Contents
Hemolytic anemia is a group of diseases that are united by one common feature, namely, a shortened life cycle of red blood cells. During the death of red blood cells, the cells lose hemoglobin. He, once in a free state, is also subject to destruction. This process is called hemolysis. Hemolysis is the underlying hemolytic anemia. This is the only thing that unites these two pathological processes, the etiology and pathogenesis of hemolysis and hemolytic anemia are different. The same applies to their symptoms and prognosis.
“Hemolytic anemia – what is it in simple words?” – this is one of the frequent questions that patients ask the doctor when they first encounter a similar diagnosis. This is not surprising, because pathology is rare, no more than 1% of the world’s population. However, in the structure of other types of anemia, hemolytic anemia occupy 11%. So, hemolytic anemia, in simple terms, is a disease of erythrocytes (red blood cells), which, as a result of this disease, are destroyed and release a large amount of indirect bilirubin into the blood.
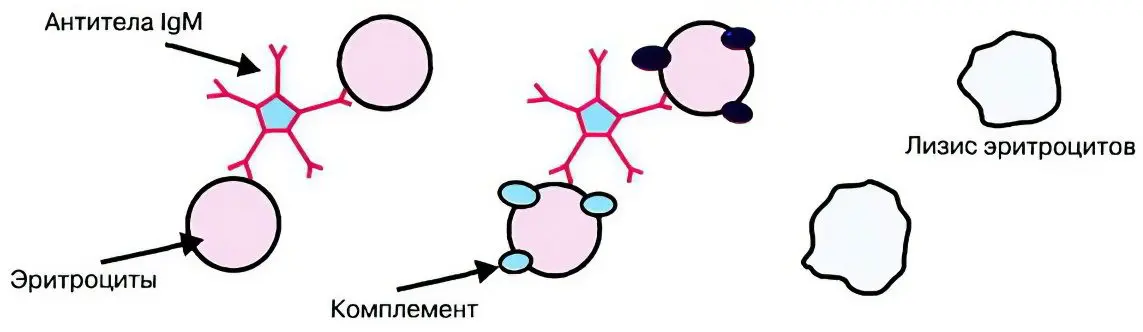
The picture below shows the hemolysis of an erythrocyte:

Hemolytic anemia – what is it?
The lifespan of red blood cells in a healthy person ranges from 80 days to 4 months. If he develops hemolytic anemia, then the maximum life span of red blood cells is reduced to 50 days. In severe cases of the disease, this period does not exceed 14 days.
Hemolysis is a process that refers to the massive early death of red blood cells. It is not normal for a person.
Hemolysis can occur inside the cells of organs and tissues, that is, outside the vascular bed. First of all, the liver, spleen, red bone marrow suffer. Also, hemolysis can start extracellularly, inside the vascular bed. This process is also called intravascular hemolysis.
Naturally, the early death of erythrocytes cannot be asymptomatic. Signs of the disease are easy to determine both during the examination of the patient and with the help of laboratory tests.
Hemolytic anemia with intracellular hemolysis
The destruction of erythrocytes outside the vascular bed is carried out mainly in the spleen. They die because they are affected by mononuclear phagocytes (macrophages). The person himself can pay attention to the fact that not everything is in order with the body. After all, his skin and feces change color. Seeing a doctor will confirm the diagnosis.

So, the symptoms that indicate intracellular hemolysis in anemia:
The skin and mucous membranes become yellow. The intensity of the color depends on the massiveness of the destruction of red blood cells. In the blood, a significant increase in the level of free bilirubin will be noticeable.
Since the level of bilirubin is characterized by pathological growth, the liver directs efforts to neutralize it. This leads to the fact that the bile is painted in a bright saturated color. The level of bile pigments in it increases, which entails a high probability of the appearance of stones in the gallbladder.
Highly concentrated bile enters the intestine, which leads to an increase in the level of urobilinogen and stercobilin. As a result, the stool becomes very dark in color.
Urine darkens due to an increase in the concentration of urobilin in it.
The level of erythrocytes in the blood decreases. The red bone marrow tries to cover the needs of the body and begins to synthesize young red blood cells called reticulocytes with a vengeance. This leads to the fact that their level in the blood rises.
Hemolytic anemia with intravascular hemolysis
If red blood cells begin to break down in the blood vessels, then this is expressed by the following symptoms:
The level of hemoglobin in the blood rises, it is released from the destroyed red blood cells.
In the blood, hemoglobin can remain unchanged or in the form of hemosiderin. From the blood, it enters the urine, giving it an uncharacteristic color: black, brown or red.
Part of the hemoglobin that breaks down is not excreted in the urine, it is stored in the body. This iron-containing pigment accumulates in the bone marrow and in the internal organs.
Previously, there was a classification of hemolytic anemia only at the site of destruction of red blood cells. That is, intravascular and intracellular anemia were isolated. Modern medicine considers hemolytic anemia from a slightly different point of view.
Classification of hemolytic anemia
Depending on the etiology and pathogenesis of hemolytic anemia, the following varieties are distinguished:
Hemolytic anemia inherited. They, in turn, are divided into: membranopathies (microspherocytosis and ovalocytosis), hemoglobinopathies (sickle cell anemia and thalassemia) and anemia caused by enzyme defects with G-6-PDS deficiency.
Hemolytic anemias acquired during life are differentiated depending on the influence of which pathological factor they developed. So, the destruction of erythrocytes can be caused by exposure to antibodies, toxic compounds, and their mechanical damage.
More often than others, people develop hemolytic anemia due to autoimmune processes in the body.
So, hemolytic anemia acquired during life has a number of differences, namely:
Anemia that manifests against the background of exposure to anti-erythrocyte antibodies on red blood cells (autoimmune hemolytic anemia). This also includes hemolytic disease of the newborn, which manifests itself when isoantibodies enter the child’s body.
Anemia that develops with somatic mutations that disrupt the red blood cell membrane. A striking example of such anemia is paroxysmal cold nocturnal hemoglobinuria.
Anemia, which develops due to exposure to the human body of various chemical compounds. Danger in this regard are poisons, salts of heavy metals, organic acids.
Lack of vitamin E can lead to the development of hemolytic anemia.
Hemolytic anemia can act as a symptom of swamp fever. They lead to it a parasitic disease – malaria, which a person becomes infected due to the penetration of malarial plasmodium into the blood. This happens when an infected mosquito bites.
Hemolytic anemia, inherited
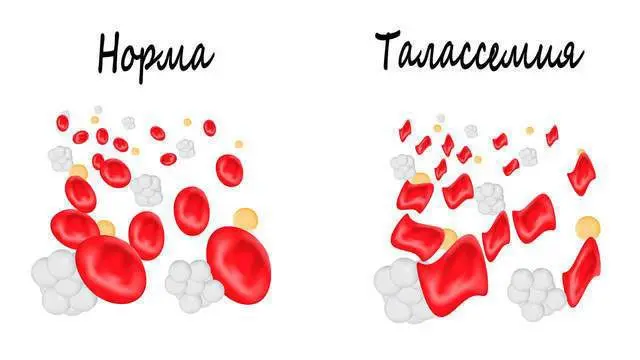
Thalassemia in a child
Thalassemia is an anemia that is based on a birth defect in the transfer RNA or gene regulator. The rate of production of one of the globin chains – alpha, beta or gamma – is also disrupted. All this, together, leads to the development of thalassemia. More often than others, people have a violation in the production of beta chains, so the diagnosis made sounds predominantly like beta thalassemia. At the same time, the concentration of normal hemoglobin decreases, and the concentration of abnormal hemoglobin increases (HbF and HbA2).
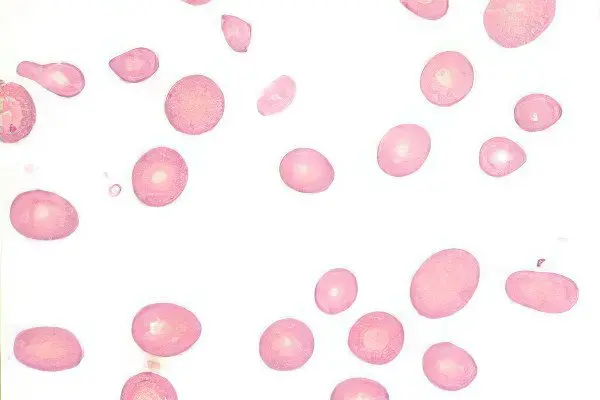
The erythrocytes, which are the transporters of the modified abnormal hemoglobin, are very thin-walled, delicate, and decompose quickly. Often they are not able to penetrate the capillaries, as their wall is too thin. As a result, the person develops symptoms of thalassemia.
There are two options for the course of the disease:
Homozygous form or Cooley’s disease, which develops in childhood.
Heterozygous form or thalassemia minor. The disease is most often discovered by chance, during a blood test. The disorder is diagnosed in adulthood.
Thalassemia minor may not manifest itself at all, so a person sometimes does not even suspect about the existing disorders in his body. The course of the pathology is mild. Thalassemia major has a severe course, it develops in children of the first year of life, gives multiple complications.
The following symptoms will indicate Cooley’s disease:
Pale skin, its yellow coloration, which can be quite intense.
Weakness, fatigue and lethargy.
Enlargement of the spleen in size, which is especially noticeable in childhood. The liver may also increase in size.
The level of red blood cells in the blood may remain normal, and the level of hemoglobin decreases.
The child will be somewhat behind in development, such children begin to crawl later, their appetite is disturbed, the child does not walk well.
Sometimes Cooley’s disease can be confused with hepatitis. To make a differential diagnosis, it is necessary to study the family history, as well as pay attention to such a blood indicator as bilirubin. In Cooley’s disease, the level of free bilirubin, as well as the level of bilirubin fractions HbF and HbA2 will be raised. In addition, the concentration of reticulocytes in the blood increases, and urobilin appears in the urine.
The therapy is reduced to the implementation of the following steps:
RBC transfusion, provided that the hemoglobin level is significantly reduced.
Passing a course of desferal therapy, which allows you to prevent the development of hemosiderosis.
Splenectomy.
Folic acid intake.
Bone marrow transplantation.
Ferrotherapy is not prescribed for thalassemia.
Minkowski-Choffard disease

Minkowski-Chauffard disease (microspherocytic membranopathy) is transmitted in an autosomal dominant manner. In this case, the patient has a congenital defect in the membranes of erythrocytes, in which they acquire a spherical shape. Whereas normal healthy red blood cells are disc-shaped. This enables them to penetrate through the narrowest passages of the capillary network. Erythrocytes, which have a spherical shape, cannot squeeze through small vessels, and when they try to do this, they are destroyed. Moreover, spherical erythrocytes let in more sodium ions than necessary. As a result, the red blood cells spend the maximum amount of energy, which also shortens their lifespan.
Pathology can manifest at any age, but the younger the child, the more difficult it will be. Minkowski-Shoffard disease is especially dangerous during the neonatal period.
Hemolytic syndrome is the main symptom of Minkowski-Choffard disease. It can develop for no apparent reason, either against the background of increased loads, after injuries, or after severe hypothermia of the body. Pathology enters a phase of exacerbation, and then is replaced by a period of calm. In addition, the disease leads to such developmental anomalies as: tower skull, cleft lip, defects in internal organs, heart defects.
Other symptoms of hereditary microspherocytosis:
Severe yellowness of the skin. If a patient develops acute hemolytic anemia, then it will be simply impossible not to notice a change in skin color.
Unexplained weakness.
High body temperature that peaks during the acute phase.
Pain in the muscles, pain in the right hypochondrium, in the abdomen.
Tachycardia, drop in blood pressure, heart murmurs.
Enlargement of the spleen in size.
Darkening of urine and feces.
If at the first examination of the patient the doctor can confuse anemia with viral hepatitis, then the results of laboratory tests will disprove this diagnosis.
A general blood test will reveal a decrease in the level of hemoglobin and red blood cells in the blood. Moreover, most red blood cells will have the shape of a sphere, and their size will decrease.
In addition, the level of reticulocytes rises, autohemolysis increases, there is more bilirubin in the blood, and the osmotic resistance of erythrocytes decreases. In the analysis of feces, the level of stercobilin will be exceeded, and in the analysis of urine – the level of urobilin.
If the disease is severe, then the patient is transfused with erythrocyte mass. B vitamins and iron preparations are not prescribed for this type of anemia, since their effectiveness will be zero. To improve the patient’s condition, the removal of the spleen is required, but this operation does not completely solve the problem.
Other hereditary causes
Of course, in addition to the two diseases described, there are other hereditary hemolytic anemias. They are quite rare.
Such diseases include:
sickle cell anemia. This disease is similar to thalassemia, but during the crisis of sickle cell anemia, massive destruction of red blood cells occurs. Hemolysis will also be quite intense. In childhood, this type of anemia can be triggered by infectious diseases. Anemia is associated with the risk of complications such as: pulmonary edema and infarction, paralysis, cirrhosis of the liver, cardiomegaly. In adulthood, crises are less common, but the likelihood of severe consequences remains.
Ovalocytosis. This hereditary disease is similar to microspherocytosis in terms of the development of symptoms of anemia. However, erythrocytes in ovalocytosis are oval in shape.
Deficiency in G-6-PDH activity is a hereditary disease that is based on a violation of the production of red blood cells. The course of pathology can be very diverse. Sometimes the symptoms of anemia are barely noticeable, and sometimes the disease provokes severe complications. It develops in both infants and adults. The smaller the child, the more severe the disorders of the nervous system will be. Crises most often develop against the background of taking medications, during pregnancy, after or during infectious diseases, when allergens enter the body. If such a crisis is not diagnosed in time, then DIC or acute renal failure may develop, which can be fatal.
Video: lecture on hemolytic anemia:









