What is appendicitis?
Appendicitis is an inflammation of the appendix. Vivid clinical symptoms and numerous nuances of acute and chronic inflammation of the appendix make the diagnosis and surgical treatment of appendicitis both an easy and complex medical task.
Removal of appendicitis (appendectomy) is the only way to radically treat the acute and chronic forms of this disease. In Russia, at least one million such operations are performed annually.

The paradox is that the diagnosis and removal of appendicitis is a common procedure and a routine abdominal (in the abdominal cavity) surgical operation.
A comparative analysis of the relatively frequent postoperative deaths and “futile” operations, from which even experienced surgeons are not insured, against the background of the simplicity of performing surgical procedures, indicates the complexity and depth of the problem.
Here are the most obvious reasons for unsuccessful appendectomy operations, apart from diagnostic / operative errors and negative physiological aspects (pregnancy, age, poor patient condition):
late treatment of patients in a medical institution, when the pathogenesis has become catastrophic (rupture of the blind process in the abdominal cavity, purulent peritonitis);
general innervation of the appendix and adjacent internal organs is accompanied by atypical manifestations and pain (outside the right iliac region)
general lymph and blood circulation of the appendix and adjacent organs, as a result of which the pathogenesis spreads to neighboring organs.
Involvement of adjacent organs through the blood, lymph and nervous system does not allow adequate detection of inflammation of the appendix even with the help of modern instrumental methods – contrast radiography, CT, ultrasound, diagnostic laparoscopy. In addition, difficulties arise when examining pregnant women in the late stages of gestation, the elderly and children.
General universal recommendations for suspected inflammation of the appendix:
Pathogenesis can develop rapidly. Do not wait for a spontaneous solution to the problem, go to the hospital! Doctors should have enough time to make the right decision.
Use knowledge about the features of appendicitis, obtained in the framework of health education, to timely contact a medical institution in case of malaise.
We will try to give the most useful information for people who do not have a medical education. So, in order.
Why does the removal of appendicitis not reduce the quality of life?

For a long time, even among doctors, the appendix was considered “an extra organ.” Its purpose was unclear. Uselessness was proved by the preservation of health after removal, and subsequent human diseases did not reveal any etiological connection with the removed organ.
Histological, physiological and immunological experiments established the importance of the appendix for the body. It consists in the participation of the body in the following processes:
the formation of a cellular link of immunity – there is a lot of lymphoid tissue in the walls of the appendix;
the production of hormones that stimulate peristaltic contractions of the intestine, involved in the synthesis of amylase, one of the digestive enzymes that break down food starch.
The absence of visible disturbances on the part of the body in persons who underwent appendectomy is explained by the inclusion of compensatory mechanisms. The functions of the lost organ are taken over by other structures. Therefore, appendectomy is a relatively safe intervention. In the absence of adverse pathologies, homeostasis in people with a remote appendix is preserved. However, you should be aware that the absence of the appendix reduces the “margin of safety” of the body.
How does appendicitis occur?
There are several theories. We will present an alternative vision of the problem, although the root cause remains with the causative agents of banal infections (staphylococci, streptococci, Escherichia coli, other anaerobes).
The involvement of banal microflora in the pathogenesis of appendicitis is possible when several unfavorable local and general factors coincide against the background of a decrease in social and living conditions.
Local factors:
Narrowing or blockage of the mouth of the appendix (calculi, swallowed foreign objects, worms, mucus, anatomical deformities of the appendix, inflammation), which is accompanied by stagnation of the contents of the appendix cavity and a decrease in the blood circulation of the organ;
Blood clots in the vessels of the organ, which cause the development of areas of stagnation and necrosis;
Spasms, blood clots and stretching of the walls of the appendix reflexively activates the peristalsis of the small intestine, stimulates excessive mucus formation, disrupts the microcirculation of blood and lymph in the capillaries.
General factors:
The nature of nutrition and food preferences of a sick person (monodiets, exclusively meat or carbohydrate nutrition negatively affect);
The presence of a chronic infectious process in adjacent organs (in the genitourinary system, stomach, intestines, pancreas, respiratory tract);
Defects in the immune system, including allergic pathologies.
Social factors:
Chronic stress (against the background of a labile nervous system);
The influence of climatic conditions on the body (frequent sore throats, colds, accompanied by the activation of opportunistic microflora).
The combination of three factors leads to the active reproduction of microbes and the development of purulent processes in the appendix.
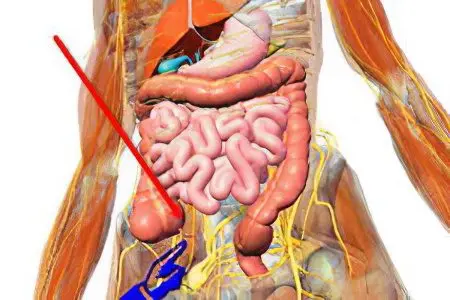
On which side is appendicitis in a person?

The appendix is located in the projection of the right iliac region.
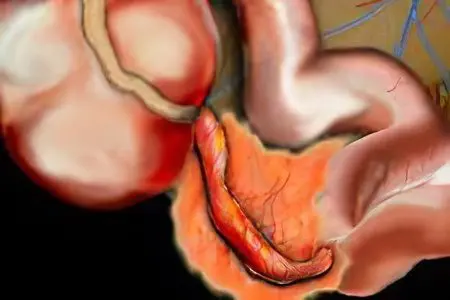
The appendix is a continuation of the caecum. It begins below the border of the transition of the ileum to the large intestine. The length of the blind section of the intestine is 6-8 cm, the width is 7 cm. Due to the absence of the mesentery, this section is mobile. The appendix (appendix) is about 8 cm long and 0,5-1,0 cm wide. There are several options for the location of the appendix in the human abdominal cavity. Accurate topography is of great importance for the surgeon when choosing an operative approach to the organ. In other possible situations, not related to medical research, knowledge of the exact topography is not required.
The nature of pain in appendicitis
The earliest and most commonly reported symptom by patients is pain. In the debut, the pain is characterized by paroxysmal manifestations against the background of the absence of precursors of the disease. Initially, the localization of pain is identified by sensations in the navel and / or solar plexus. Further, within a few hours to two days, the pain shifts to the region of the right sigh.
The nature of the pain is constant, it is aggravated by coughing, it is of a disturbing nature, that is, its intensity is often low. The characteristic posture of the patient is on the back with bent legs. There are other positions that reduce pain.
Acute appendicitis
Develops rapidly, characterized by vivid symptoms.
There are three main types of acute inflammation of the appendix:
catarrhal;
Phlegmonous;
Gangrenous.
catarrhal form characterized by morphological disorders detected by instrumental methods. In the first hours, signs of circulatory stagnation are observed at the apex of the process. They are accompanied by edema, lymphatic effusion and swelling of the mucous membrane. Cone-shaped foci of catarrhal inflammation appear. Changes in the initial period are reversible.
Phlegmonous appendicitis develops by the end of the first day. The walls of the organ thicken significantly, the mucous membrane at the mouth becomes covered with pus, multiple abscesses are found.
Gangrenous appendicitis – manifested by destructive changes in the walls and the transition of inflammation to the surrounding tissues (periappendicitis) or the mesentery (mesenteriolit).
In some cases, appendicitis ends with the disappearance of symptoms and even recovery.
Signs of acute appendicitis
Characteristic manifestations of the debut:
Pain;
Nausea, Vomiting caused by reflex excitation;
Delayed bowel movements and gases;
Diarrhea is a sign of intoxication of the body;
Often hyperthermia (up to 38,00C), rarely the norm;
Coating on the tongue, at first moist, and after a while dry.
The main symptom of appendicitis – pain – is determined by provocation tests. Dozens of different tests have been proposed to determine appendicitis, four main pain tests:
Rovsing;
Sitkovsky;
Exemplary;
Shchetkina-Blumberga.
This test does not describe research methods. For their implementation, it is necessary to know the topographic anatomy of the internal organs of a person well. Surgeons in the detection of appendicitis use more than a dozen different methods for determining the signs of the disease.
Symptoms determined by the doctor during a clinical examination:
Pulse above 100 beats / min against a background of slight hyperthermia;
The difference in temperature, determined in two places – rectally and in the armpit. Normal rectal temperature is higher by 0,8-1,00C, and appendicitis with peritonitis is characterized by a more significant difference;
Arterial pressure within the individual norm, a decrease in blood pressure is evidence of intoxication;
Bimanual (simultaneously with two hands) palpation of the right and left sides of the abdomen is accompanied by pronounced pain in the right iliac region and reflex tension of the abdominal wall at the site of increased pain;
Tapping with fingers on different parts of the abdomen is manifested locally by increased pain.
According to the time from the onset of the disease, early and late stages of acute appendicitis are distinguished. The early stage lasts two to three days. On the third day (late stage), with an unfavorable development of the pathology, the inflammatory process spreads beyond the organ, and then perforation (rupture) of the walls of the appendix is possible. With a favorable course of inflammation, the attack ends with recovery.
Signs of a favorable (abortive) course of acute inflammation:
Temperature normalization;
The disappearance of pain;
Normalization of appetite.
It is possible to preserve the pain reaction for some time with deep probing in the right iliac region. The patient, including those with a favorable course of the disease, continues to be under the supervision of a surgeon. The decision on further actions (surgical intervention or conservative treatment) is made by the attending physician. The danger of a favorable course is the transition of the acute phase to the chronic one.
There are three scenarios of pain reactions in this form of pathogenesis:
Strong, occurs suddenly, proceeds sharply, ends quickly;
Moderately pronounced, proceeds for a long time, fades slowly;
Progressive, increases gradually, is debilitating in nature, spreads beyond the inflamed organ, which is associated with effusion outside the appendix of the inflammatory infiltrate and the transition of inflammation to the organs adjacent to the appendix.
The first two scenarios may end in spontaneous recovery, or a transition to a sluggish form. The latter ends only with an appendectomy.
Localization of pain depends on the location of the appendix.
In addition to the right sigh, pain can radiate and be reflected in other places:
When the process is displaced closer to the pelvic cavity, pain in the rectum may occur.
When the process is located behind the cecum, acute pain is localized on the right side of the lower back, in the anatomical region called the triangle of Petit (Petit).
The lumbar triangle (another name for Petit’s triangle) is defined on the back side of the body, on the lower back, with a center in the projection area of the kidneys. Other areas of pain response are possible.
Complications of acute appendicitis
Two main types. Associated with unsuccessful appendectomies – the first type of complications; with pathologies of the appendix not removed – the second type of complications.
I. The first type – postoperative complications
Distinguish:
Early, which develop during the first three days after surgery;
Late, they develop on the third or fourth day, sometimes after the removal of sutures, on the 7-10th day.
Perhaps the three main options for early complications are postoperative bleeding, intestinal paresis and acute urinary retention:
Intraperitoneal postoperative bleeding. The reason is unsuccessful ligation of a blood vessel, bleeding of a small mesenteric vein or artery;
Venous bleeding is characterized by wetting of the edges of the surgical wound and soaking the dressing with blood;
Arterial bleeding, in addition to the above, is manifested by a rapid deterioration in well-being, pallor of visible mucous membranes and a decrease in body temperature.
Postoperative intestinal paresis. The reasons are the incorrect imposition of the intestinal suture, which narrows the intestinal lumen, and the reflex stop of peristalsis due to adhesive inflammation. Paresis manifests itself:
Vomiting of undigested food some time after eating;
Lack of defecation;
The absence of peristaltic noises in the intestines.
Acute retention of urine. The reason is a reflex spasm of the sphincter of the bladder. Manifested by the accumulation of urine, unsuccessful urge to urinate, overflow of the bladder and pain in the lower abdomen.
Late postoperative complications. Develop on the third or fourth day, sometimes later. This is inflammation of the mucous membranes of the peritoneal wall, suppuration of the sutures of the postoperative wound:
Peritonitis is inflammation of the peritoneum. The reason is the development of a purulent process. It is manifested by soreness, tension of the abdominal walls, fever, vomiting of digested food or bile in its absence.
Wet sutures after an operating wound. The reason is individual intolerance to surgical threads, insufficient disinfection of the suture site on the stump of the excised appendix. Manifested by fever, vomiting, pain.
II. The second type of complications
They occur in people who delay contacting a medical institution. Complications are associated with difficulties in diagnosing the complex pathogenesis of appendicitis. They have a very high risk of death. Especially in people of advanced and senile age.
There are pathological processes accompanied by:
Infiltration of inflammatory exudate around the inflamed appendix;
Abscesses of the abdominal cavity and liver;
Peritonitis due to inflammation of an unremoved organ;
Douglas space abscess;
Sepsis – infection of the blood through the general circulatory system and the flow of pathogenesis to neighboring organs (uterus in women, liver, kidneys, urinary organs).
Diagnosis of acute appendicitis

The program of measures to identify appendicitis includes two stages (at home and in the hospital):
Prehospital observation of the patient. Determination of signs of appendicitis by the sick or close people. After confirming symptoms similar to appendicitis, you should immediately contact an ambulance and prepare ahead of time:
Required documents – passport, insurance policy, possibly a medical card if it is at home;
Detailed oral description of the symptoms of the disease.
Hospital examination of the patient includes:
physical methods (history taking, examination, palpation, percussion, thermometry);
Instrumental imaging (diagnostic laparoscopy of the abdominal organs, plain radiography, computed tomography (CT) with contrast, ultrasound);
Laboratory research.
In the presence of a bright clinical picture, appendectomy is carried out on the basis of physical research methods. The reason for the operation is also a high level of leukocytes – protective cells in the blood, determined by laboratory methods, as well as positive diagnostic tests:
Bartomier Michelson. The diagnostic value of this test is very high. The probability of appendicitis is 97% when a bright response is established. The essence of the method: the subject is placed lying on his left side, while palpation of the right sigh is manifested by unpleasant sensations;
Exemplary. The diagnostic value is 83%. The essence of the diagnostic study: the patient, while lying down, raises his right leg in a straight position. The pain is aggravated by muscle tension and displacement of internal organs;
Rovsing. Diagnostic value 79%. The essence of the method: with the fist of the left hand, the doctor presses on the projection of the descending branch of the colon. The right hand presses on the opposite side of the abdomen. Inflammation of the process is manifested by an unpleasant sensation on the right side of the body.
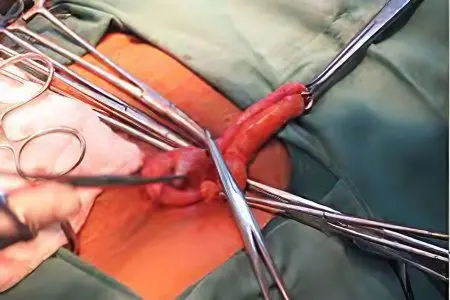
Treatment of acute appendicitis
All patients with signs of “acute abdomen” are necessarily hospitalized in order to differentiate appendicitis from similar pathologies.
During this period, a rectal and / or vaginal examination is mandatory, other types of visualization of the pathological process:
In the presence of a bright clinical picture of catarrhal appendicitis, the operation is indicated within the first two to four hours after admission to the hospital;
Appendiceal colic. Unclear signs of colic (for example, diffuse loose or dense inflammatory exudate around the organ) require differentiation of causes. At the hospital stage, additional studies are carried out, the patient is prescribed conservative inpatient (less often outpatient) treatment for 10-20 days (antispasmodics, desensitization, antibiotics). Treatment is usually carried out in a hospital. Removal of the inflamed organ upon confirmation of appendicitis is carried out in a planned manner after the removal of the phenomena of inflammatory infiltration;
Appendicitis complicated by peritonitis (diffuse, spilled). In this case, a diagnostic laparotomy is indicated – a surgical operation, during which an audit of the state of the internal organs is carried out. In recent years, laparoscopy is more often used – a study of the state of internal organs using an observation device through a small puncture of the abdominal wall.
Depending on the results of laparotomy (laparoscopy), the subsequent algorithm of actions may be as follows:
When confirming catarrh, an audit of the ileum and uterus is performed (in women);
When confirming gynecological pathology against the background of inflammation of the process, an operation is recommended;
If phlegmonous appendicitis is detected, the operation is postponed until the completion of treatment, during this period antibiotics are administered intraperitoneally for 3-4 days.
After complex treatment and normalization of the state of health, a planned operation is performed.
Emergency care for acute appendicitis
The patient and his relatives at the prehospital stage should follow several rules.
Attention! Absolutely forbidden:
Local heating of the abdomen;
Removal of pain sensations by medicines, alcohol, drugs and any other means;
The use of laxatives (oil, salt, vegetable and any other);
Enemas are the introduction of liquids into the rectum.
Emergency care for the patient consists of the following activities:
It is necessary to lay it on a horizontal surface and ensure peace;
It is allowed to reduce pain with the help of local dry cooling (a container with cold water or ice) on the right side of the abdomen. Between the container with cold and the skin, it is imperative to make a gasket from several layers of fabric – this will reduce the risk of local negative cold exposure;
Immediately call an ambulance (tel. 03).
Urgent measures in a medical institution are regulated by official regulations.
Chronic appendicitis
This disease is much less common than acute appendicitis. Diagnosis is difficult due to the possible distortion of the nature of pain, unclear clinical symptoms and the absence of macrochanges on the walls of the appendix. It is believed that the chronic form of appendicitis is a continuation of acute inflammation. Repeated catarrhal benign inflammation is accompanied by the growth of the walls of the organ and connective tissue with the formation of adhesions.
Pathology leads to a narrowing of the lumen of the process. If the lumen narrows at the mouth of the organ, this causes the accumulation of pus, mucus and transudate in its cavity.
This state is defined as:
Empyema of the appendix – accumulation of pus;
Dropsy of the appendix – accumulation of transudate (fluid);
Mucocele of the appendix is a collection of mucus.
Pathology associated with thickening of the process walls is much less common. This process is called fibroplastic appendicitis. It resembles an infectious process – tuberculosis (tubercles on the organ), a tumor (overgrown poorly differentiated tissue), actinomycomas – fungal lesions (seals, fistulas on the organ). Sometimes diverticula (pockets) are found on the appendix.
Most often, however, there is no change. This complicates the diagnosis and makes treatment ineffective.
Can appendicitis be chronic?
The chronic form of appendicitis is isolated as a separate disease. It is subdivided into:
Primary chronic appendicitis – when indolent symptoms, including persistent pain in the iliac region, occur in people who have never previously suffered from an acute form of the disease;
Secondary-chronic appendicitis – when the symptoms developed after one or more acute attacks of appendicitis.
In the scientific world there is no consensus on the legitimacy of the nosological unit “primary chronic appendicitis”. In the study, there may be no visible violations of the morphological structures of tissues, although the clinical signs of inflammation are pronounced.
After unsuccessful operations, the pain persists, since its cause is associated with damage to other organs. Currently, histological studies are the most reliable marker of chronic inflammation.
Signs of chronic appendicitis

Pain is not a constant, obligatory sign. In some cases, it is insignificant or has a paroxysmal character. It can be manifested by aching, debilitating unpleasant sensations of low intensity. In some cases, it increases after eating or exercising, sometimes accompanied by constipation and diarrhea. In women, the pain is aggravated during a period of regular hormonal changes.
They help to suspect the presence of a chronic form of appendicitis, tests that provoke a response to pain, including:
Feeling the walls of the abdomen – the pathology is manifested by pain on the right side;
The patient on the left side is restless on palpation of the right side of the abdomen.
Other samples used for diagnostic purposes:
An attempt to raise the right leg causes discomfort;
A decrease in muscle tone on the right side of the abdomen is a sign of chronic appendicitis.
When walking on the treadmill, the right leg gets tired much faster than the left.
The best diagnosis of chronic inflammation of the appendix is laparoscopy. Radiography, its modifications, ultrasound have limited diagnostic value in chronic inflammation. These methods do not reveal microscopic changes in the walls of the process.
The use of radiation diagnostic methods is limited to the identification of indirect signs of inflammation:
The delay of the contrast agent in the cavity for several days;
Uneven (fragmentary) filling with a contrast agent.
When making a diagnosis, they exclude similar diseases of internal organs, such as:
Diseases of the gastrointestinal tract (chronic forms of cholecystitis and pancreatitis);
Diseases of the urinary system (inflammation of the kidneys, ureters);
gynecological diseases (violation of the regularity of cycles, chronic inflammation of the appendages).
Treatment of chronic appendicitis
The most effective surgical removal of the appendix. The probability of a favorable outcome is lower in comparison with the removal of the process in the acute phase. Efficiency is reduced due to complex diagnostics and a high risk of developing adhesive processes in the abdominal cavity.
In some cases, drug treatment is indicated before the removal of the process. The patient is given intravenous antibiotics. During this period, patients need dietary nutrition in order to reduce the load on the intestines.









