certain how the deadly disease spread and affected millions of people. German doctor Robert Koch devoted 17 years of his life to studying this issue, and was finally able to detect and examine a dangerous mycobacterium under a microscope after he stained an infected sample with methylene blue and vesuvin. Then the doctor was able to isolate a pure bacterial culture and infect experimental animals with it. In honor of the discoverer, mycobacterium tuberculosis was named “Koch’s wand”. A solution with a bacterial culture, called “tuberculin”, is still used for diagnostic purposes.
Forms and types of tuberculosis
In more than 90% of cases, tuberculosis is localized from the lungs, but there are also bone, genitourinary, skin, brain, intestinal, miliary varieties of the disease, so it is customary to distinguish two forms of tuberculosis:
Pulmonary;
Extrapulmonary.
Based on whether a person fell ill for the first time, or the disease after remission again passed into the active stage, two types of tuberculosis are distinguished:
Primary;
Secondary.
primary tuberculosis
This is an acute form of the disease that occurs immediately after the pathogen enters the bloodstream. Primary tuberculosis often affects children under the age of five, because their not fully formed immune system cannot cope with the attack of tuberculosis mycobacteria. Although the disease is severe and has pronounced symptoms, for others at this stage, patients are not contagious.
In the lungs, the primary lesion is formed – a small granuloma. Further events can develop either according to a favorable or sad scenario. In the first case, the tuberculous granuloma heals on its own. Sometimes a person does not even realize the seriousness of the problem, attributing his malaise to fatigue and a cold. Then, during an x-ray examination, a “surprise” will be found in his lungs – a healed granuloma.
In the second case, the granuloma increases, and a free cavity appears inside it, filled with blood – a cavity. From the cavity, tuberculous mycobacteria spread throughout the body with the bloodstream, producing new foci of inflammation. The primary cavity can still close and grow together without treatment, but if new granulomas appear, and new cavities follow them, then without medical help a person will die.
Secondary tuberculosis
They talk about secondary tuberculosis when a person who has been ill has become infected with another type of tuberculosis mycobacterium and falls ill again, or when remission turned into an exacerbation. This situation is more typical for adult patients. In the lungs, new foci of inflammation are formed, sometimes so close to each other that the cavities merge, and extensive cavities with exudate appear. About 30% of patients with severe secondary tuberculosis, despite the efforts of doctors, die within 2-3 months. And only in one patient out of a hundred, secondary tuberculosis subsides as spontaneously as it arose.
A person suffering from secondary pulmonary tuberculosis is very contagious to others. When coughing with phlegm, bacteria are constantly released into the air. Such a patient is hospitalized and undergoes long-term treatment with combined antibiotics, which can last up to six months. Then for another two years the person is registered with a phthisiatrician. And only then, if the X-ray examination confirms the absence of new foci of the disease, the diagnosis of tuberculosis is finally removed.
World epidemiological reference
According to the world epidemiological reference:
Tuberculosis is now second only to AIDS in terms of the number of lives it claims every year.
In 2013, 9 million people fell ill with tuberculosis on planet Earth, of which one and a half million died. 550 thousand patients are children, 80 thousand of them died.
Nearly 95% of TB deaths occur in lagging and developing countries in Africa and Asia.
Tuberculosis is one of the three most common causes of death in women of reproductive age (16-45 years).
A quarter of all deaths of HIV-infected patients are caused by tuberculosis.
According to WHO, about 480 people who fell ill with tuberculosis in 2013 were affected by MDR-TB, a multidrug-resistant form of the disease that is practically untreatable.
From the early 45s to the present, the global death rate from tuberculosis has fallen by XNUMX%.
Thanks to modern diagnostic methods, from 2000 to 2013, approximately 37 million lives were saved worldwide.
Mortality from tuberculosis in Russia
As of 2013, out of a hundred thousand cases of tuberculosis in Russia, 11,3 ended in death. This is a big improvement compared to the figures of 2000: since then, the incidence has decreased by 30%, and the mortality rate by about 33%.
The state budget of Russia for 2015 includes 4 billion rubles for the prevention and control of tuberculosis.









