Contents
Infections during pregnancy pose a significant problem as they can be a threat to both the mother and the developing baby. For most infectious diseases, there are vaccines that protect against the disease. However, the issue of immunization during pregnancy is still controversial.
A few words of introduction
Protective vaccinations are an important element in preventing infectious diseases or reducing the risk of complications resulting from contracting a specific infectious disease.
The worldwide introduction of preventive vaccination programs allowed, among other things, the complete elimination of smallpox or a very significant reduction in the incidence of diphtheria or polio.
The fact that most vaccinations target childhood diseases, but these diseases are also a problem in adults. In addition, there are a number of protective vaccines that are applicable regardless of age.
Infections during pregnancy constitute a very important problem, as they pose a threat to the health of both the woman and the fetus and, consequently, may affect the development of the born child. In addition, due to specific changes in the body of a pregnant woman, these diseases often have a more severe course, with a higher risk of mortality than in other people. In addition, a number of infectious diseases can damage the fetus, leading to birth defects, miscarriages or fetal death.
Common diseases that damage the fetus during pregnancy include: rubella, cytomegaly, syphilis, and to a lesser extent: influenza, chickenpox, herpes or viral hepatitis. On the other hand, infections with meningococcus, pneumococcus or influenza virus can be life-threatening for pregnant women.
For most of the diseases mentioned, there is a prophylaxis in the form of protective vaccines.
Controversies
And here, the basic problem begins – the safety of immunization during pregnancy and its impact on the development of the fetus. A large group of doctors believe that preventive vaccinations are contraindicated during pregnancy and should be performed at the time of pregnancy planning. Nevertheless, life shows that it is not always possible to determine the date of pregnancy and often this is the result of chance. In addition, in some diseases, e.g. influenza (pregnancy may be severe), annual vaccination is important in prevention due to the variability of the virus, and the flu season may fall out when pregnancy is already a reality.
The main source of unclear criteria for vaccinating pregnant women is due to the lack of clinical trials assessing the impact of vaccinations on the fetus, because bioethical committees do not approve this type of research as a precautionary measure. Most often, the data allowing to draw conclusions about the impact of a particular type of vaccination on the fetus come from cases of vaccinating women unaware of being pregnant.
According to the recommendations of the American Advisory Committee on Immunization (ACIP), when vaccinating pregnant women, the risks to the fetus and the pregnant woman related to a given infectious disease and its complications should be considered.
It is very important in the risk assessment to take into account the type of vaccine and the period of pregnancy.
Breakdown of vaccines
The main division of vaccines is related to the type of element of the microorganism – the antigen that causes the human body to produce protective antibodies, and we can distinguish vaccines containing:
– live microorganisms devoid of virulent properties (so-called attenuated strains); e.g. tuberculosis, polio, measles, mumps, rubella, chicken pox
– killed microorganisms; e.g. typhoid fever
– processed products of bacterial metabolism (bacterial toxins) – the so-called toxoids (formerly toxoids); e.g. tetanus, diphtheria
– broken microorganisms or their fragments – the so-called subunit vaccines; e.g. hepatitis B, anti-pneumococcal; against meningococcus; against Haemophilus influenzae type B
Depending on the type of vaccine, subunit vaccines and toxoid-containing vaccines are considered safe during pregnancy (no evidence of harmful effects on the fetus of this type).
However, the use of live vaccines during pregnancy is not recommended. A woman should be vaccinated at least 4 weeks before the planned pregnancy. When a live vaccine has been administered to a pregnant woman, the woman should be informed of the potential effects of the vaccine on the fetus, but this situation may never be an indication for termination of pregnancy.
Taking into account the period of pregnancy, vaccinations in the second and third trimesters are safer than in the first.
In some infectious diseases in pregnant women, in order to reduce the risk of developing the disease or reduce complications, it is possible to use passive immunization, i.e. administration of immunoglobulin preparations. This type of treatment has no negative effects on the fetus.
The most common vaccines for pregnancy
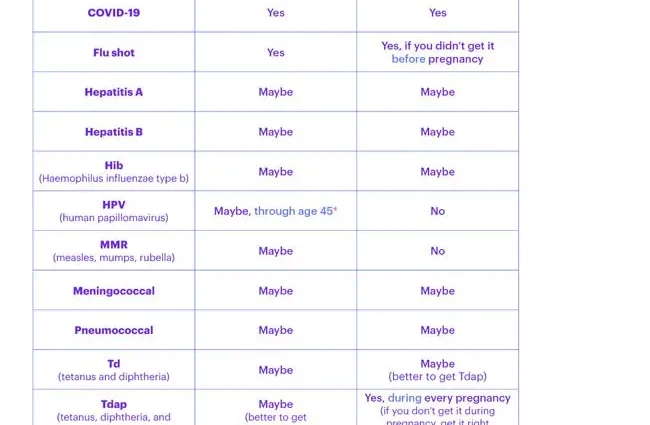
American Advisory Committee on Immunization (ACIP) recommendations for selected immunization related to pregnancy:
– hepatitis B vaccine – pregnancy and lactation are not contraindications for vaccination; vaccination is recommended from the second trimester of pregnancy
– flu vaccine (inactivated) – vaccination is recommended from the second trimester of pregnancy; during the epidemic, vaccinations should be applied regardless of the trimester; no adverse effects of the vaccine on the fetus have been observed; breastfeeding is also not a contraindication to vaccination
– tetanus and diphtheria vaccine – the vaccine is routinely recommended for pregnant women; a booster dose should be given to pregnant women who had the last vaccination at least 10 years ago; vaccination is recommended from the second trimester
– measles, rubella and mumps vaccine – the use of vaccines against these diseases is prohibited in pregnancy, especially against rubella; Pregnancy should be avoided for one month after vaccination
– varicella vaccine – pregnant women should not be vaccinated; a woman who is not pregnant should avoid becoming pregnant for at least one month from the date of vaccination and should avoid close contact with newly vaccinated persons
– pneumococcal vaccine – it is not recommended to vaccinate pregnant women
– meningococcal vaccine – vaccination is generally not recommended during pregnancy, but in the case of a clear risk of infection characterized by high mortality, pregnancy should not be a contraindication to vaccination
– rabies vaccine – if bitten by an animal suspected of rabies, pregnancy should not be a contraindication to vaccination
– hepatitis A vaccine – the probable risk of harm to the fetus after vaccination is assessed as low; however, no research; vaccinations only when there is a high risk of contracting hepatitis A in endemic areas
– vaccine against typhoid fever – vaccinations are not recommended during pregnancy and lactation
– yellow fever vaccine – used when traveling to certain countries in Africa and South America; in general, pregnant women should not travel to countries with a high risk of developing the disease; It is not recommended to use the vaccine during pregnancy and breastfeeding, and it should be administered only when it is necessary to travel to the areas at risk of yellow fever
– tick-borne encephalitis vaccine – not recommended for pregnant women except in high-risk areas
A few words of summary
In order to protect pregnant women and to protect the developing child in the womb, both non-pregnant women and their immediate family members should be encouraged to vaccinate.