Contents
Staphylococcus in the throat is the presence in the mucous membrane of the pharynx or larynx of a bacterium that can cause an infectious and inflammatory process. The microbe can exist there as a conditionally pathogenic microflora, that is, without causing a disease, but can cause an inflammatory reaction.
Staphylococcus aureus is considered the most dangerous, since it more often than other species (epidermal and saprophytic) causes disease and is the most aggressive.
According to statistics, every fifth inhabitant of the Earth is its carrier, but not all of them cause immediate inflammation in the throat. Staphylococcus aureus can simply exist in the mucous membranes of the throat, and not manifest itself in any way until favorable conditions arise for this (weakening of the body’s immune forces, SARS, influenza, etc.).
Symptoms of staphylococcus in the throat

Against the background of provoking factors, staphylococcus in the throat can cause a number of diseases, including: staphylococcal tonsillitis, staphylococcal pharyngitis and staphylococcal laryngitis. Each of these diseases has distinctive symptoms that should be considered separately.
Symptoms of staphylococcal tonsillitis:
Acute onset with fever up to 40 °C;
Sharp hyperemia of the mucous membrane of the pharynx and tonsils;
Hilly surface of the tonsils with the appearance of purulent deposits on them;
Overlays are easily removed, often affecting the temples and tongue, their color is whitish-yellow;
Symptoms of acute intoxication: headache, weakness, lacrimation;
Sharp pain in the throat with irradiation to the temple, ear, neck;
Vertigo when trying to get up;
Chills;
Inability to eat due to pain, loss of appetite;
Enlarged lymph nodes in the neck.
Symptoms of staphylococcal pharyngitis (occurs infrequently, in about 5% of cases):
Inflammation of the mucous membrane of the throat with its swelling and hyperemia, desquamation of the epithelium;
Accumulation of viscous mucous deposits on the back of the throat;
Sore throat, which manifests itself in the form of a dry cough;
Hoarseness of voice;
Sore throat;
Increased fatigue, general malaise;
Increased body temperature.
Symptoms of staphylococcal laryngitis:
Inflammation of the mucous membrane of the larynx, often with the capture of the trachea and the development of tracheitis;
The presence of purulent discharge;
Pain in the larynx, aggravated by swallowing;
Feeling of dryness and itching;
Change in timbre, pitch and strength of the voice, sometimes to complete loss of voice and pronounced hoarseness;
The disease at the beginning is accompanied by a dry cough, which, as it progresses, becomes wet;
Separation of sputum during expectoration;
An increase in temperature, most often slightly above subfebrile marks.
Staphylococcal infection, if left untreated, will progress with the capture of the lower respiratory tract – the trachea and bronchi, and, with the transition to the lung tissue.
How is staphylococcus transmitted in the throat?
Staphylococcus can get into the throat in several ways, including:
contact route of transmission. The bacterium enters the mucous membrane of the throat as a result of interaction with various household items and common use. In the children’s team, infection often occurs through contact with toys and as a result of direct interaction between the skin of the hands and the oral mucosa. Insufficient compliance with hygiene rules plays a huge role.
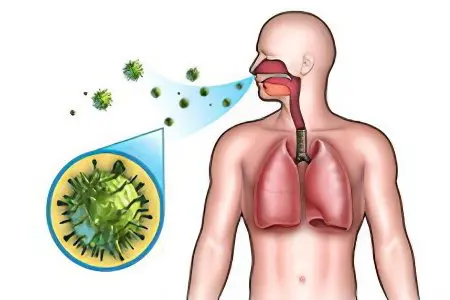
airborne way, which is based on the fact that a person inhales the air, which contains microscopic staphylococcus bacteria. They enter the environment with the secretions of an infected organism, when coughing, sneezing, breathing and talking.
With ingestion of dust particlescontaining mycobacteria. Staphylococcus is a fairly hardy microorganism and can exist in dust and on woolen fabrics for up to six months.
Alimentary route of infectionwhich should be given maximum attention. Bacteria can get on food as a result of improper cooking technology, poor-quality processing of dishes or hands. Children often become infected during breastfeeding, from an infected mother. Therefore, it is important for women not only to monitor breast hygiene, but also to sanitize possible foci of infection in a timely manner (carious teeth, rhinitis, sinusitis, etc.).
intrauterine infection, during the passage of the child through the birth canal and with the penetration of infected amniotic fluid.
Artifical route of transmission of the bacteriumwhen it enters the throat as a result of non-compliance with sanitary and hygienic measures by medical personnel, for example, when undergoing an examination such as bronchoscopy.
autoinfectious route of infection, that is, when, under the influence of certain factors, the previously asymptomatic carriage of a bacterium turns into a disease. The trigger mechanism to increase the activity of bacteria can be: reduced immunity, irrational use of antibacterial agents, SARS, damage to the mucous membrane of the throat or oral cavity, hypothermia and frequent stress.
What is dangerous staphylococcus in the throat?
The existence of bacteria in the throat can be a potential threat to human health. If, with a normal immune status, the growth and development of staphylococcus is restrained by the body’s own forces, then when it falls, it leads to the development of infectious processes.
Manifesting in the throat, the disease, as it develops, can move further, capturing organs and organ systems of a person who does not receive adequate treatment. It exacerbates existing chronic diseases, such as diabetes, rheumatoid arthritis, increases the body’s vulnerability to other bacteria, such as pneumococci, streptococci. In the most advanced cases, a staph infection in the throat can affect the lymphatics and lead to septicemia. These conditions, in turn, threaten serious health problems, even death. However, such threats of the presence of staphylococcus in the throat exist only if the person does not receive adequate therapy.
Staphylococcus aureus in the throat
It was Staphylococcus aureus that was recognized by doctors as the most dangerous variety of bacteria, primarily due to the fact that it has a high virulence and the ability to develop resistance to most antibacterial and antiseptic agents.
Settling in the throat, the bacterium causes sore throats, laryngitis, pharyngitis. Often, small ulcers and erosion are observed on the mucous membrane of the throat. Staphylococcus aureus is especially dangerous for young children. Their immune system is weak enough to resist the toxins produced by the bacteria, and the infection process is particularly acute in them.
In addition, the treatment of this particular type of bacterium is of particular difficulty, often purulent overlays and necrotic areas are subject to surgical removal.
Another danger of the presence of Staphylococcus aureus in the throat is its ability to migrate throughout the body. It can settle on distant organs and joints, lead to meningitis, endocarditis, osteomyelitis, pneumonia, sepsis, and toxic shock.
The bacterium is dangerous for the fetus, since the toxins it produces can lead to sepsis and pemphigus in newborns.
You can identify the bacterium with the help of bakposev, taken from purulent sores in the throat. In parallel, it is imperative to test for sensitivity to antibiotics. It is they who are prescribed to eliminate bacteria from the throat, often supplementing treatment with a staphylococcal bacteriophage.
Treatment of staphylococcus in the throat

The elimination of bacteria using medications is necessary if they caused an infectious-inflammatory process or their number exceeds the maximum allowable value of 104 units.
The basis of drug therapy is antibiotics. But to which antibiotics the bacterium does not have immunity, the tank-seeding will show, therefore, only the therapist prescribes treatment, after passing the tests.
If there are rashes in the oral cavity, then they must first be opened and then treated with an antibacterial drug to which sensitivity has been identified.
In addition, bacteriophages are used to eliminate bacteria. They are viruses that, after being introduced into the body, begin to eliminate certain types of bacteria.
Antibacterial therapy must necessarily be supplemented with immunotherapy. For this purpose, immunostimulants, immunoglobulins and a large amount of water are prescribed.
In addition to taking medicines inside, the patient will need local treatment with antiseptics. Lubrication of the oral cavity and tonsils after their cleansing and disinfection may be prescribed.
Diet. The fight against bacteria in the throat can take a long time. For the period of treatment, it is necessary to abandon the use of fried, spicy, salty, spicy, fatty foods. It not only undermines the body’s defenses, but also contributes to irritation of the throat mucosa, which delays recovery. It is important to enrich your diet with foods that include vitamin C.
Other diseases In addition to the direct fight against the bacterium, the patient will need to get rid of all possible foci of infection. Among them: adenoids, sinusitis, caries, etc. It is important to carry out parallel treatment of concomitant diseases. Often inflammation is accompanied by a viral infection, such as influenza. Therefore, it is important to carry out symptomatic treatment of concomitant diseases.
When pregnancy. Separately, it should be said about the treatment of a dangerous bacterium of women bearing a child. In the presence of an inflammatory process, a therapeutic effect is necessary for them, since staphylococcus aureus, especially Staphylococcus aureus, is a direct threat to the health and life of the fetus. But since most drugs are contraindicated during this period, they are prescribed to perform gargles with chlorphyllipt and irrigate it with an IRS-19 spray. In addition, drugs to increase immunity may be recommended. Two weeks later, the woman needs to be re-examined. After that, the question of the need to take antibacterial agents will be decided.
If the infectious process was diagnosed in time, and the disinfectant was correctly selected, then full recovery can be observed after two weeks.









