Contents
In the structure of oncological diseases, this is one of the most common pathologies. Lung cancer is based on malignant degeneration of the epithelium of the lung tissue and impaired air exchange. Malignant cells are also called poorly differentiated (on the topic: poorly differentiated lung cancer). The disease is characterized by high mortality. The main risk group is smoking men aged 50-80 years. A feature of modern pathogenesis is a decrease in the age of primary diagnosis and an increase in the likelihood of lung cancer in women. (on the topic: benign lung cancer)
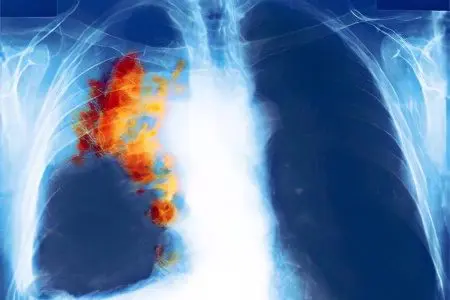
lung cancer statistics
Statistics on the incidence of lung cancer is contradictory and scattered. However, the influence of certain substances on the development of the disease has been unambiguously established. The World Health Organization (WHO) reports that the main cause of lung cancer is tobacco smoking, which provokes up to 80% of all reported cases of this type of cancer. In Russia, about 60 thousand citizens fall ill every year.
According to some researchers, the structure of the incidence of various forms of this pathology, depending on age, is as follows:
up to 45 – 10% of all cases;
from 46 to 60 years – 52% of cases;
from 61 to 75 years -38% of cases.
Until recently, lung cancer was considered a predominantly male disease. Currently, there is an increase in the incidence of women and a decrease in the age of initial detection of the disease. Researchers attribute this phenomenon to an increase in the number of women who smoke (up to 10%) and people working in hazardous industries.
Number of sick women from 2003 to 2014 increased by about 5-10%.
Currently, the gender ratio of lung cancer incidence is:
in the group up to 45 years – four men to one woman;
from 46 to 60 years – eight to one;
from 61 to 75 years – five to one.
Thus, in groups under 45 and after 60 years there is a significant increase in patients of the weaker sex.
How long do people live with lung cancer?

The disease is characterized by high mortality. This feature is associated with the importance of the respiratory function for the body.
Life can continue with the destruction of the brain, liver, kidneys, any other organs until the respiratory or heart stops. In accordance with the canons of modern pathophysiology, biological death is a stoppage of breathing or heartbeat.
At a certain stage of carcinogenesis, the patient has a rapid extinction of vital functions with a decrease in the respiratory activity of the lungs. It is impossible to compensate for lung function with artificial devices, the process of air exchange (atmospheric air – lungs – blood) is unique.
There are statistical data on the likelihood of a five-year survival rate for people at different stages of lung cancer. It is clear that patients who receive treatment in the early stages of cancer are more likely to save their lives. However, without complete information about the features of pathogenesis, it is not ethical to give an individual prognosis.
Meanwhile, the survival rate of patients is statistically significantly higher with different localizations of the focus on the periphery or in the center of the lung, where the main airways are concentrated, there are many large vessels and there are nerve nodes.
High odds long-term survival in peripheral lung disease. Cases of life expectancy of more than ten years from the moment of diagnosis are known. The peculiarity of carcinogenesis of the peripheral form of cancer is a slow course and a long absence of pain response. Patients even of the fourth stage have relatively good physiological conditions and do not feel pain. Only in the critical period does fatigue increase, weight decrease, pain syndrome develops after metastasis to vital organs.
Low odds with central cancer. Life expectancy from the moment of diagnosis does not exceed 3-4 years. Active carcinogenesis lasts an average of 9-12 months. The tumor is characterized by aggressiveness, especially in the last stages, when any modern treatment is ineffective, it is characterized by the development of pain syndrome in case of damage to the central bronchi and metastasis to neighboring organs.
It is clear that the above is conditional information. Cancer is always an unpredictable disease, accompanied by an explosive growth of cells, or a reverse process and inhibition of carcinogenesis (on the topic: lung cancer in children).
In addition, the aggressiveness of cancer depends on the microscopic (histological) structure of the cells, for example, small-celled or non-small-celled (according to the shape of the tumor cells).
Doctors are less likely to prolong the life of patients with small cell cancer, including those after radical surgery and recurrence of carcinogenesis.
Symptoms of lung cancer

Lung cancer, especially its peripheral forms, is difficult to diagnose in the early stages of carcinogenesis.
The causes of diagnostic errors are due to:
a similar density of normal cells and malignant tumors, the disguise of affected cells as healthy ones – all this complicates the diagnosis, including imaging methods;
the location of the focus under the bone tissue of the chest;
the absence of regional lymph nodes located close to the surface of the skin and most rapidly responding to pathogenesis;
weak pain sensitivity of peripheral areas of the lungs that do not have pain receptors;
a high level of compensatory protection, respectively, a long-term absence of dangerous clinical symptoms that confuse diagnosticians with similarities with diseases that can be treated with medication rather than surgical treatment.
Diagnostic steps for determining the symptoms of lung cancer and its types include the accumulation or synthesis of clinical, morphological, histological information about the disease and their subsequent analysis.
Thus, the diagnosis of any disease, including this one, includes two areas of research (synthesis and analysis) and three stages of diagnosis (primary signs, general symptoms, differential symptoms):
primary signs of the disease. Feelings of the patient in the form of hemoptysis, cough, fatigue, progressive emaciation, bad breath and other signs with which a person who feels sick consults a doctor for advice and determines the causes of malaise.
General symptoms. Determination of the localization of pathogenesis (in the central, peripheral, apical part of the lung). Installed:
physical methods (inspection, palpation, percussion or tapping in order to determine zones of altered sound, auscultation or listening to changes in respiratory sounds);
imaging methods, including ionizing ones – X-ray, CT and modifications, radioisotope, PET, PET-CT; non-ionizing – ultrasound, MRI and modifications;
laboratory methods (general clinical, specific, including tumor markers).
differential symptoms. Needed by oncologists to clarify changes at the cellular and microphysiological levels, for example, to determine non-small cell and small cell forms of cancer or their varieties. They are determined by cytological and histological methods in various modifications, sometimes supplemented by instrumental visualization methods, PET and PET-CT methods are the most informative here.
In modern oncology, screening examinations are the most promising method for early diagnosis. This is a large-scale medical examination of a conditionally healthy population. Screening for some forms of cancer effectively replaces the classic three-step method of diagnosis. Unfortunately, screening studies to determine lung cancer in our country are not carried out due to the low efficiency of instrumental detection of the disease.
For the widespread introduction of screening, it is necessary:
availability of effective highly sensitive diagnostic devices;
highly qualified medical staff;
oncological alertness of the population.
If the first two conditions have recently been more or less successfully fulfilled by the state, then our article calls for an increase in oncological alertness and a sense of responsibility for one’s own health.
We do not at all strive to make everyone who reads an oncologist. Our task is to optimize the cooperation between the patient and the doctor. After all, every ninth out of ten patients with lung cancer gets to the doctor of the district clinic.
Cough with lung cancer
Cough is a protective reaction of the respiratory organs to irritation of specific receptors. It occurs with a short-term or long-term endogenous (internal) or exogenous (external, extraneous) effect on receptors.
During the initial appointment, try to accurately describe the cough reflex, if any. Although cough is not a pathognomonic symptom of lung cancer, sometimes it indicates the nature of the pathogenesis. The combination of research methods – cough, percussion and radiography can provide the doctor with valuable material for analysis during the initial diagnosis.
Pathological (long-lasting) cough sounds are characterized as:
strong/weak;
frequent/rare;
loud/hoarse (hoarse);
long/short;
rolling / jerky;
painful/painless;
dry/wet.
The following cough sounds are not typical for lung damage: strong, loud, short. They are most likely to characterize lesions of the larynx and trachea, or oncology in these areas. Cough with irritation of receptors localized on the vocal cords is manifested by a hoarse or hoarse sound.
Characteristic cough sounds when receptors in the lung tissue are irritated:
Weak, lingering, deaf, deep – characterizes a decrease in the elasticity of the lung or pathological processes scattered in the tissues.
Painful, turning into a sparing form – coughing, indicates the involvement of the pleura around the lung in the pathogenesis, or the localization of pathogenesis in the large bronchi of the central zone, which are sensitive to pain. The pain is aggravated by movement of the chest. If during auscultation (listening) of the lung a combination of painful cough and splashing noise is detected, this means the accumulation of fluid between the lung and the pleura.
Moist cough:
with a good (liquid) expectoration of the contents – an acute course of pathogenesis in the lungs.
with a viscous discharge – a chronic course of pathogenesis in the lungs.
A dry cough may precede the development of a wet one, or a wet one may turn into a dry cough. The phenomenon of dry cough is characteristic of chronic irritation of receptors without the formation of exudate in the lung. It may also be with a growing neoplasm without inflammatory and necrotic processes around the focus.
A dangerously abrupt cessation of coughing is one of the possible signs of suppression of the reflex due to the development of intoxication.
We remind you that you should not draw independent conclusions. The information is given so that the patient can most fully describe his own feelings to the doctor in the presence of a cough reflex. The final diagnosis is made on the basis of a complex of studies.
Blood in lung cancer

Patients are always afraid of the release of blood from the respiratory tract. This phenomenon is called hemoptysis. It doesn’t have to be a sign of lung cancer. Blood secreted from the lungs is not a specific symptom of lung cancer.
The discharge of blood from the nose is a manifestation of a violation of the integrity of one of the blood vessels in the respiratory tract. The discharge of blood from the oral cavity causes confusion among non-professionals.
Isolation of blood from:
digestive organs – dark blood (the color of coffee grounds) due to the action of digestive enzymes or gastric juice;
respiratory organs – blood is predominantly scarlet in color, sometimes dark red, always foamy due to the admixture of air.
The causes of pulmonary hemoptysis are diverse and accompany diseases with pathogenesis in the human respiratory system. Among them:
late stages of tuberculosis;
internal bleeding from chest wounds;
abscesses in the lung or airways;
heart attacks;
pneumonia.
There may be other reasons as well. Bleeding in lung cancer usually means damage to one of the vessels in the mediastinum or the central part of the lung. Hemoptysis is a dangerous symptom, especially with massive internal blood loss.
Signs of massive bleeding:
copious discharge of a scarlet color, slow bleeding of a dark red color;
progressive deterioration of well-being;
pallor of mucous membranes;
thready pulse.
The first signs of lung cancer
They may differ significantly from the usual signs, such as coughing, shortness of breath, hemoptysis and other symptoms characteristic of lung cancer.
A person who can be diagnosed with lung cancer, at the initial appointment, receives a referral to doctors of the following specialties:
a neurologist, if the patient has cluster (paroxysmal) headaches and pains resembling attacks of osteochondrosis;
an ophthalmologist or neurologist, in case of violation of the mobility and size of the pupil of the eye or a change in the pigmentation of the iris of the eye;
to the therapist, if you suspect a cold with a dry cough, possibly a slight hyperthermia (high body temperature);
a therapist or a phthisiatrician, with a wet cough, wheezing in the lungs, hemoptysis, a sharp decrease in body weight, general weakness;
cardiologist, with shortness of breath, pain in the region of the heart after a slight physical exertion, general weakness.
A person noticing the above symptoms should report them to the doctor or supplement the information he collects with the following information:
attitudes towards smoking with pulmonary symptoms;
the presence of cancer in blood relatives;
a gradual increase in one of the above symptoms (it is a valuable addition, as it indicates the slow development of the disease, characteristic of oncology);
an acute increase in symptoms against a background of chronic previous malaise, general weakness, loss of appetite and body weight is also a variant of carcinogenesis.
Causes of lung cancer

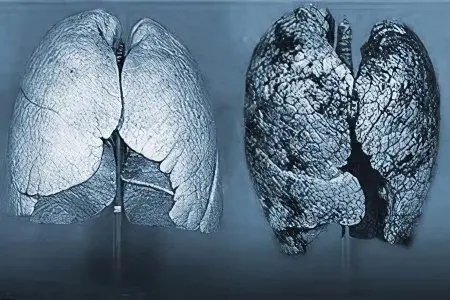
The lungs are the only internal human organ in direct contact with the external environment. The inhaled air reaches the alveoli unchanged. Microparticles present in the air linger on the walls of the mucous membranes. Constant contact with the external environment predetermines the main feature of the lung epithelium – an increased rate of renewal of generations of cells of the mucous membranes of the bronchi.
The functions of the biological filter are carried out by the mucous membranes through:
microvilli lining the airways;
mucus-producing epithelium;
cough reflex receptors.
Epithelial cells come into contact with aerosols of inhaled air, consisting of liquid and / or solid particles, including:
natural – dust, pollen of plants;
anthropogenic – tobacco smoke, car exhaust, dust from factories, mines, mines, thermal power plants.
In order for the reader to understand what is at stake, an aerosol is a stable suspension in a gas (air):
ultra-small liquid particles – fog;
ultra-small solid particles – smoke;
small solid particles – dust.
The composition of fog, smoke and dust may include aggressive inorganic and organic substances, including plant pollen, microscopic fungi, bacteria, viruses that adversely affect the microvilli of the epithelium.
Weakly protected epithelial cells are under the influence of external pathogenic factors every second, which greatly increases the likelihood of pathological mutations and the development of neoplasms in the lungs.
Potential risk factors for lung cancer:
High rate of epithelial apoptosis – the more new cells are formed, the higher the likelihood of cancerous mutations (natural factor);
Relative vulnerability of delicate tissue from the effects of harmful aerosols of inhaled air (provocative factor).
It has been noted that the likelihood of developing lung cancer is directly related to the aging of the body, genetic prerequisites and chronic lung diseases.
risk factors for lung cancer
Predominantly affected people are long-term under the influence of physical, chemical and biological factors, as well as having a hereditary predisposition.
Tobacco smoke. Approximately 80% of lung cancer patients are active smokers, but the harmful effects of secondhand smoke are also seen (Facts and consequences of smoking during pregnancy).
Radon (weakly radioactive element). The alpha radiation of radon is included in the natural radiation background of the earth. The radiation power is low, however, sufficient to stimulate mutations in the cells of the respiratory tract. Radon in the form of gas accumulates in the basements of houses, penetrates into living quarters through the ventilation system, through the gaps between the basement and the first floor.
Genetic predisposition. The presence of repeated cases of lung cancer in blood relatives.
Age. Physiological aging significantly increases the risk of developing pathological mutations in epithelial cells.
professional risks. High likelihood of workplace exposure to volatile, dusty carcinogens:
asbestos – used in construction in the production of building materials, rubber products, is part of drilling fluids;
cadmium – as part of solders it is used by jewelers, when soldering electronic circuit boards, anti-corrosion treatment, in the production of batteries and solar panels;
chromium – used in metallurgy as a component of alloyed steels;
arsenic – used in metallurgy, pyrotechnics, microelectronics, paints, leather industry;
pairs of synthetic dyes based on nitro enamel – used in construction, painting;
exhaust fumes – auto repair workers suffer;
ionizing (gamma, beta, x-ray) radiation – received by employees of x-ray rooms and nuclear power plants.
Endogenous factors, including chronic pulmonary diseases (tuberculosis, bronchopneumonia);
unclear factors. In a certain number of patients it is impossible to establish the causes of the disease with modern methods.
Classification of lung cancer
Without prior preparation, it is very difficult to understand the types and differences between the forms of lung cancer. In practical medicine, complex terms are used to denote them. There are many types and forms of cancer. We have simplified the task as much as possible and made the differences clear. All terms used to refer to forms of cancer fit into our simplified, adapted classification.
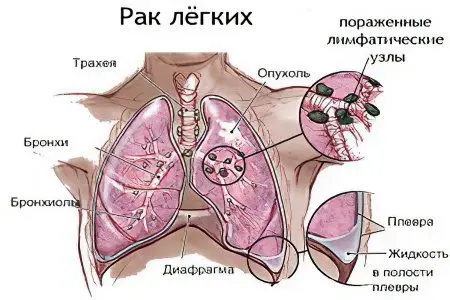
Classification according to the location of the primary focus. A cancerous tumor can be localized in different parts of the lung:
Central cancer – located in the center of the lung, where large bronchi, vessels and nerve nodes are localized;
Peripheral cancer – located on the sides of the lung, where small bronchioles, small blood vessels – capillaries, few pain receptors are localized;
Apical cancer (mediastinal lung cancer) – located at the top of the lung, this is a type of peripheral cancer. It is characterized by distracting symptoms due to the involvement of the blood vessels of the clavicle and stellate ganglion. Pankosta is manifested by neurological symptoms: on the face (asymmetry), in the pupils (different shape, omission, constriction, others), in the head (severe cluster headache). This confuses diagnosticians with the multiplicity of manifestations and the lack of x-ray visualization of tumor foci.
atypical localization. Involvement in carcinogenesis of the anterior and / or upper half of the mediastinum – the organs of the center of the chest, lying between the right and left lungs.
When describing the localization of cancer, the radiologist usually makes an addition, indicating the shape of the tumor, for example:
nodular;
branched;
nodular-branched or others.
Thus, according to the localization of the tumor in the body, cancer can be: central, apical, peripheral, as well as right-sided, left-sided or bilateral. According to the form of tumor growth – nodular, branched or mixed.
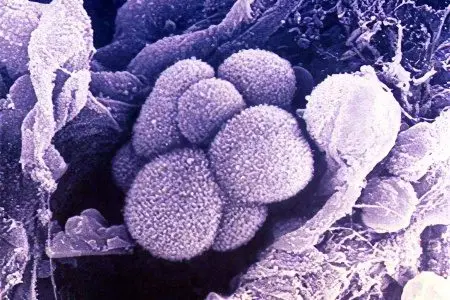
The above classification does not take into account the microscopic structure of tumor cells. For differentiation, a histological analysis is used, which is necessary to clarify the features of the microscopic structure of the neoplasm.
It is well known that the microscopic features of the structure of the oncocell determine the pathogenesis of the disease, including:
tumor growth rate;
predominant localization of the primary focus;
aggressiveness – a tendency to metastasize.
Knowledge is used by clinicians to guide treatment strategies. In our case, this is necessary for a general idea of carcinogenesis.
Classification based on histological cell differences:
Non-small cell cancer. This is a group of oncological diseases, consisting of several closely related forms. The total proportion of non-small cell forms in the structure of lung cancer is about 80-85%. The association is based on the morphological similarity of cells, however, each form has some features. Non-small cell cancer combines the forms:
squamous;
large cell;
adenocarcinoma;
rare forms.
Small cell cancer. more homogeneous group. Includes about 10-15% of clinical cases of lung cancer. It is particularly aggressive. The doubling rate of the tumor volume of this form is about 30 days versus more than 100 days for non-small cell forms.
We have given a generalized classification of lung cancer. There are subtler varieties of cancer, but they are used in scientific discussions to describe carcinogenesis. Read more about common forms below.
Stages of lung cancer
In oncology, for convenience of description, the stages of the disease are distinguished. The staging of carcinogenesis is a conditional concept, but it is very convenient, and allows you to standardize and simplify the description of the disease in professional communication.
In accordance with the international classification, the state of carcinogenesis is usually denoted by the first letters of Latin words:
Tumor (tumor), denotes a tumor, for the purpose of reduction, the first letter of the word is used – T, supplemented by numbers from one to four to characterize the size of the tumor.
Node (node), denotes regional lymph nodes, for the purpose of reduction, the first letter of the word is used – N, which is supplemented by numbers from one to three to indicate the degree of involvement of the nodes.
Metastasis (metastasis), means the presence of outgrowths of a malignant tumor in distant organs, for the purpose of reduction, the first letter is used – M, which is supplemented by the numbers zero or one and characterizes the degree of growth.
Uses an additional designation of the aggressiveness of cancer cells by writing the letter G. Designate G1 highly differentiated (non-aggressive cells). Further, in order of increasing aggressiveness to the human body – G2, G3, G4.
Similarly, the absence of visible changes in the body and precancerous conditions are indicated with the addition of symbols:
There is not enough information to describe the condition of the tumor – letter (x)
The tumor is not determined – the letter (0)
Non-invasive cancer – a combination of the letters (is) or (carcinoma in situ).
Using similar notation, we present a description of the stages of lung cancer.
stage 1 lung cancer
Т1 – the size of the neoplasm does not exceed three centimeters in diameter (on an x-ray). N0 – Lymph nodes are not affected. Metastases – M0 are absent.
Unlike breast cancer – breast cancer (see here), the first stage of lung cancer (LC) is difficult to diagnose.
For example, lymph nodes in:
Breast cancer – freely palpable by hand, starting from the earliest stages of carcinogenesis;
RL – visible only on x-rays or other sophisticated imaging methods, since the lymph nodes (peribronchial or lung roots) are located deep in the chest.
stage 2 lung cancer
Т2 – the size of the neoplasm is from 3 to 6 centimeters in diameter. This group also includes tumors of any other size sufficient to block the bronchus, which is detected on the radiograph in the form of focal atelectasis (fall) or pneumonia (seal) of the lung tissue on the periphery of the bronchus. The tumor and pathological foci of small size can be seen on the radiograph in the central region, much more difficult – on the periphery and the apex of the lung.
Involvement in carcinogenesis of regional lymph nodes of the second stage – N1. This means a unilateral lesion of cancer cells of the lymph nodes. M0 or M1 – means that metastases are equally likely to be absent and found in neighboring organs.
stage 3 lung cancer
Т3 – the size of the neoplasm is more than 6 centimeters in diameter. The tumor can also be of any other size, but it extends to the chest wall and the division of the main bronchi, the diaphragm, or it is a tumor that causes atelectasis or hardening of the entire lung. N2 – involvement in carcinogenesis of distant lymph nodes on the side of the lesion or in the area of bifurcation of the main bronchi. M1 – there are signs of metastasis in organs distant from the lungs.
stage 4 lung cancer
Т4 – the size of the neoplasm does not matter. The tumor spreads beyond the chest, primarily affects neighboring organs (heart, digestive tract, thoracic vertebrae), and is characterized by accumulation of exudate in the pleural cavity. N3 – total lesion of the lymph nodes of the diseased side, multiple lesions on the opposite side. M1– Multiple distant metastases.
Types of lung cancer
Lung cancer is distinguished by the place of localization (peripheral or central), as well as by the cytological, histological structure of oncocells (small cell, non-small cell).
Peripheral lung cancer
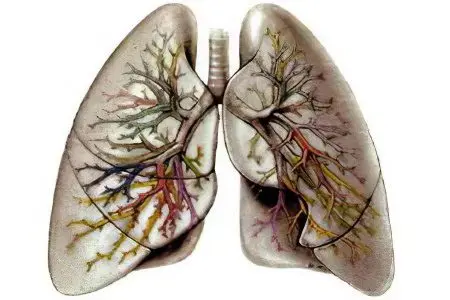
The peculiarity of this type of cancer is that the tumor develops as a result of mutations on the surface of small bronchi – subsegmental (3-5 orders) and small (6-16 orders).
To make it clear: the bronchial tree of the lung consists of bronchi in decreasing order of diameter from the 1st main bronchus to the bronchi of the 16th order. Small, 16th order, pass into even smaller bronchioles and into the final structures – alveoli.
The clinical significance of lesions of the small and smallest bronchi:
prolonged absence of symptoms (no pain receptors, better compensation for damage in small lung formations);
the first symptoms (cough, hemoptysis, pain of uncertain localization) are associated with trauma to the delicate bronchi and small capillaries.
The most characteristic growth of peripheral tumors is nodular. In this form, it is usually found on fluorography (radiography) pictures taken for acute or chronic lung diseases.
Characteristic forms of peripheral cancer, visualized in the pictures in the form of:
rounded (solitary) node;
rounded hollow node with thin walls;
blurred infiltrate;
single node less than 10 mm;
multiple small knots.
The rhythm of growth (doubling the value) is 110-140 days. Fluctuations from the norm within a minimum of 40 days, a maximum of 800 days were established. To some extent, a long doubling period indicates a benign neoplasm.
Radiation of contours is characteristic of a peripheral tumor. This phenomenon is explained by a special form of growth of nodes in the lung.
In some cases, an approximate differentiation of tumors according to the shape of contours and rays is possible:
small, frequent rays along the contour – squamous formation;
thick, long rays, calcareous punctate inclusions – Glandular cancer;
clear contours – aggressive small cell formations.
Other indirect signs of peripheral cancer, found on the pictures in the form of a negative light area:
“Rigler” deepenings are visible in the area of connection or detachment of the tumor and bronchus of the 3rd-5th order;
around the tumor of the lung tissue, a section of a small vessel clogged with a tumor;
Complications of peripheral cancer:
pneumonia behind the blockage of the bronchus and the exclusion of this area from the respiratory function. Extensive foci lead to a decrease in respiratory activity of the lung;
the formation of a cavity in the node, which may later be the focus of the spread of purulent inflammation;
accumulation of fluid in the cavity between the lung and the pleura;
the rapid growth of the peripheral node and the transition of the process to the mediastinum;
The difficult-to-diagnose forms of peripheral cancer include apical lung cancer, which is characterized by neurological symptoms due to the spread of damage to important nerve nodes located in this zone.
Small cell lung cancer
It got its name because of the shape of the cells, it is also called neuroendocrine lung cancer. It is one of the most aggressive forms of lung cancer. It occurs mainly in male smokers over the age of 40. The detection rate of this disease is no more than 25% of all histological types of cancer.
Biological characteristics of small cell carcinoma:
small size (only twice as large as a lymphocyte – blood cells);
malignancy;
rapid growth, active doubling of volume within 30 days, for comparison, in other forms of cancer – more than 100 days;
sensitivity of cancer cell receptors to chemotherapy and radiation therapy.
There are several types of small cell carcinoma:
oat cell;
intermediate;
combined.
Small cell neoplasms are capable of producing some hormones (ACTH, antidiuretic, somatotropic).
The clinical symptoms of small cell carcinoma do not differ fundamentally from other forms of lung cancer, except that the pathogenesis develops rapidly, and the manifestations visible to the researcher are scarce.
Non-small cell lung cancer
This group of oncological diseases differs from small cell forms in histological features. Clinically manifested:
increased fatigue;
pulmonary syndrome (shortness of breath, cough, hemoptysis);
progressive weight loss.
Includes about 80% of all patients with malignant diseases.
There are three main histological forms of non-small cell cancer:
squamous;
large cell;
adenocarcinoma.
The disease is characterized by a subclinical course of pathogenesis up to stage 2-3. For example, about 30% of patients recognize their diagnosis at stage 3, about 40% at stage 4.
The disease is characterized by a rapid course of the last stages. Within five years, only 15-17% of patients remain alive.
Squamous cell lung cancer
It is a smaller histological variety of non-small cell carcinoma. Differs in quiet cell growth. Mutations begin either in the central part or on the periphery of the lung.
Squamous cell carcinoma is the result of the degeneration of the ciliated epithelium under the influence of nicotine and other substances contained in tobacco smoke into a cell shape resembling an integumentary squamous epithelium.
A growing tumor sprouts with capillaries of blood vessels to ensure its own vital activity.
Clinical symptoms are similar to other forms of lung cancer. They become noticeable for diagnosis after involvement in the pathogenesis of a significant part of the lung tissue and metastasis to regional lymph nodes.
The main diagnostic method is a histological examination of a sample of cancer cells.
Central lung cancer
Refers to forms of cancer, determined by the location in the lungs. The peculiarity of the localization of the tumor in the large bronchi 1-3 orders.
It is characterized by the early onset of symptoms when:
involvement in carcinogenesis of large bronchi and mediastinal organs;
stimulation of pain receptors;
blockage of large bronchi and loss of a significant volume of the respiratory surface.
This type of oncology is relatively easy (with the exception of the earliest stages) to be visualized by conventional diagnostic methods, confirmed by laboratory and clinical symptoms.
The most typical early symptoms are:
untreated dry debilitating cough;
accession to the cough of blood as a result of a violation of the integrity of the blood vessel, and then the appearance of mucous, purulent sputum;
blockage and compression of a large bronchus is accompanied by shortness of breath at rest.
Metastases in lung cancer
Almost all human cancers are capable of metastasis – the movement of oncocells throughout the body and the formation of foci of distant secondary carcinogenesis.
General patterns of metastases in lung cancer:
distribution throughout the body with the flow of biological fluids (lymph, blood) and upon contact with neighboring organs;
cells of metastases are almost always identical to the cells of the primary focus,
mechanical movement of cancer cells to other organs does not mean the development of secondary carcinogenesis, inhibition of this process is observed.
The spread of the tumor in lung cancer occurs in three ways – lymphogenous, hematogenous and contact.
Lymphogenic movement of cells is characterized by the most likely places of fixation of malignant cells in the lymph nodes of the lung:
pulmonary;
bronchopulmonary;
tracheobronchial and tracheal;
prepericardial;
lateral pericardial;
mediastinal.
The hematogenous movement of cells is characterized by the most probable places of fixation of malignant cells in the organs of the mediastinum:
heart and its vessels;
trachea and main bronchi of the lung;
esophagus;
thymus;
nerve nodes (phrenic, vagus, stellate).
Metastases further move along the venous route to the following organs, in descending order of importance:
liver;
kidney;
bones skeleton;
adrenal glands.
The contact path explains the spread of carcinogenesis to neighboring formations that do not have a connection with the lung blood and lymphatic vessels, in particular to the pulmonary pleura.
Prognosis of the disease
Above, we talked about a significant increase in a favorable outcome when cancer is detected at an early stage of oncogenesis. The problem is that this form of cancer is difficult to diagnose in its early stages.
The use of traditional diagnostic algorithms makes it possible to detect lung cancer in 60-80% of cases at stages 3-4 of the disease, when surgical treatment is ineffective, and metastases spread far beyond the respiratory organs.
It is possible to significantly improve the prognosis of the disease by using modern diagnostic technologies.
Pay attention to the correspondence between the costs of diagnosing a disease and the quality of subsequent treatment.
Costs of high-tech cancer detection methods:
justified in the early stages of the disease, when the doctor has a large choice of treatment options;
are not justified or doubtful, when carcinogenesis has developed to a clinically detectable stage of the disease, in this case, conventional diagnostic studies can be limited.
The most promising methods for early detection of tumor cells in the lung:
Multilayer spiral computed tomography (MSCT). The technique allows you to examine the breast in 8-10 seconds, or to examine the entire person to determine the foci of primary and secondary tumors. Other methods do not have this capability. At the same time, tumors up to 1-3 mm in diameter are detected with high clarity. It is possible to build two and three-dimensional images and determine the exact localization of the tumor.
Positron emission tomography combined with computed tomography (PET-CT), the method is significantly superior to CT or MRI methods in determining the sensitivity and specific features of tumor cells.
If the sensitivity and specificity of CT or MRI is on average 60%, then the similar indicators of PET-CT are from 90% and higher, and the minimum size of a detected tumor is 5-7 mm.
Diagnosis of lung cancer

The diagnosis has a multi-stage complex professional algorithm that is understandable only to specialists. In this section, we summarize the information described above that is important to the patient.
A set of symptoms for diagnosing lung cancer:
pulmonary;
extrapulmonary;
hormonal.
We have previously mentioned the first two directions and mentioned in passing that some tumors secrete hormones and hormone-like substances that change the clinical symptoms of the disease.
For the initial diagnosis, the presence of at least one symptom in each syndrome is important.
Pulmonary syndrome
Includes long-term, untreatable:
wet cough, possibly with blood;
pain in the chest;
shortness of breath at rest, worse after exercise;
wheezing;
hoarseness.
Extrapulmonary syndrome
Characteristic for lung cancer only in combination with pulmonary syndrome:
fever;
decreased body weight;
general weakness;
epileptiform seizures, headache, changes in size, color of eye structures;
pain in the bones of the hypochondrium;
Syndrome of hormonal disorders
Manifested in certain cancers. It is important for the primary diagnosis of lung cancer in combination with one or more symptoms of pulmonary and extrapulmonary syndrome.
Violations are detected by the results of laboratory tests, namely:
high levels of calcium in the blood;
low levels of sodium in the blood;
Itsenko-Cushing syndrome;
sudden, long-term non-healing skin rashes;
thickening of the joints of the phalanges of the fingers.
The order and expediency of conducting instrumental and laboratory studies, the choice of methods for obtaining material for diagnostic histological studies will be left to oncologists.
Treatment of lung cancer

The standard treatments for lung cancer are:
surgical removal of the tumor;
chemotherapy – the introduction of intravenous chemicals that inhibit the growth of tumor cells.
radiation therapy – exposure to altered cells with hard types of radiation.
Use the above as the sole method or in combination. Some forms, such as small cell carcinoma, do not respond to surgery but are sensitive to chemotherapy.
Chemotherapy for lung cancer
The tactics of mass chemotherapy is determined by the form of the disease and the stage of carcinogenesis.
Common cytostatics are pharmacological drugs that have the ability to inhibit the growth of cancer cells: Cisplatin, Etoposide, Cyclophosphamide, Doxorubicin, Vincristine, Nimustine, Paclitaxel, Carboplatin, Irinotecan, Gemcitabine. These drugs are used before surgery to reduce the size of the tumor. In some cases, the method has a good therapeutic effect. Side effects after the use of cytostatics are reversible.
Relatively recently introduced into practical use:
hormonal treatments;
immunological (cytokinetic) methods of fighting lung cancer.
Their limited use is associated with the complexity of hormonal correction of certain forms of cancer. Immunotherapy and targeted therapy do not effectively fight cancer in an organism with a destroyed immune system.
Promising treatments for lung cancer
Radiation therapy
Visually controlled radiation exposure to a cancer cell, or technology (IGRT). It consists in the irradiation of the damaged cell, its instantaneous correction after sufficient exposure and the transfer of the load to the neighboring area of the damaged tissue.
Contact radiation exposure, or brachytherapy technology. It consists in the delivery of special substances to the tumor tissues, which enhance the targeted effect on damaged cells.
Smart knife technology The principle lies in the perfectly precise impact of the cyber-knife on the accumulation of damaged cells.
Modern chemotherapy
Marking of cancer cells (PDT-technology) with substances that increase sensitivity to external laser exposure and eliminate damage to healthy tissue.
The main disadvantage of new technologies is that they affect the developed pathogenesis, but do not prevent pathological mutations.









