In line with its mission, the Editorial Board of MedTvoiLokony makes every effort to provide reliable medical content supported by the latest scientific knowledge. The additional flag “Checked Content” indicates that the article has been reviewed by or written directly by a physician. This two-step verification: a medical journalist and a doctor allows us to provide the highest quality content in line with current medical knowledge.
Our commitment in this area has been appreciated, among others, by by the Association of Journalists for Health, which awarded the Editorial Board of MedTvoiLokony with the honorary title of the Great Educator.
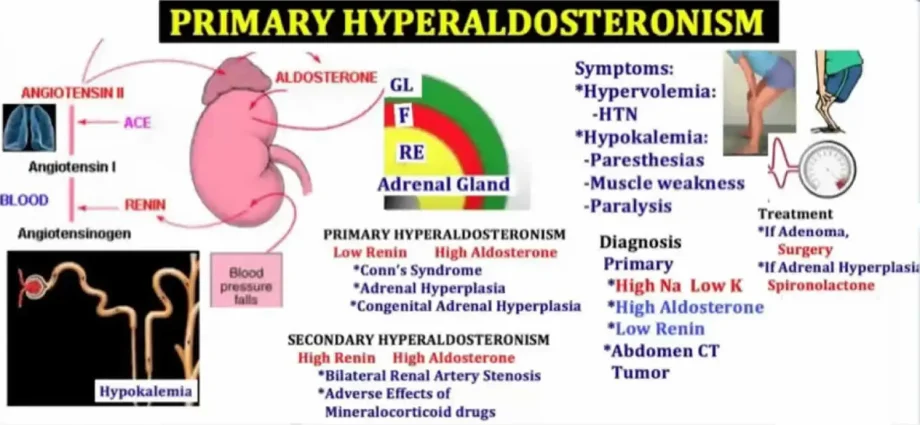
Hyperaldosteronism is an example of an overactive adrenal cortex in terms of increased aldosterone production. The disease is divided into primary (Conn’s disease) and secondary hyperaldosteronism. The symptoms in both cases are very similar. Among other things, you experience increased urine output, headaches, and dizziness.
What is hyperaldosteronism?
Hyperaldosteronism is a condition that results from the excess production of aldesterone by the adrenal cortex. Aldesterone causes the kidney to excrete less water and sodium and more potassium. The following are distinguished in hyperaldosteronism:
- Conn’s syndrome, i.e. primary hyperaldosteronism,
- Secondary aldosteronism (its causes may be decreased blood volume, loss of sodium and increased potassium).
Conn’s syndrome is less common than secondary aldosteronism. In both of these cases, the two are very similar and are usually expressed as:
- arterial hypertension,
- increased thirst,
- passing increased amounts of urine,
- muscle weakness,
- headaches and dizziness,
- Various biochemical changes (e.g. decreased levels of potassium in the blood plasma).
The diagnosis of the disease is carried out in the hospital, and for proper diagnosis it is necessary to assess the symptoms and identify biochemical changes. Treatment of hyperaldosteronism can be surgery (primary type) or pharmacological treatment (secondary type).
Hyperaldosteronism – types and their characteristics
PRIMARY HYPERALDOSTERONISM
It is characterized by a high concentration of aldosterone with reduced plasma renin activity. As a consequence, the patient develops metabolic alkalosis and hypokalemia. Primary aldosteronism is also considered a hormonally conditioned form of arterial hypertension that arises from the autonomic secretion of aldosterone.
Primary hyperaldosteronism – Causes
Primary aldosteronism is considered a common cause of hypertension. The reason for the increased secretion of aldosterone may be:
- a tumor of the adrenal cortex (which produces aldosterone) – this is a rare form of aldosteronism;
- familial type I hyperaldosteronism (inherited autosomal dominant; two genes are mutated: CYP11B1 – encoding aldosterone synatase and CYP11B2 – responsible for 11 – hydroxylase);
- familial type II hyperaldosteronism (also inherited in an autosomal dominant fashion);
- adrenal hyperplasia (bilateral) – is the most common form of primary aldosteronism;
- adenoma of the adrenal cortex (considered the second most common cause of the disease, affects less than half of patients. This adenoma is usually small, benign and unilateral. In patients with adenoma, aldosterone is produced independently of angiotensin II, which may be the basis for the differentiation from adrenal hyperplasia Patients suffering from hyperaldosteronism due to adenoma have more severe hypokalemia and higher plasma aldosterone levels (as opposed to patients with bilateral adrenal hyperplasia);
- ovarian / kidney cancer where aldosterone is produced ectopic.
Primary hyperaldosteronism – Symptoms
The clinical picture of primary hyperaldosteronism is quite diverse. The main symptoms of this ailment are:
- arterial hypertension (occurs due to the influence of aldosterone on the water and electrolyte balance and the hypersensitivity of blood vessels to the hypertensive effect of angiotensin II; due to damage to the vascular endothelium). Due to the excessive synthesis of aldosterone, the excretion of potassium in the urine is increased, which leads to a decrease in its concentration in the blood;
- hypokalemic alkalosis (usually appear as a disease caused by a single adenoma). In the remaining patients, hypokalaemia develops only as a result of taking diuretics or following a high-sodium diet.
In addition, patients with primary aldosteronism develop left ventricular mass hypertrophy and advanced organ changes. Mass hyperplasia is greater than in the group of patients with essential hypertension. More often it happens:
- increasing the thickness of the complex of the inner and middle membranes of large arteries,
- endothelial dysfunction,
- excessive stiffness of vessel walls,
- left ventricular relaxation disorders,
- albuminuria,
- in some patients, renal cysts and metabolic syndrome were reported.
Primary hyperaldosteronism – Diagnostics
Screening for primary hyperaldosteronism is performed in patients with difficult-to-treat hypertension. Due to the introduction of the aldosterone-renin ratio (ARR), the frequency of diagnosis of this ailment increased. However, such an assay is more effective in patients who have a normal potassium concentration and often a normal aldosterone concentration showing, for example, a low plasma renin activity that does not respond to stimulation by stimuli.
Primary aldosteronism also occurs when there is no evidence of the presence of factors reducing plasma aldosterone concentration or its daily urinary excretion. Braking tests are also used, e.g .:
- test with captopril;
- inhibition test with 0,9% NaCl solution;
- fludrocortisone test.
Important: Tests for primary aldosteronism have been shown to be false.
Imaging tests are also used in diagnostics, including computed tomography and magnetic resonance imaging. In addition, adrenal scintigraphy is performed. If there are differences in the size of the adrenal glands, adrenal veins are additionally catheterized (performed in a few centers).
Primary hyperaldosteronism – Treatment
The choice of the correct treatment depends on the cause of the primary aldosteronism. The primary therapeutic agent is the aldosterone antagonist spironolactone. It should initially be taken at a dose of 100-400 mg per day, and then the dose may be reduced to 50 mg / day. Prolonged use of this drug may cause side effects, such as impotence or menstrual disorders in women.
Another drug (also an aldosterone anthogonist) is eplerenone. It has a comparable effect to spironolactone. It is still being investigated in patients with primary aldosteronism.
SECONDARY HYPERALDOSTERONISM
It is a condition characterized by an excessive secretion of aldosterone as a result of disturbances in the renin-angiotensive system caused by various diseases that are not related to the primary secretion of aldosterone in the adrenal glands. Stimulation of the renin-angiotensive system causes an increased amount of aldosterone and thus hypertension.
The renin-angiotensive system
It controls the volume of body fluids, i.e. blood pressure at the same time. Aldosterone is secreted from the adrenal cortex and retains sodium in the body, thus increasing renal reabsorption. Water is absorbed together with sodium in the kidneys. For this reason, the high aldosterone go-to causes the volume of body fluids to increase, and hence to arterial pressure.
The causes of secondary aldosteronism
The excessive amount of aldosterone in secondary hyperaldosteronism is a consequence of the presence of other ailments or taking certain medications. However, the main causes of this condition are:
- taking laxatives and diuretics,
- loss of sodium
- pregnancy poisoning,
- nephrotic syndrome,
- low volume of circulating blood,
- myocardial infarction,
- heart failure
- cirrhosis of the liver, e.g. with ascites
- taking estrogens (hormonal contraception),
- presence of a tumor that secretes renin,
- accelerated phase of arterial hypertension.
Secondary aldosteronism is most often caused by a low blood supply to the kidney. This may be due not only to low body fluid volume, but also to a narrowing of the renal artery.
Secondary hyperaldosteronism – Symptoms
The main symptom of this condition is arterial hypertension, which often does not respond to treatment. In addition, there may be edema of hepatic origin, low blood potassium levels and excessive urinary potassium excretion.
Secondary hyperaldosteronism – Diagnostics
In both primary and secondary aldosteronism, blood aldosterone levels will be elevated, therefore blood and urine tests to differentiate them are not necessary. In the diagnosis of the secondary form of the disease, tests of the level of ARO (plasma renin activity) are important. This activity will be significantly increased when the renin system is stimulated for a long time.
Secondary hyperaldosteronism – How is it treated?
Treatment methods depend on the cause of the condition. The aim is to eliminate the underlying disease that significantly affects the high concentration of aldosterone in the blood. In patients who present with renal artery stenosis, a so-called angioplasty, which helps to effectively get rid of both secondary hyperaldosteronism and arterial hypertension.
Pharmacological agents include potassium and spironolactone, which blocks the aldosterone receptor and thus reduces its concentration in the blood and lowers ARO. Furthermore, spironolactone does not have a diuretic effect and does not lead to a significant loss of potassium in the urine.