Contents
What is arterial hypertension?
Arterial hypertension is a disease of the cardiovascular system, in which the blood pressure in the arteries of the systemic (large) circulation is steadily increased.
Blood pressure is divided into systolic and diastolic:
Systolic. According to the first, upper number, the level of blood pressure is determined at the moment of compression of the heart and expulsion of blood from the artery. This indicator depends on the force with which the heart contracts, on the resistance of the walls of blood vessels and the frequency of contractions.
diastolic. The second, lower number determines the blood pressure at the moment when the heart muscle relaxes. It indicates the level of peripheral vascular resistance.
Normally, blood pressure readings are constantly changing. They physiologically depend on the age, gender and condition of the person. During sleep, pressure decreases, physical activity or stress leads to its increase.
The average normal blood pressure in a twenty-year-old person is 120/75 mm Hg. Art., forty years old – 130/80, over fifty – 135/84. With persistent figures of 140/90, we are talking about arterial hypertension.
Statistics show that about 20-30 percent of the adult population is affected by this disease. With age, the prevalence rate inexorably increases and by the age of 65, 50-65 percent of older people suffer from this disease.
Doctors call hypertension the “silent killer”, as the disease quietly but inexorably affects the work of almost all the most important human organs.
Symptoms of arterial hypertension
Symptoms of hypertension include:
Dizziness, feeling of heaviness in the head or in the eye sockets;
Pulsating pain in the back of the head, in the frontal and temporal parts, radiating to the orbits;
Feeling a pulse in the head;
Flashing glare or flies before the eyes;
Noise in ears;
Redness and face;
Swelling of the face after sleep, especially in the eyelids;
Feeling of tingling or numbness in the fingers;
Nausea;
swelling of the extremities;
increased sweating;
Periodic chills;
Internal tension and anxiety;
Tendency to irritability;
memory impairment;
Decreased overall performance;
Cardiopalmus.
Causes and risk factors of arterial hypertension
The main risk factors for hypertension include:
Floor. The greatest predisposition to the development of the disease is observed in men aged 35 to 50 years. In women, the risk of hypertension increases significantly after menopause.
Age. High blood pressure is more common among people over the age of 35. Moreover, the older a person becomes, the higher the numbers of his blood pressure.
Наследственность. If first-line relatives (parents, siblings, grandparents) suffered from this disease, then the risk of developing it is very high. It increases significantly if two or more relatives had high blood pressure.
Stress and increased psycho-emotional stress. In stressful situations, adrenaline is released, under its influence the heart beats faster and pumps blood in large volumes, increasing pressure. When a person is in this state for a long time, the increased load leads to vascular wear, and increased blood pressure is converted into chronic.
Drinking alcoholic beverages. Addiction to the daily consumption of strong alcohol increases blood pressure by 5 mm Hg. Art. Every year.
Smoking. Tobacco smoke, getting into the blood, provokes vasospasm. Damage to the walls of the arteries causes not only nicotine, but also other components contained in it. Atherosclerotic plaques appear at the site of damage to the arteries.
Atherosclerosis. Excess cholesterol, as well as smoking, lead to a loss of elasticity in the arteries. Atherosclerotic plaques interfere with free blood circulation, as they narrow the lumen of blood vessels, due to which blood pressure rises, spurring the development of atherosclerosis. These diseases are interrelated risk factors.
Increased consumption of table salt. Modern people consume with food much more salt than the human body needs. Excess dietary sodium provokes a spasm of the arteries, retains fluid in the body, which together leads to the development of hypertension.
Obesity. Obese people have higher blood pressure than normal weight people. Abundant content of animal fats in the diet causes atherosclerosis. Lack of physical activity and excessive consumption of salty foods lead to the development of hypertension. It is known that for every extra kilogram there are 2 units of blood pressure.
Hypodynamia. A sedentary lifestyle increases the risk of developing hypertension by 20-50%. A heart that is not accustomed to stress copes with them much worse. In addition, the metabolism slows down. Lack of physical activity seriously weakens the nervous system and the human body as a whole. All of these factors contribute to the development of hypertension.
Degrees of arterial hypertension

The clinical picture of hypertension is affected by the stage and type of disease. In order to assess the level of damage to internal organs as a result of persistently elevated blood pressure, there is a special classification of hypertension, consisting of three degrees.
Arterial hypertension of the 1st degree
Manifestations of changes in target organs are absent. This is a “mild” form of hypertension, which is characterized by periodic rises in blood pressure and an independent return to normal values. Pressure surges are accompanied by mild headaches, sometimes sleep disturbance and fatigue during mental work.
Systolic pressure indicators range from 140-159 mm Hg. Art., diastolic – 90-99.
Arterial hypertension of the 2st degree
“Moderate” form. At this stage, it is already possible to observe objective lesions of some organs.
Diagnosed:
localized or widespread narrowing of the coronary vessels and arteries, the presence of atherosclerotic plaques;
hypertrophy (enlargement) of the left ventricle of the heart;
renal failure in a chronic form;
constriction of retinal vessels.
With this degree of remission are rarely observed, high blood pressure parameters are persistently maintained. Upper pressure indicators (SBP) – from 160 to 179 mm Hg. Art., lower (DAD) – 100-109.
Arterial hypertension of the 3st degree
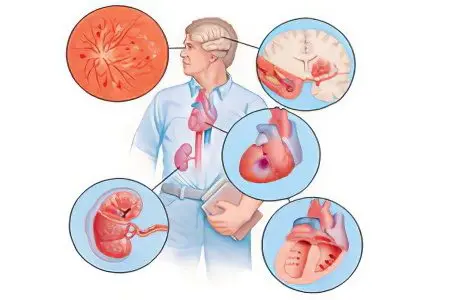
This is a severe form of the disease. It is characterized by a violation of the blood supply to the organs, and, as a result, is accompanied by the following clinical manifestations:
from the side of the cardiovascular system: heart failure, angina pectoris, development of myocardial infarction, blockage of the arteries, detachment of the walls of the aorta;
retina: papilledema, hemorrhages;
brain: transient disorders of cerebral circulation, stroke, vascular dementia, hypertensive encephalopathy;
kidneys: renal insufficiency.
Many of the above manifestations can be fatal. With hypertension of the III degree, the upper pressure is stable 180 and above, the lower one – from 110 mm Hg. Art.
Types of arterial hypertension
In addition to the above classification according to the level of blood pressure, on the basis of differential parameters, doctors divide arterial hypertension into types by origin.
Primary arterial hypertension
The causes of this type of disease have not yet been clarified. However, it is this form that is observed in 95 percent of people suffering from high blood pressure. The only reliable information is that heredity plays a major role in the development of primary hypertension. Geneticists claim that the human genetic code contains more than 20 combinations that contribute to the development of hypertension.
In turn, primary arterial hypertension is divided into several forms:
Hyperdrenergic. This form occurs in approximately 15 percent of cases of early hypertension, and often in young people. It occurs due to the release of adrenaline and norepinephrine into the blood.
Characteristic symptoms: discoloration of the face (the person may turn pale or red), a feeling of a pulse in the head, chills and a feeling of anxiety. Pulse at rest – from 90 to 95 beats per minute. If the pressure does not return to normal, a hypertensive crisis may follow.
Hyporeninic. Occurs in older people. A high level of aldosterone, a hormone of the adrenal cortex that retains sodium and fluid in the body, in combination with the activity of renin (a component that regulates blood pressure) in the blood plasma creates favorable conditions for the development of this type of hypertension. The external manifestation of the disease is a characteristic “kidney appearance”. Patients should refrain from eating salty foods and drinking plenty of water.
Hyperreninous. This form affects people with hypertension, progressing rapidly. The frequency of cases is 15-20 percent, and often these are young men. It is characterized by a severe course, sharp jumps in blood pressure are typical. SBP can reach 230, DBP – 130 mm Hg. Art. With an increase in blood pressure, the patient feels dizzy, intense headache, nausea and vomiting. Left untreated, the disease can cause atherosclerosis of the renal arteries.
Secondary arterial hypertension
This type is called symptomatic hypertension, as it develops with third-party lesions of the systems and organs responsible for the regulation of blood pressure. Its cause can be identified. In fact, this form of hypertension is a complication of another disease, which makes its treatment more difficult.
Secondary hypertension is also divided into various forms, depending on which disease caused the hypertension:
Renal (renovascular). The narrowing of the renal artery impairs blood circulation in the kidneys, in response to this, they synthesize substances that increase blood pressure.
The causes of narrowing of the artery are: atherosclerosis of the abdominal aorta, atherosclerotic plaques of the renal artery and inflammation of its walls, blockage by a thrombus, trauma, compression by a hematoma or tumor. Congenital dysplasia of the renal artery is not excluded. Renal hypertension can also develop against the background of glomerulonephritis, amyloidosis or pyelonephritis of the kidneys.
With all the complexity of the disease, a person can feel quite normal and not lose working capacity even with very high blood pressure. Patients note that a pressure jump is preceded by characteristic pain in the lower back. This form is difficult to treat, in order to cope with the disease, it is necessary to cure the primary disease.
Endocrine. In accordance with the name, it occurs in diseases of the endocrine system, among them: pheochromocytoma – a tumor disease in which the tumor is localized in the adrenal glands. It is relatively rare, but causes a very severe form of hypertension. It is characterized by both sharp jumps in blood pressure and persistent high blood pressure. Patients complain of visual impairment, headache and heart palpitations.
Another cause of the endocrine form of hypertension is Conn’s syndrome. It is manifested by hyperplasia or a tumor of the adrenal cortex and is characterized by excessive secretion of aldosterone, which is responsible for kidney function. The disease provokes an increase in blood pressure, accompanied by headache, numbness of different parts of the body, weakness. The work of the kidneys is gradually disrupted.
Syndrome Itsenko-Cushing. The disease develops due to the increased content of glucocorticoid hormones produced by the adrenal cortex. Also accompanied by high blood pressure.
Hemodynamic. May present in advanced heart failure and congenital partial narrowing (coarctation) of the aorta. At the same time, blood pressure in the vessels extending from the aorta above the narrowing area is significantly increased, lower – reduced.
Neurogenic. The reason is atherosclerotic lesions of the vessels of the brain and brain tumors, encephalitis, encephalopathy.
Medicinal. Some medications that are taken on a regular basis have side effects. Against this background, arterial hypertension may develop. The development of this form of secondary hypertension can be avoided if you do not self-medicate and carefully read the instructions for use.
Essential arterial hypertension
This species can be combined with primary hypertension, since its only clinical sign is long-term and persistent high blood pressure in the arteries. It is diagnosed by exclusion of all forms of secondary hypertension.
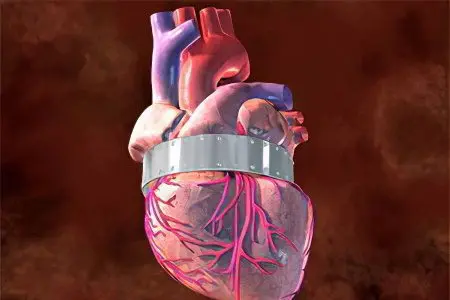
Hypertension is based on dysfunctions of various systems of the human body that affect the regulation of vascular tone. The result of this influence is a spasm of the arteries, a change in vascular tone and an increase in blood pressure. Left untreated, the arterioles become sclerotic, making the elevated BP more persistent. As a result, organs and tissues receive less nutrition, which leads to disruption of their functions and morphological changes. In different periods of the course of hypertension, these changes appear, but first of all, they always concern the heart and blood vessels.
The disease is finally formed when depressor renal function is depleted.
Pulmonary arterial hypertension
This type of hypertension is very rare, the incidence is 15-25 people per million. The cause of the disease is high blood pressure in the pulmonary arteries connecting the heart and lungs.
The pulmonary arteries transport blood containing a low proportion of oxygen from the right ventricle of the heart (lower right side) to the small vessels and arteries of the lungs. Here it is saturated with oxygen and goes back, only now to the left ventricle, and from here it diverges throughout the human body.
In PAH, blood is not able to freely circulate through the vessels due to their narrowing, increases in thickness and mass, edema of the vascular walls caused by inflammation, and the formation of clots. This violation leads to damage to the heart, lungs and other organs.
In turn, PAH is also divided into types:
hereditary type. The cause of the disease is genetic problems.
Idiopathic. The origin of this type of PAH has not yet been established.
Associate. The disease develops against the background of other diseases, such as HIV, liver disease. May occur due to the abuse of various pills to normalize body weight, drugs (amphetamines, cocaine).
Persistent elevated blood pressure significantly increases the load on the heart, the affected vessels interfere with normal blood circulation, which over time can cause the right ventricle of the heart to stop.
Labile arterial hypertension
This type of hypertension is referred to as the initial stage of hypertension. Actually, this is not yet a disease, but rather a borderline condition, since it is characterized by minor and unstable pressure surges. It stabilizes on its own and does not require the use of drugs that reduce blood pressure.
In principle, people with labile hypertension are considered quite healthy (provided that the pressure returns to normal without intervention), but they need to closely monitor their condition, since blood pressure is still not stable. In addition, this type may be a harbinger of the secondary form of hypertension.
Diagnosis of arterial hypertension

Diagnosis of hypertension is based on three main methods:
The first is the measurement of blood pressure;
The second is a physical examination. Comprehensive examination, which is carried out directly by the doctor. These include: palpation, auscultation (listening to the sounds that accompany the work of various organs), percussion (tapping of different parts of the body, followed by sound analysis), routine examination;
The third is an electrocardiogram.
Now let’s proceed to the description of all diagnostic measures for suspected arterial hypertension:
AD control. The first thing your doctor will do is measure your blood pressure. It makes no sense to describe the method of measuring pressure using a tonometer. This technique requires special training, and an amateurish approach will give distorted results. But we recall that the permissible limits of blood pressure for an adult range from 120-140 – upper pressure, 80-90 – lower.
In people with an “unstable” nervous system, blood pressure indicators increase with the slightest emotional outbursts. When visiting a doctor, a “white coat” syndrome may be observed, that is, during a control measurement of blood pressure, a rise in pressure occurs. The reason for such jumps is stress, this is not a disease, but such a reaction can cause disruption of the heart and kidneys. In this regard, the doctor will measure the pressure several times, and in different conditions.
Inspection. Height, weight, body mass index are specified, signs of symptomatic hypertension are revealed.
Medical history. Any visit to the doctor usually begins with a doctor’s interview with the patient. The task of a specialist is to find out from a person the diseases that he suffered before and has at the moment. Analyze risk factors and evaluate lifestyle (does a person smoke, how does he eat, does he have high cholesterol, does he suffer from diabetes), did first-line relatives suffer from hypertension.
physical examination. First of all, the doctor examines the heart to detect murmurs, changes in tones and the presence of uncharacteristic sounds using a phonendoscope. Based on these data, preliminary conclusions can be drawn about changes in the heart tissue due to high blood pressure. And also to exclude vices.
Blood chemistry. The results of the study allow us to determine the level of sugar, lipoproteins and cholesterol, on the basis of which we can conclude that the patient is prone to atherosclerosis.
ECG. An electrocardiogram is an indispensable diagnostic method for detecting cardiac arrhythmias. In addition, according to the results of an echocardiogram, it is possible to determine the presence of hypertrophy of the wall of the left side of the heart, characteristic of hypertension.
Ultrasound of the heart. With the help of echocardiography, the doctor receives the necessary information about the presence of changes and defects in the heart, the function and condition of the valves.
X-ray examination. Arteriography and aortography are used in the diagnosis of hypertension. This method allows you to examine the arterial walls and their lumen, exclude the presence of atherosclerotic plaques, congenital narrowing of the aorta (coarctation).
Dopplerography. Ultrasound examination, which allows to determine the intensity of blood flow through the arteries and veins. When diagnosing arterial hypertension, the doctor is primarily interested in the condition of the cerebral and carotid arteries. For this purpose, it is ultrasound that is most often used, since it is completely safe, and after its use there are no complications.
Ultrasound of the thyroid gland. Simultaneously with this study, the doctor needs the results of a blood test for the content of hormones produced by the thyroid gland. Based on the results, the doctor will be able to determine what role the thyroid gland plays in the development of hypertension.
Ultrasound of the kidneys. The study makes it possible to assess the condition of the kidneys and renal vessels.
Treatment of arterial hypertension

Non-drug treatment is prescribed to all patients with hypertension without exception, as it increases the effect of drug therapy and significantly reduces the need for antihypertensive drugs.
First of all, it is based on changing the lifestyle of a patient suffering from arterial hypertension. It is recommended to avoid:
smoking if the patient smokes;
drinking alcoholic beverages, or reducing their intake: for men up to 20-30 grams of ethanol per day, for women, respectively, up to 10-20;
increased consumption of table salt with food, it must be reduced to 5 grams per day, preferably less;
the use of drugs containing potassium, magnesium or calcium. They are often used to lower high blood pressure.
In addition, the doctor will strongly recommend:
overweight patients to normalize body weight, for which it is sometimes better to contact a nutritionist for a diet that allows you to eat a balanced diet;
increase physical activity by exercising regularly;
Introduce more fruits and vegetables into your nutritious diet while reducing your intake of foods rich in saturated fatty acids.
With “high” and “very high” risks of cardiovascular complications, the doctor will immediately begin to use drug therapy. The specialist will take into account the indications, the presence and severity of contraindications, as well as the cost of drugs when prescribing them.
As a rule, medicines with a daily duration of action are used, which makes it possible to prescribe a one-, two-time intake. In order to avoid side effects, taking the drugs begins with a minimum dosage.
We list the main drug hypertensive drugs:
In total, there are six groups of hypertensive drugs that are currently used. Among them, beta-blockers and thiazide diuretics are leading in terms of effectiveness.
Again, drug treatment, in this case, thiazide diuretics, should be started with small doses. If the effect of taking is not observed, or the patient does not tolerate the drug well, minimal doses of beta-blockers are prescribed.
Thiazide diuretics are positioned as:
first-line drugs for the treatment of hypertension;
the optimal dose is the minimum effective.
Diuretics are prescribed for:
heart failure;
arterial hypertension in the elderly;
diabetes mellitus;
high coronary risk;
systolic hypertension.
Diuretics are contraindicated in gout, and in some cases, during pregnancy.
Indications for the use of beta-blockers:
a combination of angina pectoris with hypertension and with a previous myocardial infarction;
the presence of increased coronary risk;
tachyarrhythmia.
The drug is contraindicated in:
bronchial asthma;
obliterating vascular diseases;
chronic obstructive pulmonary disease.
In the drug therapy of hypertension, doctors use combinations of drugs, the appointment of which is considered rational. In addition, according to indications, it can be prescribed:
antithrombocidal therapy – for the prevention of stroke, myocardial infarction and vascular death;
taking lipid-lowering drugs, in the presence of multiple risk factors;
combined drug treatment. It is prescribed in the absence of the effect expected from the use of monotherapy.
Prevention of arterial hypertension

AH is easier to prevent than to cure. Therefore, it is worth thinking about preventive measures even in youth. This is especially important for people who have relatives suffering from arterial hypertension.
Prevention of hypertension is designed to eliminate factors that increase the risk of developing this formidable disease. First of all, you need to get rid of bad habits and change your lifestyle in the direction of increasing physical activity. Sports, running and walking outdoors, regular swimming in the pool, water aerobics significantly reduce the risk of developing hypertension. Your heart will gradually get used to the loads, blood circulation will improve, due to which the internal organs will receive nutrition, metabolism will improve.
In addition, it is worth protecting yourself from stress, but if you can’t, then at least learn how to respond to them with a healthy dose of skepticism.
If possible, it is worth buying modern devices for monitoring blood pressure and pulse. Even if you do not know what high blood pressure is, as a preventive measure, you should periodically measure it. Since the initial (labile) stage of hypertension can be asymptomatic.
People over the age of 40 should undergo annual preventive examinations with cardiologists and therapists.









