Contents
Shoulder-shoulder periarthritis is an inflammatory process accompanied by degenerative changes in the periarticular tissues that are involved in the functioning of the shoulder. Ligaments, muscles, tendons, synovial bags suffer from humeroscapular periarthritis.
The humeroscapular type of pathology in the general system of periarthritis is more common than others. It accounts for up to 80% of the total number of rheumatic inflammations of the shoulder. Approximately 10% of the world’s population is affected by this disease in one way or another. Such a wide spread of the disease is due to the fact that the muscle tendons surrounding the shoulder joint are in tension almost all the time. As a result, degenerative processes develop there very early. Most often, humeroscapular periarthritis is diagnosed in women who have crossed the age limit of 55 years, although its symptoms may begin to bother at an earlier age.
Patients most often complain of right-sided periarthritis, since the load on the right limb is usually higher. However, the development of left-sided and bilateral humeroscapular periarthritis is not excluded.
Causes of humeroscapular periarthritis

Scientists consider two main reasons that can lead to the development of humeroscapular periarthritis:
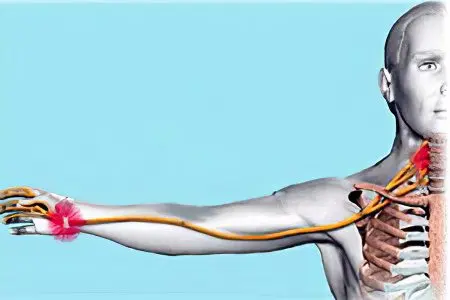
Neurodystrophic changes occurring in the tendons, which manifest against the background of diseases of the musculoskeletal system in the cervical spine (osteochondrosis, spondylosis, displacement of the vertebrae). In this case, the nerve roots are pinched, the vessels at the reflex level are compressed, the normal blood supply to the shoulder joint begins to suffer. As a result, the development of inflammation and the manifestation of dystrophic processes in the tendons of the shoulder girdle.
Injury to the soft structures of the shoulder girdle. A person can receive injuries when performing cyclic stereotypical actions that load the shoulder joint, or in the event of an emergency (falling on an outstretched arm, receiving a strong blow to the shoulder, dislocation of the joint, etc.). In this case, the tendons are torn, the integrity of the shoulder cuff is violated, the tissues responsible for the movement of the shoulder swell, the normal blood supply system fails and inflammation develops.
Sometimes the causes of the development of humeroscapular periarthritis cannot be found out.
It is impossible not to mention the risk factors that increase the likelihood of manifestation of periarthritis in the humeroscapular region:
The person is over 40 years of age.
Hypothermia, both local and the whole organism as a whole.
Pulmonary tuberculosis.
Prolonged exposure to dampness.
The presence of human diseases of the musculoskeletal system: arthrosis, sciatica, arthritis.
Cervical spondylosis with radicular syndrome in 80% of cases is combined with humeroscapular periarthritis.
Diabetes.
The presence of congenital anomalies in the development of the humeroscapular region.
Neuropsychiatric disorders, including against the background of traumatic brain injury. Other dangers include brain tumors and kinsonism.
coronary heart disease. At the same time, periarthritis is able to manifest both at the peak of an angina attack and during its extinction.
Postponed myocardial infarction. Periarthritis is observed on average in 10-15% of patients.
Hemiplegia (complete unilateral paralysis of the arm), which occurs after a stroke, or against the background of other lesions of the spinal cord and brain.
Parkinson’s disease.
Operations that interfere with the blood supply to the area of the shoulder joint, such as a mastectomy.
What happens with humeroscapular periarthritis?

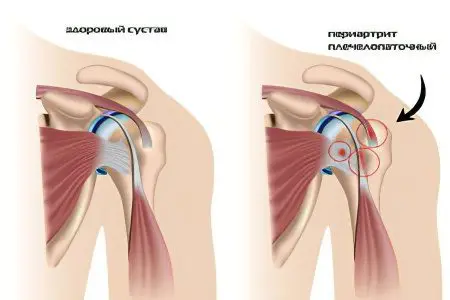
To understand exactly what processes occur in the tendons during the development of humeroscapular periarthritis, it is necessary to understand the structure of the joint, as well as to consider the pathogenesis of the disease.
The system that is responsible for hand movements is quite complex. In addition to the “true” shoulder joint, the “second” shoulder joint is of no small importance. It is represented by musculoskeletal and capsular-tendon formations. Its upper layer is formed by the acromion and deltoid muscle, and the lower layer is formed by the tendons responsible for the rotation of the shoulder. The tendons are intertwined with a muscle capsule covering the true joint and the humeral head. These connections together form the cuff, which is responsible for the rotation of the shoulder. The center of the “second” shoulder joint is represented by serous bags and loose connective tissue. This allows the muscles to slide freely relative to each other.
With the development of the disease, collagen fibrils are torn, which are located inside the tendons, which leads to the formation of foci of necrosis on them. Subsequently, the foci of necrosis are opened into the cavity of the serous bags, which represent the middle layer of the “second” shoulder joint. If the disease has a severe course, then a complete rupture of the tendon is possible.
In parallel, a reactive inflammatory process develops and gains momentum. The tendon thickens, irregularities appear on it, it is possible that it will completely turn out of the intertubercular groove.
Complications of the disease
Against the background of the current inflammatory process, calcifications begin to form in the tendon. Some of them are able to dissolve on their own, while others penetrate the serous bags and provoke additional foci of necrosis in their cavities. With chronicization of the process, the walls of the bags may merge, which causes a pronounced limitation of mobility in the shoulder joint.
Not only the “second” shoulder joint, represented by muscles, suffers, but also the “true” joint. In the place where it borders on the inflamed tendon, wrinkling of its capsule may occur. This process is called fibrous capsulitis. As a result, the normal mobility of the shoulder suffers even more.
Another danger that threatens people with humeroscapular periarthritis is the compaction of bone tissues of the large tubercle of the head of the shoulder with the removal of lime from it and the formation of osteophytosis in this area.
In addition to the fact that the foci of necrosis are able to calcify and scar, disrupting the mobility of the limb, they can also undergo aseptic inflammation.
Blocked shoulder syndrome with its complete immobilization is the most formidable complication of the disease.
Symptoms of the humeral scapular periarthritis

There are three forms of humeroscapular periarthritis, each of which is characterized by a specific set of symptoms.
A simple form of the disease, which foreign authors call “a simple painful shoulder.”
Acute form of the disease.
A chronic form of the disease, which is called “frozen shoulder”, “ankylosing periarthritis”, “blocked shoulder”.
If the disease develops against the background of an injury, then from the moment it is received until the first symptoms appear, it can take from 3 days to a week. Often this factor is the reason that patients are not always able to point out the cause that led to the formation of periarthritis.
Symptoms of a simple form of periarthritis, which proceeds quite easily and has the most favorable prognosis:
Complaints of mild pain in the shoulder area.
Pain appears only at the moment when a person performs certain movements (he can designate them independently).
There is no pain at rest.
The pain intensifies at the moment when the patient tries to rotate with the participation of the shoulder joint, or tries to overcome resistance.
Restriction of mobility is weakly expressed: it is difficult for the patient to raise his hand high up, and also to bring it behind his back. If this succeeds, then the patient is not able to touch the spinal column with his fingers. Other movements do not cause pain.
Perhaps the appearance of pain during a night’s rest, this is especially true for people who are used to sleeping on their backs.
During palpation, the doctor reveals painful points located on the anterolateral surface of the shoulder, if the supraspinatus and infraspinatus muscles are involved in the pathological process. The bicipital groove responds with pain if the head of the biceps muscle becomes inflamed.
The general condition of the patient is not disturbed, blood counts remain within the normal range.
Most often, a simple form of humeroscapular periarthritis stops on its own after a month.
With an unfavorable course of the disease, with an increase in the load on the diseased area, or with repeated injury, simple periarthritis can turn into an acute form. However, in some cases, acute periarthritis develops as an independent disease and is not preceded by a simple form of the disease.
Acute periarthritis is characterized by the following symptoms:
The pain comes on suddenly and tends to get worse. It is caused by the migration of calcifications from short tendons into synovial bags. The pain is diffuse and most often occurs after severe physical exertion.
The pain is localized not only in the shoulder area, but also goes to the neck and arm.
During a night’s rest, the pain intensifies.
Rotating the joint and pulling the arm back causes the patient severe pain. Therefore, his movements are severely limited.
Relief comes when a person holds a hand near the chest, while bending it at the elbow.
The frontal surface of the shoulder has a slight swelling.
The general well-being of the patient is disturbed: the body temperature rises to subfebrile levels, insomnia increases, and performance deteriorates.
The blood picture shows an increase in ESR, and during the X-ray, calcifications are most often detected.
Acute periarthritis lasts about a month or less. Then the pain decreases, the range of motion is restored. In some cases, calcifications are able to resolve on their own.
If acute periarthritis has not been qualitatively treated, then in 50% of cases it will turn into a chronic form of the disease.
The symptoms of the disease are as follows:
The pain is not too intense, localized in the shoulder.
During movement of the shoulder joint, the pain tends to increase, which causes some discomfort.
During a night’s rest, there may be a feeling of ache in the shoulder girdle.
Painful shootings periodically occur when you try to rotate your hand, when making sudden movements.
If chronic periarthritis is ignored, it can provoke ankylosing periarthritis. This process does not happen instantly, but over several years.
Its symptoms are as follows:
The tissues surrounding the joint become very dense to the touch.
The shoulder will be completely immobilized.
When you try to raise your hand or put it behind your back, a person experiences a sharp pain, which is almost unbearable.
This is the final stage of the development of the disease, which is observed in approximately 30% of all patients.
Algodystrophic syndrome
Algodystrophic syndrome is a special form of humeroscapular periarthritis. This syndrome was first described by Steinbrocker in 1947. Also, algodystrophic syndrome is called “shoulder-hand”.
It is characterized by the following symptoms:
The appearance of sharp pains.
The presence of cold, dense and diffuse edema in the tissues.
Cyanosis of the hand and fingers.
Thinning of the skin.
Strengthening the fragility of the nail plates.
Atrophy of muscle tissue and subcutaneous adipose tissue.
Formation of contracture of the fingers.
Sharp restriction of mobility of the shoulder and hand.
Risks of developing algodystrophic syndrome:
In 20% of cases, the disease develops after a heart attack. The disease manifests itself approximately 1-6 weeks after the occurrence of a cardiovascular catastrophe and is characterized not only by pain in the limb, but also by its coldness, increased sweating, and cyanosis of the skin.
In 20% of cases, the syndrome occurs against the background of existing spondylosis of the cervical spine.
In 23% of cases, the causes of development remain unclear.
In 10% of cases, algodystrophic syndrome develops after an injury. Men are most often affected. Pain in this case occurs spontaneously, they make themselves felt during flexion and extension of the shoulder.
Against the background of other diseases, this form of periarthritis develops in 6% of cases.
The course of the disease is protracted, it can last for several years. Although it is not uncommon when, after 1-2 years of treatment, the patient gets rid of vasomotor disorders and he manages to partially restore the movements of the limb. Although it will not be possible to get rid of contracture of the fingers and trophic changes 100%.
Diagnosis of shoulder periarthritis

If you experience pain in the shoulder and with limited movement, you should consult a doctor. The therapist deals with the diagnosis of humeroscapular periarthritis. It is possible that after the examination, the doctor will redirect the patient to a narrower specialist: a surgeon, neurologist, rheumatologist or orthopedist.
In addition to an external examination of the patient and taking an anamnesis, the doctor will definitely evaluate the motor activity of the shoulder joint, palpate the area of inflammation.
To clarify the diagnosis and find out the causes of the development of periarthritis, an x-ray of the diseased joint and cervical spine is performed, it is also possible to conduct ultrasound and MRI diagnostics.
As for laboratory tests, the doctor sends the patient for blood donation. If the patient’s periarthritis is in the acute stage, there will be an increase in ESR and CRP. In other forms of the disease, the blood picture remains unchanged.
If there is a need for surgery, then before it is carried out, the patient can be referred for invasive diagnostic procedures: arthrography or arthroscopy.
It should be taken into account that periarthritis of the humeroscapular region can be confused with other diseases that give similar symptoms. Therefore, it is important to make a differential diagnosis with arthritis, arthrosis, Pancoast syndrome against the background of lung cancer, thrombosis of the subclavian artery.
Treatment of humeroscapular periarthritis

Treatment of humeroscapular periarthritis should be long and persistent. First of all, it is necessary to remove the load from the diseased tendon, which minimizes the risks of its further traumatization. For this purpose, support bandages or plaster splints are used.
Inflammation and pain are relieved with the following medications:
From the group of NSAIDs: Ketorol, Nimesil, Dicloberl, etc. These drugs not only eliminate the pain attack, but also relieve inflammation from the affected muscle.
Painkillers, for example, Baralgin or Analgin.
Muscle relaxants, for example, Mydocalm. This group of drugs allows you to relax the muscles, relieve spasm from them by reducing muscle tone.
Chondroprotectors, for example, Structum. These drugs are aimed at improving the physiological activity of the joint, reducing intra-articular fluid, and eliminating swelling. Thus, not only an analgesic, but also a therapeutic effect is achieved.
If the pain cannot be eliminated by the above drugs, then it is possible to block the subscapular nerve. The injection is administered into the subacromial space. For this purpose, use the drug Diprospan. Injections are given 2 times during the entire treatment, the interval between procedures should be 20 days, but not less. A combination of drugs such as Flosteron, Metipred and Diprospan is also possible.
Before agreeing to perform blockades, you should familiarize yourself with the side effects that they can give: atrophy of the skin at the injection site, inflammation of the shoulder joint, degenerative processes in the periarticular region, tendon atrophy, etc.
Another type of blockade of pain in shoulder periarthritis is the introduction of Novocain. The effect of such an injection is observed almost instantly. Often, novocaine blockades are combined with glucocorticoids. This allows you to reduce inflammation, eliminate pain, relieve swelling. However, it should be understood that hormonal drugs depress the patient’s immune system, so they can be used under strict medical supervision.
Physiotherapy in the treatment of humeroscapular periarthritis

Physiotherapeutic techniques are a separate direction in the treatment of humeroscapular periarthritis.
The following actions are possible:
Electrical stimulation of the muscles of the shoulder girdle. The procedure allows you to normalize muscle tone.
Laser treatment. To get rid of pain, you must go through at least 10 sessions, the duration of each of them is 5 minutes.
Phonophoresis improves the nutrition of tissues, contributes to their speedy recovery.
Shock wave therapy quickly heals damaged areas of the tendons, promotes the dissolution of calcifications.
Other methods of treating periarthritis: acupuncture, magnetotherapy, hydrotherapy, hirudotherapy, stone therapy, taking sulfide and radon baths.
Manual therapy is indicated in the case when periarthritis was provoked by displacement of the vertebrae.
Surgery

In the case when drug correction does not allow to achieve the desired effect for 6-8 months, the patient is indicated for surgical intervention.
It is useful in the following situations:
Partial damage to the integrity of the tendons, which led to disruption of the muscles.
Extensive cuff tear.
Transosseous damage to the cuff.
Inflammation of the radial or subscapular nerve.
tunnel syndrome.
However, the operation may not always be carried out.
Obstacles to surgical intervention are:
Formed persistent contracture.
Purulent inflammation, regardless of its location.
The presence of contraindications to the introduction of anesthesia.
Refusal of the patient from the operation.
Surgical treatment of advanced form of shoulder periarthritis is reduced to arthroscopic subacromial decompression. Its essence lies in the fact that the patient is removed acromion (a small process on the shoulder blade), as well as one ligament in the joint. This allows you to ensure that the tissues do not injure each other, which means that inflammation is eliminated. In parallel, the doctor removes the formed contractures. If the operation is successful, then the patient fully recovers the entire range of motion.
It is possible to carry out surgical intervention both with an open method and with the use of endoscopic equipment. The postoperative period requires wearing an orthosis, which allows the patient to recover faster.
You do not need to follow any special diet during treatment. It is only important to ensure that the diet is balanced and allows you to cover all the needs of the body, which spends additional strength on the restoration of damaged tendons.
During the acute stage of the disease, massage is strictly contraindicated. It is prescribed at the stage of recovery. However, the procedure should be carried out exclusively by a specialist with a medical education, bypassing the inflamed areas of the muscle.
Therapeutic exercise

Therapeutic gymnastics is one of the conditions for a speedy recovery. Well, if there is an opportunity to perform exercises in the water. Swimming and hydrokinesitherapy are included in all recommended complexes for humeroscapular periarthritis. Classes in the pool allow not only to normalize muscle tone and remove excess stress from them, but also to increase the range of motion in the damaged joint.
The main goals pursued by the gymnastic complex:
Normalization of blood flow.
Enrichment of tissues with oxygen.
Elimination of congestion.
Muscle strengthening.
Normalization of metabolic processes.
You should not start performing the gymnastic complex during the acute stage of the disease, with severe pain in the joint.
A few effective exercises that will speed up recovery:
Feet should be shoulder-width apart, arms raised above your head. You should reach with your fingertips to the ceiling, but do not take your feet off the floor. Both arms are extended first, and then each limb in turn.
Hands should be spread apart and left at shoulder level. Next, you should perform turns with the body and head, but at the same time keep your hands in their original position.
Raise your hands above your head and grab your elbows. You need to slowly move your hand back, without making sudden movements.
Perform simple gymnastic exercises should be 3 times a day. This is the best prevention of recurrence of the disease.
Prevention of shoulder periarthritis

Measures aimed at the prevention of humeroscapular periarthritis:
It is necessary to prevent macro and microtrauma of the shoulder girdle.
It is important to avoid excessive and monotonous loads on the shoulder joint.
All diseases of the spinal column must be treated in a timely manner.
Hypothermia should be avoided.
To prevent recurrence of the disease, you need to perform physical exercises aimed at working out the muscles of the shoulder.
You should always monitor your posture, regardless of the type of activity that a person is engaged in.
Answers to popular questions
Is disability indicated for humeroscapular periarthritis? If the patient has a persistent violation in the functioning of the shoulder joint, and the operation does not allow to restore the range of motion, then the patient is sent to a commission regarding the receipt of disability.
Is it possible to visit the bath with periarthritis? You can visit the bath only at the stage of recovery, when an acute attack of the disease has been removed.
Is it possible to warm up a sore part of the muscle? Warming up can be performed only when there is no acute inflammation. In other cases, thermal procedures can increase blood circulation in the damaged area and reduce pain.
Which doctor treats shoulder periarthritis? A rheumatologist is engaged in the treatment of periarthritis, but for the initial diagnosis, it is necessary to contact a local therapist.









