Contents
Reflux-esophagitis can rightfully be considered one of the most common diseases of the esophagus. As of 2010, 5 million people in Russia suffer from it. No more than 2 out of 10 people receive adequate therapy for their disease. It often occurs due to contact of the mucous membrane of the esophagus with the contents of the stomach. The latter, as you know, has high acidity and affects the lower esophagus. As a result, a person feels pain, heartburn and other symptoms of indigestion.
Unfortunately, it is impossible to trace the real incidence of reflux esophagitis, because it often occurs with mild symptoms and people do not seek help from specialists. For patients with reflux esophagitis, constant heartburn that occurs after eating is a variant of the norm. They stop the discomfort with an Almagel tablet or other usual remedy. Such carelessness can cost a person dearly, since reflux esophagitis is not the safest disorder. Often it causes severe bleeding and even cancerous tumors.
The second category of patients can be called people with persistent, severe symptoms of the disease, requiring outpatient treatment. The most dangerous are refluxes with complications (ulcers and bleeding). This form of the disease requires hospitalization.
GERD and reflux esophagitis
Reflux esophagitis is often confused with gastroesophageal reflux disease (GERD). These are two different conditions that differ, first of all, in the approach to therapy. Their main differences are presented in the table.
Differences between reflux esophagitis and GERD
Comparative characteristics | GERD | Reflux-esophagitis |
Concept definition | When the disease occurs, the reflux of gastric contents into the esophagus. At the same time, the mucous membrane lining it suffers, since it is not adapted to contact with acids. | |
Are there any changes in the esophageal wall? | If the disease has an uncomplicated course, then the mucous membrane retains its normal structure. | The walls of the esophagus are always inflamed. |
Making a diagnosis | The doctor makes a diagnosis already during the initial examination of the patient. | It is possible to make a diagnosis only after performing FGS with endoscopic examination of the esophagus. |
Features of therapy | Medicines are taken only as needed. | A person should regularly take drugs that will prevent narrowing of the esophagus, bleeding, cancerous tumors and other complications. |
Thus, esophagitis is an inflammation of the esophagus, which can be diagnosed during fibrogastroscopy. GERD can develop without esophagitis, but esophagitis is always combined with GERD.
Causes of reflux esophagitis
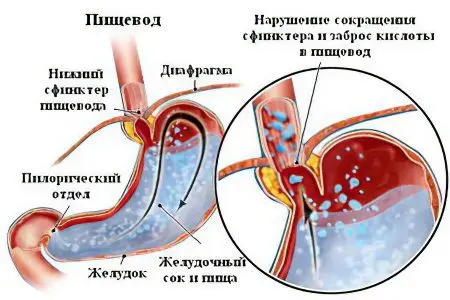
The lower esophageal sphincter is a natural valve between the esophagus and the stomach, which prevents its contents from escaping back. Food that the stomach has begun to digest moves lower and does not rise into the esophagus. Sometimes there is a reflux of contents from the stomach, but this does not happen often during the day and does not cause discomfort in a person, therefore it is considered a variant of the norm. The disease is said to be in the case when the reflux of gastric contents occurs very often. At the same time, food masses contain a large amount of acid.
Reflux esophagitis has a number of different causes. In young children, it usually occurs due to an underdeveloped neuromuscular apparatus, namely, the cardiac esophagus. That is why babies often burp.
Also, the cause of reflux esophagitis can be gastritis or peptic ulcer: because of them, the pressure inside the stomach increases, and the mobility of the gastrointestinal tract is significantly reduced. In addition to heartburn, the patient feels spasms, hypertonicity. Stress, obesity, decreased salivation and malnutrition can disrupt intestinal motility. Among the most dangerous foods are citrus fruits, chocolate, tomatoes, fatty and spicy foods, coffee and spirits. Smoking and the use of certain medications, especially sedatives and sleeping pills, prostaglandins, nitrates and nitrites, also harm the esophagus and stomach.
Before starting therapy, it is important to establish and eliminate the pathological factor that led to the development of reflux esophagitis. Otherwise, the disease will always recur.
The reason for the development of the disease | Mechanism of disease development | Conditions that can provoke reflux esophagitis and GERD |
Increased pressure on the lower esophageal sphincter | High intra-abdominal pressure, which causes food to rise up. |
|
Weak lower esophageal sphincter | If the valve does not work, then the reflux of contents from the stomach into the esophagus occurs very often. |
|
Increased acidity of the stomach | If the gastric contents contain too much hydrochloric acid, then even single reflux of food into the esophagus can lead to the development of the disease. Sometimes gastric juice has an increased aggressiveness due to the fact that it contains too many enzymes. |
|
The symptom is reflux esophagitis

It is very important to pay attention to the first symptoms of reflux esophagitis, which can be divided into two categories. The first category is the esophageal manifestations of reflux esophagitis, and the second category is the extraesophageal clinic.
Esophageal symptoms are caused by damage to the mucous membrane of the organ. They appear as follows:
Heartburn. Heartburn becomes more intense after drinking alcohol, after exercise, after overeating. Although in patients with reflux esophagitis, heartburn can occur at almost any time. The more affected the mucous membrane of the esophagus, the stronger this symptom will be. Some diseases also affect the frequency of heartburn: inflammation of the gastric mucosa, ulcerative defects of the digestive organs, etc.
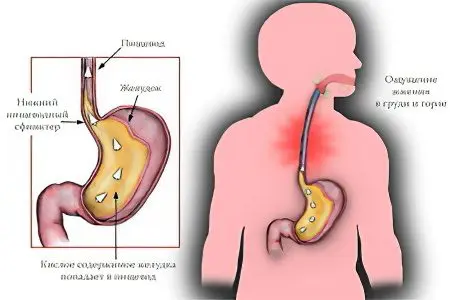
Pain. Painful sensations are concentrated behind the chest, and sometimes rise higher. They are almost always associated with heartburn. You can cope with pain if you take an antacid, for example, Rennie or Almagel. Pain is related to eating. This is its distinguishing feature from heart pain, which cannot be stopped with antacids.
Belching of sour contents. This symptom is indicated by most people suffering from reflux esophagitis. Often, some food comes out during burping.
Swallowing disorder. This symptom is observed in those patients who suffer from esophagitis for a long time. The food bolus passes through the esophagus with difficulty, this process is accompanied by pain.
In addition to the symptoms described above, patients may suffer from damage to the vocal cords, lungs, bronchi, and trachea. Acidic contents can enter the organs of the respiratory system and cause inflammation. As a result, a person can be treated for bronchitis, asthma, laryngitis and even pneumonia for a long time, and the exact cause of the disturbance will not be established.
If reflux esophagitis has a chronic course, then additional symptoms of the disorder are:
Voice change. He becomes hoarse.
Cough, which, if the trachea is affected, will be dry. If inflammation of the bronchi or lungs occurs, the cough becomes wet.
Sore throat.
Coryza that haunts the patient for a long time.
The esophagus and other organs that suffer from the damaging effects of stomach acid will bleed. As a rule, bleeding is small, but can lead to anemia. Its symptoms are manifested in increased weakness, weakness. There may be a craving for unusual smells. In patients, the condition of nails, skin and hair often worsens.
Diagnosis of reflux esophagitis
A standard examination is not enough to make a diagnosis. Laboratory diagnostics practically does not provide information on the disease. With its help, it will only be possible to assess the general state of human health, as well as to identify some complications of the disease. When a person comes to an appointment with a doctor, he will prescribe him only 3 tests: blood, urine and feces. Changes in reflux esophagitis will only affect the blood picture.
Abnormalities in the blood picture in reflux esophagitis | What do these violations indicate? |
An increase in the erythrocyte sedimentation rate in women up to 15 mm/hour, and in men up to 10 mm/hour. A decrease in the level of red blood cells in women up to 3,6 * 1012, and in men up to 4,4 * 1012. Decrease in hemoglobin level in women up to 120 g/l, and in men up to 130 g/l or less. | An increase in ESR indicates that there is inflammation in the body. A drop in the level of hemoglobin and red blood cells indicates developing anemia, in which the number of oxygen-carrying cells decreases. |
It is possible to make a diagnosis only with the help of such a method of examination as FGS – fibrogastroscopy.
Features of the FGS

During the procedure, a thin tube is inserted into the patient’s oral cavity, which is equipped with a camera and a working tool. Before the examination, you need to stop eating 3-4 hours before it starts. Do not drink water 40 minutes before the procedure.
The patient will need to take a towel and a disposable napkin with them. The person is laid on the left side. To reduce the discomfort that occurs when the tube is inserted, the patient is sprayed with an anesthetic solution on the root of the tongue. Then a mouthpiece is inserted into the patient’s mouth, it will need to be clamped with lips and teeth.
FGS cannot be called a pleasant procedure, but in time it takes no more than 7 minutes. At this time, the doctor examines the condition of the mucous membranes of the esophagus and stomach. If necessary, tissue sampling is carried out. Later it is studied under a microscope. The doctor will be able to detect atypical cells, bacteria, thinned epithelial structures in it.
The doctor will be able to make an initial diagnosis immediately after FGS. If a laboratory study of tissues is required, then the data can be obtained after 7-14 days.
Evaluation of results
After the examination, the doctor will be able to make the following conclusion:
Catarrhal reflux esophagitis. This is the most “harmless” version of the disease. The mucous membrane is loose, full-blooded, there are no serious injuries on it. This type of esophagitis is not divided into stages.
Erosive reflux esophagitis. In this case, the esophagus will be covered with ulcers, or thinned sections of the epithelium will be found on it. This condition requires immediate treatment, as it threatens the development of bleeding, can lead to stenosis or complete obstruction of the organ. Ulcerative defects are dangerous degeneration into cancerous tumors. The erosive form of the disease is divided into stages. The doctor must take the material for microscopic examination without fail.
Presence of bleedingwhich complicates erosive esophagitis. Often, in such patients, anemia is detected during laboratory diagnostics, which is accompanied by appropriate symptoms (fatigue, taste distortion, etc.). A person can undergo outpatient treatment, since there is no threat to his life. However, if cancer cells are found in the tissues taken for analysis, hospitalization is required.
Fibrin deposits on the walls of the esophagus. This sign indicates that the disease progresses in a person for a long time.
Sore throat after FGS

After FGS, the patient may experience sore throat. It occurs in 90% of people. Even if the procedure was carried out perfectly, it is impossible to exclude the appearance of discomfort. The pain develops for the reason that the device injures the mucous membrane of the esophagus. The stronger they are, the longer the person will be haunted by pain. Sometimes they remain for 14 days after the procedure. Pain will pass when the mucous membrane of the esophagus is restored.
If the pain is intense, then you need to see a doctor to make sure that the esophagus was not severely injured. In the hospital, the patient may have a chest x-ray or x-ray. If free air is found in the organs, this indicates a rupture of the esophageal wall. In this case, the person needs immediate surgical intervention. However, one should not be afraid of FGS, since the described case is the rarest exception, which is practically not registered in modern medicine.
As a rule, sore throat after the procedure does not require any therapy. The mucous membrane of the organ will recover on its own. If the pain causes discomfort, then you can take a drug from the NSAID group, for example, Nimesulide or Meloxicam. They are unable to harm the digestive system. However, in such cases it is better to consult a doctor.
Degrees and stages of the development of the disease
If the patient has an erosive form of the disease, then the doctor in the diagnosis will have to indicate the degree and stage of its development. To understand what exactly the doctor had in mind, you can use the table.
The degree of development of the disease | Los Angeles classification of the disease | Stage | Classification of the disease according to Savary-Miller |
A | Thinning of the epithelium 1-5 mm long | 1 | Erosion single |
B | Thinning over 5 mm | 2 | Erosions are confluent, but do not cover the entire esophagus along its circumference |
C | Erosion covers 3/4 of the organ | 3 | Erosions and inflammation cover the esophagus around the entire circumference |
D | More than ¾ of the body is affected | 4 | There are complications of the disease in the form of stenosis, ulcerative defects, etc. |
| 5 | There are symptoms of precancer in the lower esophagus (Barrett’s esophagus). | |
The higher the stage of the disease, the higher the likelihood of complications.
Treatment of reflux esophagitis
Reflux esophagitis is dangerous because it does not cause intense symptoms, so many people do not see a doctor on time. Pathology progresses, which leads to the development of dangerous complications. To prevent such a situation, it is necessary to start therapy in a timely manner.
Treatment of reflux esophagitis is primarily to eliminate the disease that caused it (gastritis, neurosis, peptic ulcer or gastroduodenitis). Proper therapy will reduce the symptoms of reflux, help reduce the harmful effects of gastric contents thrown into the esophagus, increase the resistance of the esophageal mucosa, and quickly clear the stomach after eating.
General recommendations

A person with reflux esophagitis needs not only to take medications, but also to reconsider his lifestyle in general.
Therefore, doctors give all patients the following recommendations:
Refusal of cigarettes. Nicotine provokes an increase in the acidity of gastric juice, relaxes the walls of the esophagus, which leads to the progression of the disease.
You can not go to bed immediately after eating. Within half an hour after eating, you need to remain in a sitting position, or walk a little at a slow pace. Do not run or lift weights. Any physical activity after eating is prohibited.
Weight lifting restrictions after meals are 3 kg for women and 5 kg for men.
Alcohol should be avoided 2-3 hours before bedtime. You also need to eat no later than this time.
To prevent the symptoms of the disease from aggravating in the supine position, it is recommended to place an additional pillow so that the upper body is elevated. This will reduce heartburn and chest pain.
Clothing should not constrict the abdomen. Do not tighten the belt, corset or belt after eating.
It is important to direct efforts to get rid of concomitant diseases: gastritis, obesity, ulcers, etc. If this is not done, then it will not be possible to get rid of reflux esophagitis.
Compliance with diet

A very important component of the treatment of reflux esophagitis is diet. Patients should give up fatty and spicy foods, coffee, chocolate, citrus fruits, tomatoes, alcohol and smoking.
Many people think that dieting means eating tasteless foods and restricting yourself in everything. Actually it is not. It is important to remove only certain foods from the diet. Using various culinary techniques, you can make your menu varied, tasty and very healthy.
The following products are banned:
Drinks containing caffeine: Coca-Cola, energy drinks, cocktails.
Gas drinks.
Alcoholic drinks.
Flour products that increase the production of acid in the stomach.
Chocolate and sweets.
Dairy products.
Linseed and olive oil, animal fats. Vegetables and fruits that contain acids: radishes, pomegranates, citrus fruits, etc.
Food should not be fried using animal or vegetable fats. Such products contribute to the fact that gastric juice is produced in excess quantities. This leads to the progression of the disease. Food should be boiled, steamed, stewed in its own juice.
Tips for preparing healthy and tasty meals:
Wrap. Using foil or parchment paper, you can cook almost any meat product without adding oil. Spices can be replaced with salt, dried herbs, natural vegetables.
Use of the oven. Baking is the best cooking method for people suffering from esophagitis. At the same time, oil is not added to the dishes, which reduces the fat content of meat products. Products can be filled with water. In one baking sheet, not only meat is prepared, but also a side dish, which allows you to reduce your time in the kitchen. It is important to bake dishes no longer than 70 minutes. The optimum temperature is 200 °C.
Preparation dishes in a double boiler or in a slow cooker. These modern appliances can significantly increase the value of any dish, add juiciness to it. Steam processing gives the products a pleasant taste and does not destroy the vitamins present in them. You can add salt to dishes, as well as herbs.
Cooking food on an open fire. This method of processing products should be practiced during field trips. Excess fat will leave the meat, while it retains its juiciness and tenderness. It is important not to marinate foods in spicy brines.
To get rid of reflux esophagitis, you need to reduce the consumption of oil and mayonnaise, ketchup, mustard and other hot sauces. They negatively affect the condition of the mucous membranes of the gastrointestinal tract, increase the acidity of gastric juice.
Dishes should not be too hot or cold, as they irritate the esophagus.
Taking medications
Antacids. If the above recommendations do not help, then special medications are prescribed that reduce the acidity of the stomach – antacids. In case of peptic ulcer and erosion, it is recommended to take antisecretory drugs (proton pump inhibitors or H2-blockers). This will reduce the pressure inside the stomach, make it resistant to eating, normalize intestinal motility and eliminate the symptoms of reflux esophagitis.
Modern proton pump inhibitors represented by 5 substances: omeprazole, lansoprazole, rabeprazole, esomeprazole, pantoprazole. To determine the drug, you need to visit a gastroenterologist.
Before starting treatment, it is necessary to study some features of proton pump inhibitors (data from 2014-2016).
Individual characteristics of the patient | Which drug is better to choose? | Why this drug and not another? |
It is required to take drugs that help reduce the AP enzyme (Enalapril, Lisinopril, Captopril, Ramipril, etc.). | Pantoprazole or rabeprazole | In people who suffer from heart disease or high blood pressure, taking omeprazole and esomeprazole increases the likelihood of heart attack and stroke. These drugs neutralize the protective effect of agents for the treatment of cardiac pathologies, as they help to reduce the level of AP enzyme. |
Pregnant woman after 13 weeks | Lansoprazole, pantoprazole | The American Physicians Association has not found any toxic effects that these drugs could have on the body of a woman or fetus. They are not prescribed before the 13th week of pregnancy, since at this time the main systems of the future organism are being laid. Omeprazole, esomeprazole and rabeprazole are not prescribed during pregnancy. |
Patients with bronchial asthma | Omeprazole or esomeprazole | Reflux esophagitis and bronchial asthma are interrelated diseases. There is evidence that the listed drugs have a positive effect on the state of the respiratory system. |
Patients with liver diseases (hepatitis cirrhosis, fatty hepatosis, etc.). | Any drugs, but it is better to give preference to rabeprazole. | The minimum dose of rabeprazole is 10 mg, which is 2 times less than the dosage of other drugs. Scientists believe that it is this drug that damages the diseased organ less than the others. |
It is necessary to quickly and permanently lower the acidity of gastric juice | Lansoprazole, pantoprazole or rabeprazole. | The effect of taking omeprazole and esomeprazole develops only 3-4 days after the start of treatment. The rest of the drugs begin to act from the first day they are taken. |

Histamine blockers. If for some reason patients cannot take proton pump inhibitors, then they are prescribed histamine H2 blockers. They are less effective, so they are taken in large doses. They are used only in extreme cases. These are drugs such as: Famotidine, Ranitidine, Nizatidine and Roxatidine.
Prokinetics. It is not enough to simply reduce the acidity of gastric juice, it is important to reduce the number of reflux of its contents into the esophagus. This can be achieved through the use of prokinetics. These drugs improve the contractility of the digestive tract and contribute to the normalization of the movement of food through them.
Such medicines are represented by the following trademarks:
Domperidone (Motilak, Motonium, Motilium). These are the drugs of choice for inflammation of the esophageal wall. They allow you to normalize the work of the sphincter, stomach and intestines.
Cisapride (Coordinax, Peristil). These drugs affect the lower esophageal sphincter, the stomach. Their tone increases, and the frequency of refluxes decreases.
Metoclopramide (Raglan, Perinorm, Cerucal). If reflux into the esophagus occurs very often, and other drugs do not reduce their number, then Metoclopramide is prescribed. However, it has a number of side effects, including: increased fatigue, muscle tics and weakness.
Any drug must be prescribed by a doctor. All of them have indications and contraindications for admission. They need to be taken into account before starting treatment.
To get rid of pain in the esophagus, you need to take antacids. They are also indicated for heartburn. Antacids do not cure esophagitis, but they do an excellent job of stopping its main symptoms. They have a minimal set of contraindications, so they can be used without a medical prescription.
The most famous antacid is Almagel. He showed up before the others. Modern drugs are significantly superior to it in terms of effectiveness. These drugs include: Gaviscon, Maalox, Rennie, Megalac.
They begin to act faster and remain active longer than Almagel. In addition, such drugs better lower the acidity of gastric juice.
[Video] Dr. Evdokimenko – GERD, reflux esophagitis and HEARTBURN – causes, symptoms and effective TREATMENT:









