Contents
The different types of drug interactions

Drug interactions: a major health problem
If there is one market that the crisis has not altered, it is the health sector. An OECD report recently showed that drug overuse remains a major societal problem. If Canadians are the second largest consumers of drugs behind the Americans, the French are not left out. They remain the undisputed champions of the use of “happiness pills”, the antidepressants. This habit leads to hundreds of consultations every day related to the inadequacy of a treatment, its overdose or its association with another drug. There would be, according to the French Ministry of Health, 128 hospitalizations and 000 annual deaths due to bad drug interactions, ie twice the number of people killed on the roads!
Seniors on the front line
Advances in medicine have made it possible to push life expectancy to unexpected limits. But this new perspective comes at a price: People over 65 often have to juggle drugs they don’t know anything about. A legitimate polypharmacy but which considerably increases the risk of the appearance of side effects linked to drug interactions. They are defined as “modification of the effect of a drug following the concomitant administration of another drug”. This phenomenon, often underestimated, is responsible for 10% of hospitalizations in people over 65 and almost 20% in over 80 years. It can nevertheless occur in all categories of the population and lead to the worst-case scenario.
The journey of a drug through the body
To understand the mechanisms, it is first necessary to recall the mode of operation of a drug. Whether in capsule, cream or spray state, it always has a substance active (or active principle), that is to say a component which has a therapeutic effect. To be effective, this substance must reach the systemic circulation (the blood) and therefore cross the biological membranes of the site of absorption. This can be the lining of the digestive tract when administering oral formulations (tablets, oral solutions, etc.) or the skin when administering percutaneous formulations (ointments, patches, etc.). Once in the blood stream, these substances will seek to reach the site of action, but part of them will bind to transport proteins: this is the stored form. Only the free form will be able to pass biological membranes and subsequently exert a therapeutic effect. It is its adhesion to a receptor which will then cause the action: inhibition of the synthesis of bacteria, reduction of pain, stimulation of the immune system …
The body’s response
At the same time, the body will try to get rid of this drug, which it sees as a foreign compound. The enzymatic system, in particular in the liver, will focus on transforming it into a product that is easily eliminated through the urine: it is the metabolization. The active substance is then eliminated by the body, either in unchanged form or in the form of processed products (metabolites) via the kidney, the main organ of excretion. Depending on the nature of the drug, the body will have more or less trouble breaking it down. Some will be eliminated quickly while others will persist for a long time in the body. This depends on the body’s ability to degrade the molecule concerned (= clearance) but also on the dose administered: the stronger it is, the more its lifetime in the body will be high.
All of these parameters play a role in the effectiveness of a drug. When administering treatment, care must be taken to ensure that the prescribed dose is sufficient to be effective. If the body’s ability to break down the drug is high (therefore clearance), there is a good chance that the drug is ineffective. The dose must then be increased. But, conversely, care must be taken that the latter is not too strong to be toxic! Sometimes this therapeutic margin is very weak and interactions with other drugs will significantly affect it. It is therefore very important to have all this in mind when combining several treatments.
There are actually two main types of drug interactions:
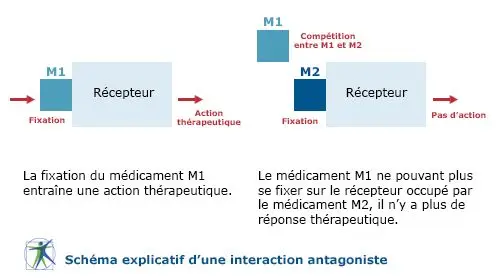
— l’interaction pharmacodynamic : the effect of a drug will reduce or amplify the action of another drug, by intervening on its site of action (= the receptors).
— l’interaction pharmacokinetics : the effect of a drug will reduce or increase the concentration of a second drug in the body.









