Contents
Reticulocytosis is an increase in the level of reticulocytes in the peripheral blood by more than 1%. Reticulocytosis is a sign of increased erythropoiesis (the process of forming blood cells).
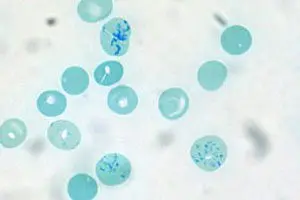
Reticulocytes are young forms of red blood cells. They are formed from normoblasts after the loss of their nucleus. Therefore, reticulocytes are non-nucleated immature erythrocytes. After entering the blood, they begin to mature. This process takes 1-2 days. They enter the bloodstream directly from the bone marrow in which they are born. Therefore, the number of reticulocytes reflects the ability of this organ to regenerate. With an increase in the level of reticulocytes, one can speak of increased erythropoietic activity of the bone marrow.
The sizes of reticulocytes exceed the sizes of mature erythrocytes. Their cytoplasm contains a basophilic mesh, which looks like small grains, filaments and glomeruli. These elements are sticky ribosomes and mitochondria.
Depending on the degree of maturity, the following reticulocytes are distinguished:
Progenitor cells of erythrocytes containing a nucleus. They are called erythronormoblasts.
Reticulocytes containing granularity in the form of a ball.
Reticulocytes containing granularity in the form of a dense network.
Reticulocytes containing granular filaments.
Reticulocytes containing individual grains.
The vast majority of reticulocytes (about 80% of all cells) contain granularity in the form of filaments and individual grains. An indicator of the norm of reticulocytes is their content in the blood from 0,2 to 1% of the total number of red blood cells. Within a few hours, these reticulocytes will mature into full-fledged red blood cells, and new reticulocytes will come in their place. If their number is exceeded by more than 1%, doctors speak of reticulocytosis.
There is evidence that the level of reticulocytes in the body of a woman exceeds the level of reticulocytes in the body of a man. In addition, in children after birth (for several days), the level of reticulocytes in the blood can be from 5 to 10%, but then it decreases.
Symptom reticulocytosis
Reticulocytosis itself is not a pathology. Moreover, in some cases, this laboratory indicator is considered by specialists as a sign of good bone tissue regeneration (true reticulocytosis). However, at the same time, the number of reticulocytes should increase not only in the peripheral blood, but also in the bone marrow itself.
If reticulocytosis develops against the background of aplastic anemia, then the patient will complain of the following symptoms:
Increased fatigue and tiredness.
Pale skin.
Noise in ears.
Dizziness.
Dyspnea.
Frequent nose and gum bleeding.
Diseases such as: stomatitis, pneumonia, infections of the skin and urinary tract.
Hemolytic crisis is a syndrome that is accompanied by intravascular or intraorgan destruction of red blood cells.
The following signs indicate a hemolytic crisis:
Tachycardia, shortness of breath, dizziness, pale skin, or its icteric color.
Nausea, vomiting, abdominal pain, fever.
Disturbance of consciousness and convulsions.
Enlargement of the spleen in size.
Darkening of urine.
Symptoms of occult bleeding depend on its intensity. Common signs include dizziness, shortness of breath, thirst, pale skin, fainting, or lightheadedness. The rate of increase of these symptoms will depend on the intensity of bleeding.
Malaria, which is accompanied by reticulocytosis, can begin acutely, or manifest itself as a slight increase in body temperature, headaches, and malaise. On the 3-5th day of the patient’s illness, attacks begin to haunt, which are alternately replaced by chills, fever and sweating. These paroxysms are repeated up to 10-14 times, after which there is an improvement. However, the disease has a tendency to recur.
Polycythemia with reticulocytosis develops for a long time and gradually. Most often, it is diagnosed by chance during a blood test. The patient is periodically worried about heaviness in the head, dizziness, his vision may deteriorate, sleep disorders appear. The most pathognomic sign of polycythemia is vascular plethora, when the skin acquires a cherry-red color, this is especially noticeable on the face, neck, hands and mucous membranes. In this case, the hard palate of the patient has a normal color, and the soft palate acquires a cyanotic hue.
Acute hypoxia with reticulocytosis develops quickly, in a few minutes. If oxygen starvation is not stopped, then irreversible consequences occur in organs and tissues and a person may die. This condition is manifested by the insufficiency of all organ systems. First of all, the central nervous system suffers, breathing and heartbeat slow down, blood pressure decreases. Organ failure turns into a coma and agony, after which the person dies.
Causes of reticulocytosis

The causes of reticulocytosis can be the following:
Reticulocytes can reach a level of 60% with hemolytic anemia. Hemolytic crises lead to significant jumps in reticulocytes in the blood.
On the 3-5th day after acute blood loss, all patients develop a reticulocyte crisis.
An increase in the level of reticulocytes may indicate occult bleeding, for example, in patients with peptic ulcer, typhoid fever and other lesions of the gastrointestinal tract.
Malaria and polycythemia will lead to reticulocytosis.
If the patient was diagnosed with iron deficiency anemia, then after 3-5 days from the start of treatment, the level of reticulocytes in the blood will increase. This indicates the effectiveness of the therapy. A similar situation is observed in the treatment of pernicious anemia.
Hypoxia of the body provokes an increase in the level of reticulocytes in the blood.
The penetration of tumor metastases into the bone marrow leads to reticulocytosis.
Against the background of massive destruction of red blood cells, the level of reticulocytes can rise up to 50%.
Taking certain medications can provoke the development of reticulocytosis. These drugs include: Corticotropin, antipyretic and antimalarial drugs, Furazolidone, Levodopa.
True reticulocytosis is indicated by an increase in the number of reticulocytes in the peripheral blood and in the bone marrow.
False reticulocytosis is indicated by an increase in the level of reticulocytes in the peripheral blood, but with their normal level in the bone marrow.
The following reasons can provoke false reticulocytosis:
The presence of Jolly bodies or malarial plasmodium in the blood.
high leukocytosis.
Deformed hemoglobin.
The presence of giant platelets in the blood.
Hyperthrombocytosis.
Diagnosis of reticulocytosis

There are certain indications for performing a reticulocyte analysis:
The need to evaluate erythropoiesis in hemolysis or bleeding.
Evaluation of bone marrow capacity for recovery after the patient has been treated with cytostatics or after surgery for transplantation of this organ.
Evaluation of the possibilities of erythropoietin production in patients undergoing kidney transplantation.
Passage of doping control by people professionally involved in sports.
Diagnosis of anemia, regardless of its cause.
Search for the causes leading to a decrease in the level of red blood cells.
Search for the causes that lead to insufficiency of the function of hematopoiesis of the bone marrow.
Search for the causes that lead to a violation of the regenerative capacity of the hematopoietic organs during the treatment of anemia. Evaluation of the effectiveness of the ongoing treatment of anemia.
Evaluation of the effectiveness of ongoing therapy using erythropoietin or erythrosuppressors.
Reticulocyte counting can be carried out in several ways: using the method of luminescence microscopy, counting the number of reticulocytes in a blood smear with the introduction of special dyes into it, counting the number of reticulocytes using a hemolytic analyzer.
Treatment of reticulocytosis

In order for the level of reticulocytes in the blood and in the bone marrow to return to normal, it is necessary to eliminate the cause that provoked their increase.
With aplastic anemia, a person must be hospitalized. To prevent infectious complications, it should be in an isolated box. Most often, patients with aplastic anemia are prescribed immunosuppressive therapy. In this case, the patient receives injections of immunoglobulin and cyclosporine A. If necessary, he is transfused with a platelet or erythrocyte mass, and plasmapheresis is performed. It is possible to remove the spleen. Bone marrow transplantation significantly improves the prognosis for patient survival.
In a hemolytic crisis, assistance to the victim should be provided immediately. He is urgently hospitalized, replenishes the volume of lost blood and eliminates harmful products of hemolysis in the blood. For this, albumin, a solution of glucose, vitamin B2, sodium chloride, Desferal are administered intravenously. With the help of Furosemide, diuresis is stimulated to prevent the development of renal failure. To enhance the diuretic effect, Eufillin is prescribed. Be sure to use glucocorticoids to suppress the body’s immune response. If necessary, the patient is given a blood transfusion. To prevent a second crisis, removal of the spleen is recommended.
Latent bleeding should be detected and stopped in a timely manner.
Treatment of malaria requires infusion therapy, heavy drinking, bed rest. Quinine is used to eliminate the infection from the body.
To normalize the volume of circulating blood, it is required to perform bloodletting in volumes up to 500 ml 2-3 times a week. Removed blood volumes are replenished using saline or reopoliglyukin. In severe cases of polycythemia, cytostatics are prescribed or radioactive phosphorus therapy is carried out.
Acute hypoxia requires the elimination of the causative factor and the maintenance of body cells with oxygen. In this case, oxygen is pumped into the lungs under pressure (hyperbaric oxygenation).
Treatment of reticulocytosis is reduced to the elimination of the pathological cause, if any. Often, an increase in the level of reticulocytes occurs during the treatment of iron deficiency anemia and is a favorable prognostic sign. In this case, no therapeutic measures are required. After some time, reticulocytosis will stop on its own.









