Contents
subclinical hypothyroidism (hidden) is the initial stage of the disease, characterized by damage to the functionality of the thyroid gland, but without pronounced clinical symptoms. Thyroid disorders are manifested as a significant increase in thyroid-stimulating hormone (TSH) with normal levels of free T3 and T4. According to statistics, subclinical hypothyroidism occurs in 20% of women over 50 years of age.
Causes of subclinical hypothyroidism
The causes of latent hypothyroidism are the same processes that contribute to the development of classic hypothyroidism:
development of autoimmune thyroiditis;
abnormal development of organs in the prenatal period;
insufficient amount of iodine in the human body;
removed (in whole or in part) thyroid gland (this happens according to indications – cancer of the gland);
long-term use of drugs that depress the work of the thyroid gland (amiodarone, drugs that treat heart problems);
inflammatory processes localized in the organ (subacute inflammation of the gland, postpartum or painless);
irradiation of the neck area (presence of malignant neoplasms);
treatment of the gland with radioactive iodine.
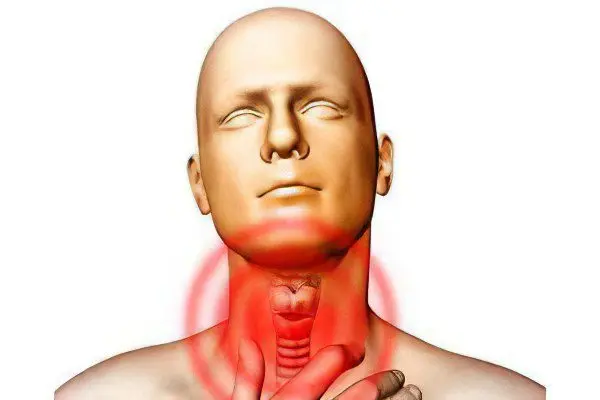
Symptoms of subclinical hypothyroidism

The course of subclinical hypothyroidism is not particularly pronounced, it can simply be overlooked or confused with a general malaise of the body:
constant chills and a feeling of chilliness;
hypothermia;
lethargy, feeling of rapid fatigue, absent-mindedness, drowsiness;
pronounced slowness;
decreased appetite;
galactorrhea;
refusal and unwillingness to perform any work;
decreased libido;
tendency to depression and nervous breakdowns;
reduced concentration;
With the development of the disease, the symptoms become more pronounced:
decrease in intellectual abilities;
weight gain;
memory impairment;
increased intraocular pressure;
violation of the menstrual cycle;
vaginal bleeding;
problems with potency;
dryness, roughness and severe yellowness of the skin;
heartburn, stomach pain;
violation of the chair: constipation, flatulence;
infertility;
miscarriage – premature birth, placental abruption;
severe pain in the muscles;
violation of urine excretion;
hair loss, dryness and brittleness;
swollen eyelids, puffy face;
increased level of endothelial dysfunction;
bradycardia;
hypochromic anemia (decreased hemoglobin in red blood cells).
Diagnosis of the disease

To confirm the diagnosis, it is necessary to conduct a certain number of studies:
a blood test to determine the level of thyroid thyroid hormone: normally, this figure is 2,6-5,7 mmol / l, and, accordingly, 9,0 – 22,0 mmol / l of triiodothyronine and thyroxine. It is impossible to make a correct diagnosis based only on the data of this analysis, since in subclinical hypothyroidism, the level of hormones decreases gradually.
determination of the presence of antibodies to AT-TG (thyroglobulin) and AT-TPO (thyreopercosidase). In a healthy person, these indicators are normally either absent, or their concentration is extremely low: 0-19 U / ml and 0-5,7 U / ml. A significant increase in these antibodies indicates the autoimmune nature of hypothyroidism.
a blood test to determine the level of thyroid-stimulating hormone (TSH) of the pituitary gland: normally, its concentration is 0,5 – 4,3 Med / l. This is one of the most reliable indicators of the development of subclinical hypothyroidism – the pituitary gland is one of the most sensitive parts of the brain that responds to any changes in the human body. In case of malfunction of the thyroid gland, the level of TSH rises sharply, since the production of hormones synthesized by this organ has sharply decreased.
one of the mandatory methods for studying this pathology is scintigraphy, which is based on the use of radioactive isotopes. Using this procedure, you can evaluate the functionality of the thyroid gland, foci of pathological processes or changes in the vascular pattern. With hypothyroidism, the thyroid gland is saturated with iodine much less, which is clearly seen during the study.
In blood tests, anemia can often be detected, the cause of which is complicated hemoglobin synthesis, iron or vitamin B12 deficiency.
To diagnose subclinical hypothyroidism, a number of additional studies are also used:
ultrasound examination (ultrasound) of the thyroid gland – is carried out to study the structure and size of the organ. Changes primarily depend on the cause of the development of the disease. For example, in Hashimoto’s disease, the thyroid gland has a characteristic appearance – “moth-eaten places.”
Ultrasound of the abdominal cavity is performed with pronounced symptoms, which may indicate the neglect of the disease.
X-ray examination of the chest – allows you to assess the degree of development of the skeleton (suspicion of hypothyroidism in children) and the presence of fluid in advanced forms of pathology.
electrocardiography – shows the frequency of a decrease in heart rate and low kink voltage, which is also a significant sign of the development of a serious illness.
Treatment of subclinical hypothyroidism

The treatment of this pathology does not have any specific features, therefore it is based on the use of drugs that regulate the level of thyroid hormones:
hormone therapy includes drugs based on thyroid hormones. This treatment is prescribed and controlled strictly by an endocrinologist, after a complete and thorough examination of the patient.
treatment of the original cause of the development of pathology.
special vitamins and minerals in the treatment of hypothyroidism must be taken every day to maintain the body and stabilize the level of immunity.
normalization of the diet. In any case, with hypothyroidism, the metabolism is significantly disturbed, therefore, in order to avoid complications, it is important to follow simple rules.
It is necessary to exclude:
soy products;
Sugar;
Reduce water intake (up to 500 – 600 ml per day);
Foods with polyunsaturated fats (fatty fish, vegetable and butter, avocados, peanuts).
The diet for hypothyroidism should include:
More fresh fruits;
Meat products (poultry, turkey, beef);
Seafood (to restore the normal functioning of the thyroid gland, iodine is needed, which is found in large quantities in seafood);
Light meat broths;
Natural coffee (natural coffee contains B vitamins and magnesium).
Prognosis of the disease
The sooner the disease is detected, the sooner the recovery period will begin. Advanced forms of hypothyroidism can lead to coma, and more serious disorders of many organs.
Prevention
To date, only those types of hypothyroidism that are associated with iodine deficiency can be prevented, and this is a rare pathology.
In order to avoid intrauterine development of pathology, a pregnant woman must pass all the above tests and, if necessary, start treatment on time.









