Contents
- What is pulmonary tuberculosis?
- Early signs of pulmonary tuberculosis
- Other symptoms of pulmonary tuberculosis
- Is pulmonary tuberculosis contagious or not?
- Stages of pulmonary tuberculosis
- Forms of pulmonary tuberculosis
- Complications and consequences of pulmonary tuberculosis
- Diagnosis of pulmonary tuberculosis
- How is the treatment?
- Prevention of pulmonary tuberculosis
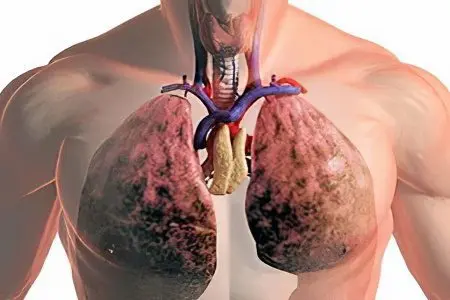
What is pulmonary tuberculosis?
Pulmonary tuberculosis is a disease of an infectious nature, characterized by the appearance in the lungs of specific inflammatory changes. This disease is caused by Mycobacterium tuberculosis, also called tuberculosis bacillus. It is transmitted through the air, when coughing, talking, sneezing.
According to WHO, there are up to 2 billion infected people in the world. Medical sources indicate that 100 out of 18 people in Russia die from the disease every year, which would seem to be a small number. However, based on the total number of people in the country, it turns out that tuberculosis will kill 25 people in just one calendar year. Although over the past 000 years, the mortality of this disease has decreased by almost 13%.
Incubation period for pulmonary tuberculosis
From the moment Koch’s wand enters the body, and until a person develops the first symptoms of the disease, a certain period passes, called the incubation period. For each person, it makes up different time periods, but lasts at least 3 months and no more than a year. Although the moment when the bacterium leaves the incubation stage can often be mistaken for the symptoms of a common ARVI.
During the incubation period, the following happens: all mycobacteria that enter the respiratory tract are attacked by the immune system. If he copes well with his own functions, then they die. In this case, the disease does not develop. If for some reason the immune system fails, the mycobacterium continues its journey through the respiratory tract, is absorbed into the bloodstream and enters the lungs, starting to cause inflammation in them. At the end of the incubation period, the initial symptoms of the disease appear.
It is important that during this stage the person is not contagious to the people around him. Moreover, the Mantoux test gives negative results, which significantly complicates the diagnosis of the disease in the early stages.
Early signs of pulmonary tuberculosis
It is necessary to be attentive to your own health and pay attention to the slightest changes in your own body so as not to miss the early signs of pulmonary tuberculosis. This is important because the disease often does not manifest itself in any way, and can only be detected after undergoing a fluorography.
The following symptoms should alert a person:
Frequent and unmotivated dizziness.
Apathy and lethargy.
Sleep disturbances and excessive sweating during night rest.
Pale skin.
Blush on cheeks.
Unexplained weight loss.
Lack of appetite, not associated with gastrointestinal disease.
Subfebrile body temperature, not exceeding 37 ° C.
If one or more signs are found, it makes sense to consult a doctor and undergo not only fluorography, but also an x-ray of the lungs.
Other symptoms of pulmonary tuberculosis

At a late stage in the development of the disease, tuberculosis manifests itself more pronouncedly. It is characterized by the following features:
Persistent cough with or without sputum.
Shortness of breath, in which a person feels an acute shortage of air even after a slight physical exertion.
Wheezing, which the doctor may pay attention to when listening. Their intensity and characteristics do not lend themselves to a specific description, since they can be varied: dry and wet.
Increased body temperature.
Shine in the eyes, pallor of the skin.
Sometimes there are symptoms of vegetative-vascular dystonia.
Sudden weight loss, up to 15 kg or more.
The appearance of blood in the sputum.
The occurrence of pain in the sternum, both during a deep breath, and at rest. This symptom appears if the process has moved to the pleura.
If the last two signs were found, then this means that the person is sick with a complex form of tuberculosis and prompt hospitalization is indicated for him. Often, it happens that the disease, originating in the lungs, passes through the blood to the intestines, bones and other organs.
Temperature in pulmonary tuberculosis
Hyperthermia is one of the leading signs of infection of the body with Mycobacterium tuberculosis. It is this reaction of the body that often precedes all the main manifestations of the disease and is a clinical sign of lung damage. This disease is characterized by both constantly high thermometer readings (in acute form of tuberculosis and caseous pneumonia) and subfebrile values (in focal, infiltrative and disseminated forms).
Rarely, but the following type of fever occurs: the temperature rises to low values in the morning and declines in the evening. With active, progressive forms of the disease, the temperature can reach 41 ° C.
Cough in pulmonary tuberculosis
Cough with pulmonary tuberculosis has the following features:
The cough is wet. The person feels that there is a lump in the chest, and constantly tries to cough it up. This is due to the fact that mucus accumulates in the bronchi, as a result of the ongoing inflammatory process. It interferes with normal air circulation, disrupts gas exchange in the alveoli. Therefore, a person has a protective reflex – a constant cough, which is designed to clear the lumen for the normal passage of air. But due to the fact that the mucus is constantly arriving, the cough occurs again and again.
The nature of the attacks is most often protracted. This is due to the fact that when trying to cough up mucus, the patient strains the pleura and diaphragm, which causes pressure on the lungs and a violation of their ventilation. This leads to the spread of inflammation and causes difficulty in breathing, and hence new coughing fits.
Cough with tuberculosis is most often with sputum. It is a mixture of pus and mucus. It contains a colossal number of pathogens, which explains the prevalence of tuberculosis. At the initial stages of the development of tuberculosis, the mucus is transparent and light, later it becomes rusty due to blood impurities. At the final stage, a person begins to cough up blood alone, with impurities of pus. The discharge has an unpleasant putrid odor.
Increased coughing most often occurs when a person is in a prone position. Therefore, seizures often overtake the patient during a night’s rest. This is due to the excessive production of mucus and its stagnation, when a person remains motionless for a long time. There may also be pain in the chest and a constant urge to cough. Rest on high pillows can alleviate the patient’s condition.
Is pulmonary tuberculosis contagious or not?
This disease is very dangerous and contagious, especially considering how many people suffer from tuberculosis. The method of transmission is airborne. Not a single person can insure against a meeting with a dangerous mycobacterium. In addition, not only people can become carriers of the disease, but also insects, for example, flies and cockroaches.
There is a belief that a person is contagious if he is a carrier of an open form of the disease. It really is. Tuberculosis is not transmitted in a closed form. But the whole danger lies in the fact that the transition of the disease from a closed form to an open one cannot always be noticed in time. Symptoms can easily be confused with a common cold, while the person is already a danger to others. And in a year, a person suffering from an open form infects at least 15 people. That is why the disease is so common on the planet.
Stages of pulmonary tuberculosis
There are three stages of pulmonary tuberculosis:
primary infection. Inflammation develops locally, in the area where the infection has entered. In this case, the bacteria enter the lymph nodes and the primary complex is formed. As a rule, a person feels well, sometimes primary signs of infection are observed.
stage of latent infection. If the immune system is weakened, then mycobacteria begin to multiply and spread throughout the body. Foci of tuberculosis are formed, localized in various organs.
Recurrent tuberculosis of the adult type. Formed foci of the disease begin to affect the organs. The lungs are most commonly affected. If the cavities formed inside them break into the bronchi, the person becomes contagious to others and we can talk about an open form of the disease.
Forms of pulmonary tuberculosis

The forms of the disease can be different. It is on what form tuberculosis has that the prognosis and method of treatment largely depend, as well as how dangerous the disease will be for others and for the carrier of the Koch wand itself.
Infiltrative pulmonary tuberculosis
This form of the disease is characterized by the fact that inflammatory changes are formed in the lungs, which are exudative in nature (that is, the processes occur directly in the area of inflammation). Caseous necrosis is formed in the center – the tissue becomes similar to a protein mass consisting of cottage cheese. The decay process is quite dynamic. Caseous pneumonia is also referred to this form of tuberculosis, but with it necrosis is more pronounced.
Sometimes the infiltrative form proceeds inapperceptively (that is, imperceptibly for the person himself) and is detected only when a person undergoes an x-ray examination. A clear symptom of this form of the disease is early hemoptysis, with a fairly satisfactory condition of the person. Often the disease develops under the cover of pneumonia, bronchitis, prolonged flu, etc.
Disseminated pulmonary tuberculosis
This form of the disease occurs when mycobacteria are dispersed throughout the body through the blood or the lymphatic system, or sometimes both. If the spread occurs through the bloodstream, then the foci form in the upper sections of the lungs. If the lymphatic system, then in the lower sections there is a large number of foci. While the generalized variant of the disseminated form is quite rare, it is with a predominant lesion of the lungs in almost 90% of cases.
There are many variants of the course of this form of the disease, as well as clinical manifestations. The onset of tuberculosis can be either subacute or chronic. In the first case, the disease begins sluggishly, the increase in symptoms occurs gradually, but the intoxication is quite pronounced. Lesions outside the lungs are often seen. This form is characteristic of both the first stage of the development of the disease and the second.
Cavernous pulmonary tuberculosis
The cavernous form has a number of features and is primarily characterized by the presence of a thin-walled cavity that appears on the lung tissue. Cavities begin to develop more actively when tuberculomas begin to disintegrate or with the progression of other forms of tuberculosis, more often infiltrative.
Primary infection is always latent. Bacteria most often enter the body through the aerogenic route. Catarrhal phenomena begin to appear later, when the walls around the cavity become thicker. The x-ray image shows a cavity that has the shape of a circle. Treatment occurs with several types of medications, in combination with physiotherapy and immunostimulating drugs.
Fibrous tuberculosis of the lungs
A distinctive feature of the fibrous form is the presence of a fibrous cavity, the appearance of corresponding changes in the lung tissue. In this case, the bronchi adjacent to the cavity are affected, emphysema, bronchiectasis, and pneumosclerosis often appear in the lungs.
The processes preceding the appearance of a fibrous cavity are infiltrative, tricky or disseminated forms of the disease. The number of foci can be both multiple and single, caverns appear both in one and in both lungs. There are several options for the development of the disease:
Thanks to chemotherapy, the disease subsides, exacerbation appears after a few years.
Periods of calm are often replaced by periods of exacerbation.
Sometimes, against the background of fibrous tuberculosis, complications begin to develop, more often with a progressive nature of the disease.
Focal pulmonary tuberculosis
This form is most often secondary. With it, a few foci appear, the place of their localization is different – both one and both lungs can be affected. The symptoms are not obvious. This form includes both fresh foci and old ones that have a fibrous nature of the lesion. They differ in density, composition, size.
A pronounced intoxication of the body with a cough, high body temperature and other symptoms in the focal form of the disease occurs during the exacerbation phase. If changes in the focal nature in the lungs do not show active signs, as can be seen from the X-ray examination, then tuberculosis is considered cured.
Open pulmonary tuberculosis
This form is the most dangerous. The lungs are most commonly affected, but other organs may also be involved. Infection occurs by inhalation of the infectious agent. A patient with an open form must be isolated.
This term should be understood as the fact that a person is contagious to others, as he releases active mycobacteria into the environment. The presence of an open form can be determined by examining a sputum smear.
Healing an open form is possible, although it is a rather complicated process. The difficulty lies in the fact that bacteria become resistant to many types of drugs. In addition, such people should be in long-term isolation from others.
Closed pulmonary tuberculosis
The closed form of the disease is the opposite of the open form. With it, there is no release into the external environment of mycobacteria that are infectious for people around.
This type of disease is much more common and may not manifest itself for a long time. Only the Mantoux test will be positive. According to some reports, a third of the world’s population is infected with this form of tuberculosis.
Complications and consequences of pulmonary tuberculosis

Complications of tuberculosis are pathological processes caused by the underlying disease. If the disease is not treated, then the most formidable consequence is the death of a person.
You can also highlight the following complications:
Other internal organs may be affected. Most often this happens when treatment is not started on time. In most cases, the liver suffers, its functioning is disrupted.
Joints can be affected, bone tuberculosis develops, leading to severe pain, swelling, arthritis, and sometimes abscesses.
Pulmonary bleeding is one of the formidable complications of the underlying disease. In this case, the person needs urgent medical attention.
Weakens the immune system, which leads to the vulnerability of the body to a variety of infections. The patient begins to suffer more often from flu, colds, etc.
Hemoptysis.
Pulmonary insufficiency.
Heart failure.
Broncholitis, in which a calcified formation is observed in the lumen of the bronchi.
Aspergilloma is a fungal infection of the lung tissue that can damage the wall of the blood vessel that is adjacent to the formation and cause pulmonary bleeding.
Tuberculoma is a growth resembling a tumor.
Reactivation of the tuberculosis process.
Bronchiectasis, in which a person develops nonspecific inflammation.
A person who once had tuberculosis is not immune from its consequences in the future. So, there are no guarantees that a woman will be able to give birth to an absolutely healthy child. He may have both physical and mental disabilities. Often there is a frozen pregnancy and the death of a child during childbirth.
Sometimes, after an illness, a person may suffer from headaches, discomfort in muscles and joints for some time. Most often, such a reaction is the result of treatment with potent drugs. Often, restoration of the work of the intestines and stomach is required, and stool disorder is observed.
Tuberculosis and lung cancer
The combination of tuberculosis and lung cancer in recent years is not uncommon. Recent studies show that TB survivors are 10 times more likely to develop lung cancer. Therefore, all people suffering from tuberculosis and overstepping the age limit of 40 years are considered to be at risk for oncology.
The most susceptible to lung cancer are long-term smokers, persons with metatuberculosis syndrome and those people who have been exposed to various carcinogenic factors for a long time.
Most often, the diagnosis of lung cancer is established in people with chronic forms of tuberculosis and fibrous formations in the tissues. Another problem of such people is the difficulty of diagnosis. X-ray examination may not give a complete picture and additional methods are required – cytological and histological. When lung cancer is detected, surgery is required.
Diagnosis of pulmonary tuberculosis

Diagnosis of the disease includes instrumental, immunological and laboratory research methods and consists of several successive stages:
Listening to patient complaints, doctors pay attention to the presence of shortness of breath, general weakness, weight loss, cough, as well as the nature of sputum.
Collecting the history of the development of the disease. At the same time, it is necessary to find out whether the person had contacts with patients with tuberculosis, how the disease began and how it proceeds.
General inspection, which includes monitoring the skin, examining the lymph nodes, listening to the lungs using a special device – a phonendoscope.
Mantoux test. At the same time, the antigen of the causative agent of the disease is injected under the human skin, after a few days the injection site and the body’s immune response are studied. If an infection has occurred, then the reaction will be quite pronounced: the stain is large. However, it should be understood that only with the help of this technique it is impossible to make a diagnosis, since the tuberculin test often gives false results.
X-rays of light. This study allows you to see some changes in them and suspect the presence of the disease. However, X-rays are not able to fully confirm the diagnosis or refute it.
Sputum analysis. At least three smears are subject to examination. If causative agents of the disease are found in the sputum, and characteristic changes are visible on the x-ray, then repeated analyzes are carried out to confirm the diagnosis. With a positive result, they determine the form of the disease and prescribe the appropriate treatment.
Additional research methods are the following:
Bronchoscopy, which allows using a special device to examine the lungs from the inside. Also during this study, flushing is performed from the alveoli and bronchi, then their cellular composition is studied and the presence of the pathogen is detected. If required, during bronchoscopy, the affected area is taken.
Puncture pleural area is done in the presence of tuberculous pleurisy in the lung. After its sampling, a study of the composition and the presence of the corresponding mycobacteria in it is carried out.
Biopsy of the affected area is made to study its cellular composition. If a granuloma is found, the diagnosis is no longer in doubt.
PCR. For this, blood is taken for analysis.
How is the treatment?

Treatment of the disease has specific goals:
Elimination of clinical manifestations, as well as laboratory signs of the disease.
Restoration of human performance. Bringing him back to normal life.
Sustained cessation of bacterial excretion, which must be confirmed by special studies.
Elimination of destructive, focal and infiltrative manifestations of the disease, the absence of active signs of the disease in x-ray examination.
Treatment is carried out in a tuberculosis dispensary. The leading method is the impact on mycobacteria with the help of drugs. At the same time, one drug is not enough, they are usually used in combination, according to a certain scheme.
Active against mycobacteria that cause disease are rifamycins, aminoglycazides, polypeptides, isonicotinic acid hydroside, pyrazinamide, cycloserine, thiamides, fluoroquinolones, etc. All of them have antibacterial and bacteriostatic properties.
If resistance of mycobacteria to drugs is observed and the treatment does not give the desired effect, then such drugs are used from the reserve treatment regimens.
Surgery
Sometimes the disease requires surgical intervention, but there are strict indications for this:
Chemotherapy did not have the desired effect, the person shows multiple drug resistance.
The disease caused irreversible changes in the pleura, lungs, bronchi and lymph nodes.
There are life-threatening complications caused by the disease.
Most often, surgical intervention is required when establishing cavernous, fibrous tuberculosis, as well as in case of tuberculoma. Although the operation is performed in other forms of the disease, but somewhat less frequently.
In most cases, operations for tuberculosis are planned, but sometimes emergency intervention is required. This occurs in life-threatening conditions such as tension pneumothorax, profuse pulmonary hemorrhage, etc.
Contraindications are the high prevalence of the process, serious violations of the respiratory function, kidney and liver diseases.
Prevention of pulmonary tuberculosis

The importance of preventive measures cannot be underestimated, given the prevalence of the disease among the population. The specific method includes, first of all, vaccination. The well-known BCG vaccine, which is given to children in the hospital. It is derived from a weakened strain of the disease-causing mycobacterium. The introduction is made to develop specific immunity. This vaccine does not give a 100% guarantee that a person will not get sick, but most likely he will have a mild form of tuberculosis. Immunity is maintained for 5 years, and then a person is revaccinated (at 7 and at 14 years). If there is evidence, then the vaccine should be administered before the person reaches 30 years of age, with a break of 5 years.
The fact that the Mantoux test after the introduction of the vaccine will be positive for 7 years is the norm. This indicates good immunity.
Such a screening method of examination as fluorography should be carried out annually. In addition to tuberculosis, it will allow you to identify other pathologies of the lungs at an early stage.
An important method of prevention is the exclusion of contact with patients. Naturally, it will not be possible to completely protect yourself from infection in this way, however, if there is information that a person is infected with an open form, then it is important to avoid contact with him.
Good nutrition, a healthy lifestyle, giving up bad habits – all this will help maintain immunity and help it resist Mycobacterium tuberculosis when it is possible to meet it.
Author of the article: Makarova Evgenia Vladimirovna, pulmonologist









