Contents
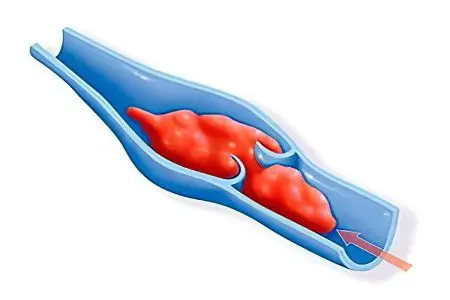
The portal vein is a large vessel that transports blood from the digestive organs to the liver to cleanse it of toxins. In the liver, a large vessel is divided into smaller veins, suitable for the hepatic lobules. In portal vein thrombosis, a blood clot blocks the vascular lumen, causing its complete or partial blockage (occlusion). The disease is localized in any part of the portal vein.
The age category of patients most susceptible to pathology is elderly patients, less often newborns. A separate category is pregnant women who have developed eclampsia in late gestation. A characteristic sign of eclampsia is blood clotting in all large vessels, including the portal vein.
Causes of
The reason for the formation of a blood clot in the portal vein is a violation of blood flow. In half of the cases, the pathology is based on a functional violation of the liver. Other causes may be associated with infectious and somatic disorders.
Causes of thrombus formation:
Hepatic alveococcosis;
Thromboembolism of the hepatic veins;
Cirrhosis;
Oncological damage to the liver;
Acute appendicitis (in children);
Infection of the stump of the umbilical cord in newborns;
Tumors of the abdominal cavity of any etiology;
Budd-Chiari syndrome – thrombosis of the veins of the liver;
Pancreonecrosis;
Operations on the digestive organs;
Consequences of removal of the spleen;
Pylephlebitis in history;
Ulcerative colitis;
Increased blood density;
Infection of the umbilical vein in the fetus;
Acute bacterial (constrictive) inflammation of the heart sac.
Classification of portal vein thrombosis
The disease is classified on several grounds.
By time of occurrence:
Acute thrombosis – the development of the pathological process occurs at lightning speed, within 5-7 minutes the patient dies due to necrosis of the digestive tract (liver, spleen, intestines, stomach, pancreas);
Chronic thrombosis – the blood flow in the vein does not stop immediately, because of the growing thrombus, it gradually decreases, while an alternative path of blood flow is formed, bypassing the clogged area.
Stages of development of thrombosis:
The localization of the thrombus is the transition of the portal vein to the splenic vein, the distribution area is less than 50% of the vascular system.
The localization of the thrombus is the area up to the mesenteric vessel.
The area of distribution in the third stage is all the veins of the peritoneum.
In the fourth stage, extensive circulatory disturbance occurs.
Portal vein thrombosis symptoms

This type of thrombosis has no specific symptoms inherent only to it. Manifestations of the disease may be similar to those of hepatitis, cancer or cirrhosis of the liver, gastritis, pancreatitis, colitis, enteritis. They depend on the localization of the blood clot that blocks the blood flow in various parts of the portal vein system.
Symptoms of stem thrombosis:
Pain in the left hypochondrium, in the epigastric region;
Pride;
Vomiting blood;
Peritonitis;
Expansion of the veins of the abdominal cavity;
Ascites, portal hypertension;
Jaundice;
Edema of the extremities;
Anemia.
Symptoms of radicular thrombosis of the mesenteric veins:
Increasing pain in the epigastrium;
Intestinal necrosis.
Symptoms of radicular thrombosis of the splenic vein:
The rapid onset of the disease;
Pain in the epigastrium, in the left hypochondrium;
Enlargement of the spleen;
Black stool with blood
Vomiting blood;
Ascites;
Venous bleeding from the esophagus and stomach.
Symptoms of terminal thrombosis:
Increase baked;
Ascites;
Expansion of the subcutaneous veins.
In chronic thrombosis, in 30% of cases, the disease cannot be diagnosed at the initial stage.
Diagnostics

Upon admission of the patient to the hospital, laboratory tests are carried out to confirm the diagnosis:
Complete blood count – reduced content of hemoglobin, erythrocytes, color indicator;
Coagulogram – reduced blood clotting time, increased prothrombin index;
Blood for biochemistry;
liver tests;
Lipidogram;
General urine analysis.
Instrumental research:
Computed tomography of the abdominal cavity (CT) – determines symptoms such as varicose veins of the portal vein system, localization of a blood clot, ascites, enlargement of the spleen.
Doppler ultrasound – determines the size and location of the thrombus, the speed of blood flow in the portal vein.
Angiography is an accurate method of monitoring the movement of a contrast agent through a vein using an X-ray machine. Determines the size of the thrombus, its localization, blood flow velocity.
Treatment of portal vein thrombosis
The goal of portal vein thrombosis treatment is to restore blood flow, minimize the consequences of vein blockage, and prevent relapses. Conservative and surgical treatment of pathology is used.
Conservative treatment is reduced to the use of such groups of drugs as: anticoagulants, plasma substitutes (replenishing the volume of blood flow after bleeding), thrombolytics, diuretics for ascites, glucocorticosteroids.
Operative therapy
With the ineffectiveness of drug therapy, as well as in acute conditions, surgical treatment is practiced.
Methods of surgical intervention:
Placement in the stomach of the Sengstein-Blackmore probe to force air and press the veins against the wall of the esophagus. Every 6 hours, the veins are freed from exposure to the probe to prevent bedsores. The use of the probe lasts for 48 hours.
Sclerosing injection therapy – the introduction of the drug Thrombovar into the veins for gluing varicose veins.
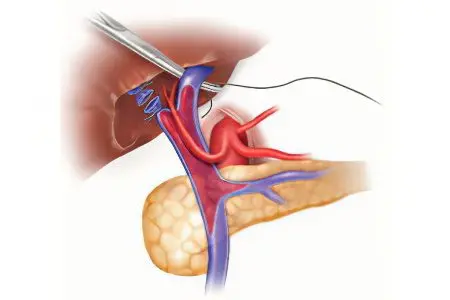
The imposition of a splenorenal anastomosis on a vein;
Prosthetics of a blocked vein;
Operation Tanner – stitching the stomach;
Opening and draining the inflamed parts of the vein to prevent the development of a vein abscess.
To prevent the disease, you need to forget about bad habits, strengthen the vascular system with dosed physical activity. You should eat right, if signs of malaise appear, consult a doctor.









