Contents
Abdominal pain, flatulence, diarrhea? Antibiotics are a double-edged sword – they destroy bad bacteria, but they also weaken the gut microbiota. Fortunately, probiotics come to our aid, i.e. live cultures of bacteria or yeasts, whose main task is to rebuild the digestive tract. We explain when to take probiotics and which ones are best to choose.
Post-antibiotic dysbiosis
Today we know that antibiotic therapy is a “real Armageddon” for the microbiota of our intestines. Due to their antibacterial activity, antibiotics are deadly not only for pathogenic bacteria, but also for beneficial bacteria that naturally inhabit the intestines, which affect many aspects of our life: digestion, immunity, body weight, sleep and even mood.
According to research, 7-day antibiotic therapy may disturb the intestinal microflora for the next 1-2 years. The most common side effect is gastrointestinal disturbance leading to antibiotic-associated diarrhea (AAD), which affects 10 to 40% of patients. adult patients, in the case of children up to 80%!
It is also suspected that disruption of the gut microbiota resulting from exposure to antibiotics increases the risk of some chronic diseases by exacerbating both local and systemic inflammatory responses, leading to metabolic disturbances and immune impairment. It has been shown that the perinatal period, characterized by the development of the immune system and the maturation of the gut microbiota, is a particularly sensitive period in which antibiotic dysbiosis translates into long-term health effects, i.e. a greater risk of diseases later in life, including inflammatory bowel diseases, atopic or metabolic disorders such as type 2 diabetes and obesity.
However, the negative effects of antibiotic therapy can be prevented by following a few guidelines. First of all: we only use antibiotics when indicated, adhering to the recommendations regarding the duration of therapy and dosage. Secondly: we do not forget about protective therapy, i.e. the need to use probiotics, which should be taken during antibiotic therapy and after its completion. Why is it so important? Probiotics taken during antibiotic therapy prevent the occurrence of post-antibiotic diarrhea, and when used after its completion, they help us rebuild the proper intestinal microflora.
What to consider when choosing a probiotic?
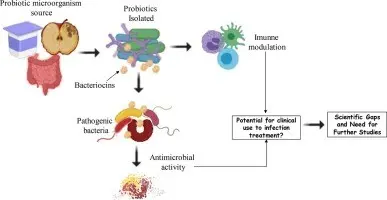
What exactly are probiotics? Their name derives from the Greek “pro bios”, meaning for life, and according to the FAO / WHO definition of 2002, they are living microorganisms that, when administered in appropriate amounts, have beneficial health effects. The microorganisms with a probiotic effect include mainly lactic acid-producing bacteria of the genus Lactobacillus (L. acidophilus, L. casei, L. reuteri, L. rhamnosus) of the Bifidobacterium (e.g. B. animalis) as well as yeast Saccharomyces boulardii.
Importantly, the probiotic effect relates to a specific strain of a microorganism, and not to a genus or species. Hence, the name of a good probiotic should consist of three elements: the generic name (e.g. saccharomyces), species name (e.g. boulardii) and alphabetic strain designation (e.g. CNCM I-745).
The best-studied strains that have been clinically proven to be effective in preventing drug-induced diarrhea during antibiotic therapy are: probiotic yeast Saccharomyces boulardii CNCM I-745 and bacteria Lactobacillus rhamnosus DD
Are you wondering what to consider when choosing a probiotic to an antibiotic? Medications, not dietary supplements, will be by far the best choice. In the case of drugs, manufacturers guarantee the declared content of live microorganisms (yeasts or bacteria) and their survival during the shelf life of the preparation, and the effectiveness and safety of the medicinal product are confirmed by appropriate tests. Additionally, each drug in Poland must be registered with the Office for Registration of Medicinal Products, Medical Devices and Biocidal Products.
The probiotics in the form of drugs most often recommended by doctors and pharmacists to prevent diarrhea associated with the use of antibiotics include Enterol, containing yeast Saccharomyces boulardii CNCM I-745, available in both capsules and sachets.
When to take probiotics – before or after an antibiotic?
It’s time to put theory into practice, that is to explain how to use probiotics correctly. Many people wonder when to take probiotics: before, during or after an antibiotic?
ESPGHAN (European Society for Pediatric Gastroenterology, Hepatology and Nutrition) experts recommend administering the two best-studied probiotics: Saccharomyces boulardii CNCM I-745 lub Lactobacillus rhamnosus GG from the first day of antibiotic therapy in children. For the prevention of induced diarrhea Clostridium difficile recommend serving Saccharomyces boulardii CNCM I-745. The meta-analysis of studies involving adults published in 2021 also confirmed the effectiveness of probiotics in the prevention of post-antibiotic diarrhea (reducing the risk of diarrhea by 38%) in this group of respondents.
When it comes to the time of taking, the probiotics should be taken at a certain distance from the antibiotics, preferably approx. 1-2 hours before or after the antibiotic. The exception is probiotics containing yeast Saccharomyces boulardii CNCM I-745, which can be consumed even simultaneously with an antibiotic, because they are resistant to most prescribed antibiotics.
Another important point is the relationship between the intake of probiotics and meals. Given that the bacteria contained in probiotics are not conducive to an acidic environment, taking them on an empty stomach, in which the pH is high, may unfortunately weaken their effectiveness. Therefore, it is much better to take probiotics with a meal, which is a kind of protective buffer against the damaging effects of gastric juice. We will achieve even more beneficial effects if our meal contains a small amount of fat. Like other drugs, probiotics should be washed down with water at room temperature, not with juice, tea or coffee, and never mixed with alcohol.
When it comes to storage, each manufacturer specifies the temperature range in which a given preparation should be stored on the package insert. Some of them should be kept in the refrigerator and others containing yeast Saccharomyces boulardii (eg Enterol) can be stored at room temperature below 25 ° C.
How long should you use probiotics with antibiotics?
How long should we use a probiotic? It all depends on how intense the antibiotic therapy was and how aggressive the antibiotic was used. Basically, the period of a few or several days after the end of antibiotic therapy is the period of compulsory taking of probiotics. However, you should be aware that this time may be extended to several weeks or even several months! After all, rebuilding the intestinal microflora after antibiotic therapy is a long process and it is worth taking care of its proper course.
If you want to support the multiplication of good bacteria after antibiotic treatment, it is also worth paying special attention to the diet and enriching our daily menu with natural probiotics: silage, buttermilk, kefir or yoghurt. Remember, however, that although fermented milk products and silage are recommended as a daily dietary component, natural products are not able to provide the same effect during antibiotic therapy as probiotic preparations recommended by doctors.
The best way to use probiotics during antibiotic therapy
At the end, it’s time for a short summary, i.e. knowledge in a nutshell. Probiotics based on bacterial strains are best taken at a certain distance from the antibiotic, preferably approx. 1-2 hours before or after the antibiotic, because the antibiotic would negatively affect their operation and reduce the number of viable cells of beneficial bacteria. On the other hand, probiotics containing yeast can be taken freely, even together with an antibiotic, and this will not reduce their effectiveness. An example of the best-studied probiotic strain from this group is Saccharomyces boulardii CNCM I-745, which can be found in the drug Enterol.
Not only the time of administration is important, but also the duration of the probiotic use. According to the latest knowledge, it is recommended to take the probiotic for at least a few more days after the end of antibiotic therapy in order to minimize the risk of the so-called post-antibiotic dysbiosis.
Details on the Enterol.pl website
ENTAS/001/22