Contents

Stress urinary incontinence is a common problem for many women that is not usually talked about out loud. However, it can significantly impair the quality of life. Women with this pathology experience physical and psychological discomfort, however, for a number of reasons, they do not go to the doctor. It has been established that about 40% of women in Europe suffer from stress urinary incontinence. It is simultaneously a urological, gynecological and neurological problem. Moreover, she begins to disturb women even at reproductive age, and by the age of 70, every second representative of the weaker sex will suffer from urinary incontinence.
In Russia, the problem of stress urinary incontinence is also of enormous proportions. According to the chief urologist of the Ministry of Health of the Russian Federation, more than 40% of women over the age of forty suffer from it in the country. Although this problem has existed since ancient times, until the middle of the last century, medicine did not consider it as a disease. Therefore, most women still consider stress urinary incontinence to be a natural process of aging of the body and do not take any measures to combat it. However, this approach is fundamentally wrong.
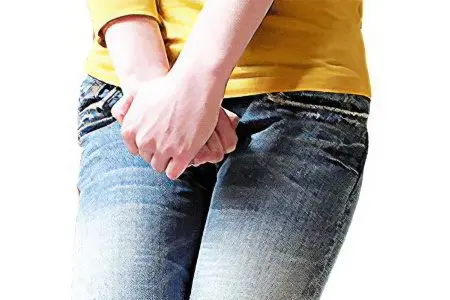
So, stress urinary incontinence is an involuntary release of urine, which may be associated with the failure of the function of the urethral sphincter, or with the weakness of the muscles of the pelvic floor. As a result, urine flows out even with a slight tension of the peritoneum: with laughter, with coughing, sneezing, sexual intercourse, a sharp rise from a place and physical exertion. The word “stress” in this case is used in the context of “effort, load”.
Causes of stress urinary incontinence
In more than 60% of cases, stress urinary incontinence is associated with weakened sphincter function. This can occur after a difficult birth, or after a gynecological operation. Moreover, it is not the number of births that matters, but their course. In this regard, the birth of a large child, the narrow pelvis of a woman, ruptures of the pelvic floor muscles, the use of obstetric forceps, episiotomy, etc., represent a danger. After childbirth, the restoration of tissues and ligaments can take place independently, but it will not be complete. As for operations, interventions such as hysterectomy, oophorectomy, etc. can affect.
In 15% of cases, violations occur due to severe physical exertion. That is, the woman was engaged in hard physical labor, which led to a weakening of the pelvic floor muscles and changed the position of the internal organs.
In 7% of cases, stress incontinence is due to hormonal disorders in the body that occur against the background of menopause. Age-related estrogen deficiency affects, leading to atrophic changes. This is especially noticeable in the condition of the skin, which becomes dry and flabby. Not only the skin becomes decrepit, but also the ligaments that are responsible for holding urine in the bladder.
Prerequisites for the development of stress incontinence can be factors such as: obesity, frequent constipation, radiation therapy.
The risk of stress urinary incontinence is increased in women who suffer from chronic cystitis or urethritis.
Do not overlook diseases such as COPD and bronchial asthma in the pathogenesis of stress urinary incontinence. These pathologies are characterized by frequent episodes of increased intra-abdominal pressure, which over time causes overstretching of the ligamentous apparatus around the urethra.
So, it is wrong to consider stress urinary incontinence solely as a consequence of aging.
Symptoms of stress urinary incontinence

The main symptom of stress urinary incontinence is the involuntary leakage of urine that occurs without any urge to empty the bladder. There is incontinence due to physical stress.
If urine leakage is ignored, then the pathology will progress. The amount of urine lost increases from a few drops to the full volume of the bladder.
Three degrees of stress urinary incontinence should be distinguished, each of which is characterized by the following symptoms:
Easy degree. The output of urine occurs when sneezing, coughing, physical effort. If a woman does not cough or laugh, then urine does not leak. At first, it is released only when the bladder is sufficiently full.
Average degree. Urine begins to leak during a sharp rise from a place, while running.
Severe degree. Urine leaves the bladder even when walking and at rest.
Urologists use a classification based on the number of pads a woman uses per day. First degree – one pad per day, second degree – from two to four pads per day, third degree – more than four pads per day.
Diagnosis of stress urinary incontinence

The diagnosis of urinary incontinence should be started by filling out a diary, which must be kept for several days. A woman needs to record the amount of fluid she drinks, the number of urination and portions of urine shed in milliliters, as well as the frequency of episodes of incontinence. It is important to note what exactly the woman was doing at the moment when the involuntary release of urine occurred.
Each patient with urinary incontinence should visit a gynecologist who will assess the condition of the tissues and muscles, determine the possible prolapse of the walls of the vagina and uterus. A cough test is also performed in the gynecologist’s office. A woman with a full bladder should cough several times. If at this time there is leakage of urine, then the test is considered positive. Based on these examinations, a diagnosis is made.
In some cases, it may be necessary to implement the following diagnostic procedures, such as:
Ultrasound of the pelvic organs;
Cystoscopy;
ureteroscopy;
Uroflowmetry.
The doctor simultaneously assesses the condition of the skin of the perineum, reveals the presence of genitourinary fistulas. As for laboratory methods of examination, urine culture, general urinalysis, smear microscopy are shown.
Treatment of stress urinary incontinence

Treatment of stress urinary incontinence in the early stages is absolutely not difficult. If a woman seeks medical help in a timely manner, then surgery can be avoided and conservative methods of therapy can be dispensed with.
If the disease has only recently manifested itself, then the doctor will select the woman exercises that are aimed at strengthening the muscles of the pelvic floor. As a rule, this is possible at stages 1-2 of the development of incontinence. Well proven Kegel exercises, which are reduced to alternate tension and relaxation of the muscles of the pelvic floor.
It is possible to use special devices that are inserted into the vagina and stimulate it from the inside with electrical impulses.
Another progressive non-surgical treatment for stress incontinence is BFB (biofeedback) therapy. This method resembles a computer game, when a woman, looking at the monitor, learns to control the muscles of the pelvic floor. She alternately strains and relaxes the muscles of the perineum. Sensors are connected to her body at this time, which detect muscle contractions and display them on the screen in the form of a floating fish. If you combine biofeedback therapy with other exercises, you can achieve good results: normalize the functioning of the bladder, sphincters, improve blood circulation in the pelvic organs, get rid of stressful urine leakage.
You can also train the muscles of the pelvic floor with the help of special cone weights that are placed in the vagina and held by the strength of its muscles. As you train, the weight of the weights increases, which leads to the development of self-control skills during urination. As a rule, the effect can be felt already after 1-1,5 months after the start of such classes.
It is equally important to normalize weight, quit smoking, which provokes a cough. It is important to exclude such a factor as hard work.
As for drug correction, it is possible to prescribe antidepressants, estrogen and systemic HRT. When incontinence develops against the background of menopause, hormonal preparations have proven themselves quite well.
In the later stages of the development of urinary incontinence, the choice of therapeutic tactics depends on what exactly caused the pathological condition.
In some cases, it is not possible to do without surgical intervention. To date, incontinence can be dealt with using a synthetic prolene loop (sling operation). The loop is inserted into the body and placed under the middle part of the urethra, pulling it in the right way. The loop is adjusted by the surgeon, after which it is fixed and left in the woman’s body. It is possible to perform the operation under local anesthesia. Recurrent stress urinary incontinence in women develops in 10-20% of cases.
Another modern technique for treating incontinence is the introduction of hydrogels into the sphincter area. They support weakened muscles by providing a locking effect. However, this method has a number of disadvantages, including: a low degree of biocompatibility of drugs, their rapid resorption and migration in tissues. In this regard, it is preferable to inject an artificial polymer, the use of which can be considered as safe as possible.
Depending on the indications, operations such as anterior colporrhaphy, implantation of an artificial sphincter, urethrocystopexy, etc. can be applied. In general, there are more than 200 methods of operations for urinary incontinence. Many of them have long been abandoned, as they are very traumatic, such as the Goebel-Steckel operation, while others are not effective enough, such as anterior colporrhaphy.
Prevention of urinary incontinence

It is necessary to give up bad habits.
Maintain a normal body weight.
It is important to strengthen the muscles of the pelvic floor, to control the timely emptying of the intestines.
Neurological and urogenital diseases should be treated in a timely manner.
When urinary incontinence is detected, women should put aside false shame and address their problem to the doctor. The sooner treatment is started, the better the results will be. When qualified assistance is provided in the early stages of the development of the pathological process, it is almost always possible to avoid surgical intervention.









