Contents
- Symptoms of polyps in the gallbladder
- Causes of polyps in the gallbladder
- What are polyps in the gallbladder?
- Diagnosis of polyps in the gallbladder
- Answers to popular questions
- What to do if polyps are found in the gallbladder?
- Treatment of polyps in the gallbladder without surgery
- Surgery for polyps in the gallbladder
- Diet for polyps in the gallbladder and after removal
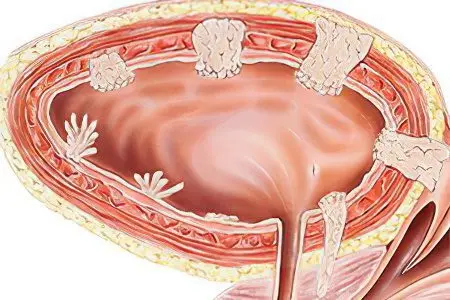
Polyps are growths of the surface epithelium of the gallbladder, can be single and large 1-2 cm, or form a network of small neoplasms 1-2 mm high. Polyps are benign in nature, but if they are present, the risk of oncological degeneration of cells and the development of gallbladder cancer increases.
The following figures reflect important information about polyposis and organ cancer:
Oncological diseases of the gallbladder are rare and range from 0,27 to 0,41% of all cancers.
Gallbladder cancer is twice as common among women as among male patients.
The risk of oncology increases with age, increases from the age of 45, and reaches its peak at 56-70 years.
Biliary tract operations can provoke the development of gallbladder cancer – it develops in 1-5% of all cases.
Among other oncological diseases of the digestive tract, gallbladder cancer is in fifth place after diseases such as cancer of the pancreas, stomach, intestines (rectum and colon)
Symptoms of polyps in the gallbladder
Any manifestations of the disease will depend on where the tumor is located. The most unfavorable situation is its growth on the neck of the bladder, or inside its duct. This creates a barrier to the path of bile to the intestines, which causes the patient to develop a disease such as obstructive jaundice. When polyposis growths are localized in other parts of the gallbladder, the patient does not experience any specific symptoms.
Nevertheless, its presence in the organ can be suspected by some indirect signs:
Pain. They appear in response to excessive stretching of the walls of the organ not by the polyp itself, but by bile, which stagnates through its fault. Such stagnant processes lead to the fact that multiple receptors located in the serous membrane of the organ are constantly irritated. In addition, pain can occur due to too frequent contraction of the walls of the gallbladder. The nature of the pain is dull and aching. They tend to give to the right hypochondrium, are present on a periodic basis. Provocateurs of pain can be alcohol-containing drinks, fatty foods and severe stress. That is why patients do not associate discomfort with polyps, attributing their occurrence to other factors, such as malnutrition.
Staining of the skin and mucous membranes in yellow. A similar symptom is the result of obstructive jaundice, which occurs when a bile duct polyp is clamped. Unable to exit naturally, bile begins to seep through the walls of the bladder and enter the bloodstream. The patient begins to experience itching, the integument becomes dry and tight, the urine darkens, vomiting of bile masses may begin and the temperature rises.
Renal colic. If the polyp has a very long stalk and is located in the area of the neck of the affected organ, then when it is twisted or clamped, hepatic colic may develop. Most often this occurs with a pronounced contraction of the organ. When torsion occurs, a person experiences sudden pain, which has a sharp cramping character, the heartbeat rises, blood pressure rises. At the same time, the patient cannot choose for himself a more or less comfortable position in order to somewhat calm the discomfort. It is the last sign that is a clear indicator of hepatic colic.
Dyspeptic symptoms. The presence of a polyp is most often indicated by dyspeptic symptoms. Its severity varies. Typical manifestations are: bitter taste, morning sickness, vomiting after overeating. All these manifestations are explained by periodic or constant congestion occurring in the organ. In addition, due to the polyp, there is a violation of the production of bile. Its deficiency negatively affects the digestion process, so the patient can begin to quickly lose weight.
However, all of the above symptoms rarely force the patient to go to medical institutions, and even more so to undergo an ultrasound examination, during which existing tumors can be detected.
Causes of polyps in the gallbladder
There are four reasons why polyposis growths in the gallbladder may presumably begin to develop:
Factor of heredity and anomalies of genetic development. Thus, heredity influences the growth and development of polyposis growths. Most often, adenomatous formations and papillomas are inherited. It has been established that even if other tumors are detected in close relatives, the risks of developing gallbladder polyps increase. In addition, a genetic predisposition to bile duct dyskinesia is a direct cause leading to the development of polyposis. However, it cannot be said that only genetic predisposition is the cause of tumor formation. It grows and develops under the influence of other factors. A burdened family history in this case is an additional provocateur for the manifestation of the disease.
Diseases of the gallbladder of inflammatory origin. Chronic cholecystitis is the most common reason for the development and growth of a polyp. In the organ against the background of cholecystitis, stagnation of bile occurs, its wall thickens and undergoes deformation. The granulation tissue of the bladder begins to respond to the inflammatory process. This reaction manifests itself in the form of proliferation of its cells. As a result, pseudo-polyps of inflammatory origin are formed in a person.
Failures of metabolic processes. The most common cause of the growth of cholesterol pseudopolyps are lipid metabolism disorders. As a result, a significant amount of cholesterol begins to circulate in the bloodstream. Its excess gradually begins to be deposited on the walls of blood vessels, as well as in the organ – the storehouse of bile. This leads to the formation of pseudopolyps consisting of cholesterol. In addition, such formations can appear even against the background of a normal concentration of lipids in the blood, which is due to the cholesterol that is part of bile. When conducting an ultrasound examination, it is precisely such pseudopolyps that are most often found. The longer a person is their carrier, the more they become. Their growth is facilitated by the absence of any symptoms that disturb a person.
Diseases of the hepatobiliary system. Any diseases of the biliary tract contribute to an imbalance between the optimal amount of bile necessary for digestion and its volumes allocated for this process. Both its deficiency and excess disrupt the process of digestion of food. This leads to various pathologies of the gastrointestinal tract, including provoking the development of polyps.
Concomitant diseases in gallbladder polyps
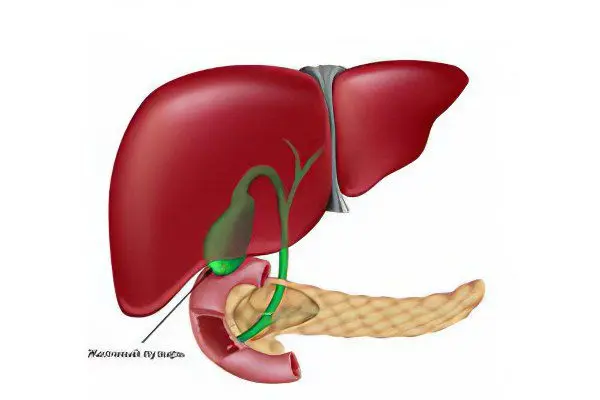
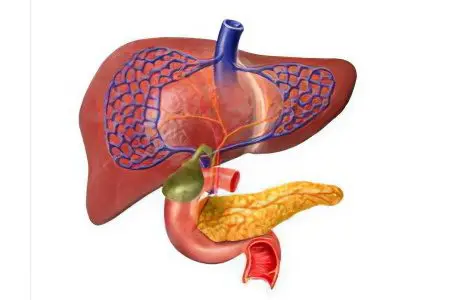
Polyps of the gallbladder can provoke pathologies in the organs closest to it – the liver and pancreas. So, polyps are a potential focus for the development of infection, which give rise to the inflammatory process. This provokes cholecystitis, spasms of the biliary tract, pancreatitis and other diseases. In addition, inflammatory processes in the gallbladder themselves can contribute to the pathological growth of its mucosa.
What diseases are observed in gallbladder polyps?
Dyskinesia or spasms of the gallbladder duct. Dyskinesia, which is hypertonic in nature, in which the tone of the gallbladder increases, is more common in women and is usually closely associated with the menstrual cycle. Hypotonic dyskinesia (insufficient intensity of contractions of the gallbladder) is common among middle-aged or older people. Dyskinesia leads to difficulty in the outflow of bile, which in a chronic course can provoke cholecystitis or the deposition of stones in the gallbladder, and in addition, creates conditions for the formation of polyps. Also, the disease can be caused by dysfunction of the sphincter of Oddi, which separates the bile ducts from the duodenum.
Cholelithiasis – the formation of cholesterol stones in the liver, bile ducts or gallbladder, due to lipid metabolism disorders. The formation of cholesterol stones in the gallbladder begins with a violation of the chemical composition of bile – it lacks bile acids and phospholipids, but there is a glut of cholesterol and fatty acids. The causes of this disease can be obesity, an unbalanced diet, bile stasis, infections of the gallbladder and biliary tract. At the same time, cholesterol polyps of the gallbladder and other neoplasms of its mucosa can be observed.
Acute and chronic pancreatitis – an inflammatory disease of the pancreas, which in 65-60% of cases is observed with dyskinesia, spasms or dysfunction of the sphincter of Oddi, hepatic colic and cholelithiasis. Other causes of pancreatitis are the spread of the inflammatory process caused by infection from the gallbladder and its duct to the pancreas, the abuse of alcohol and food that causes increased pancreatic secretion.
Acute or chronic cholecystitis – inflammation of the gallbladder, which in 90% of cases is observed in the presence of stones and cholesterol deposits, as well as when they are displaced and enter the biliary tract. In addition to cholelithiasis, cholecystitis can be associated with infectious diseases, parasitic invasion, neoplasms in the gallbladder.
What are polyps in the gallbladder?
Cholesterol polyps – tumor-like formations, which consist of cholesterol deposits with calcified inclusions, develop first under the gallbladder mucosa, after which it grows, forming a polyp. They are usually observed in people with impaired fat metabolism with an increased level of low-density lipoprotein and a decrease in the concentration of HDL (high-density lipoprotein). They are quite common, they are discovered by chance during the examination, since their formation and growth are asymptomatic.
Inflammatory polyps – the cause of their formation is the inflammatory process, which can develop as a result of a bacterial infection. On the inner membrane of the gallbladder, an overgrowth of granulomatous tissues in the form of a tumor is formed.
Adenomatous polyps – true tumors, benign, but with an increased risk of malignant degeneration. The cause of adenomatous polyps and papillomas is the growth of glandular tissue, in 10% of cases they degenerate into oncological formations, which causes concern among doctors and requires constant monitoring of their growth and immediate treatment.
Papillomas – also benign tumors, usually small in size and characteristic papillary growths.
Diagnosis of polyps in the gallbladder
The detection of pathological growths in the gallbladder has become possible due to the development of radiology since the thirties of the twentieth century. Since then, modern medicine has taken several steps forward in this regard, and more accurate and harmless diagnostic methods are available to patients.
In most medical institutions, ultrasound and endoscopic ultrasonography are used to diagnose polyps:
US allows you to detect single or multiple polyps of the gallbladder mucosa. They appear on the screen of the apparatus as rounded formations associated with the walls of the bubble without an acoustic shadow. When changing the position of the patient’s body, the polyps do not move.
Ultrasonography consists in the study of the duodenum and gallbladder using a flexible endoscope. The device is swallowed by the patient, at its end there is an ultrasonic sensor, with the help of which the walls of the gallbladder are examined for the presence of growths. An important role in the detection of various details is played by the operating frequency of the sensor – the higher it is, the more detailed the resulting image. This method allows you to get a better image, respectively, and the diagnostic data is more accurate.
In addition, a CT scan called magnetic resonance cholangiography is available in some hospitals. This is the most progressive method at the moment, thanks to which the doctor can not only see, localize and evaluate the size of the neoplasm, but also identify the presence of concomitant formations that occur during the malignancy of the polyp. To assess the amount of contrast agent accumulated by tumor tissues, multislice computed tomography may be additionally prescribed.
Due to the breadth of application of modern diagnostic methods, statistics of cases of gallbladder polyps was compiled, which showed that approximately 4% of the population are their permanent carriers, of which the predominant part (60%) are women aged 30 years and above.
Answers to popular questions
Can a polyp in the gallbladder dissolve? In 95% of cases, the detected polyps are loose cholesterol formations, which makes their conservative treatment with choleretic drugs, which include ursosan and ursofalk, possible. Medicines that thin bile promote the resorption of polyps in the submucosal layer of the gallbladder.
Is it possible to remove only the polyps themselves while maintaining a functioning gallbladder? It is impossible to remove a polyp without damaging the walls of the gallbladder, so even if the doctor saves the organ, its function will be impaired, and polyps will reappear after a while, possibly in greater numbers than before the operation. This practice has been abandoned for a long time. Already in the 70s of the last century, they stopped performing operations that preserve the gallbladder after the removal of neoplasms from it. In addition, at one time there was a popular method of crushing stones (lithotripsy). However, this treatment technique turned out to be meaningless, since after a while 99% of patients had a relapse of the disease. In the future, they were helped only by surgical intervention with the removal of the organ. Therefore, the optimal method of treatment is surgery, namely, laparoscopic cholecystectomy.
However, removal of the gallbladder is not the only way out; most neoplasms are amenable to conservative treatment. The patient is required to regularly undergo diagnostics twice a year to prevent the malignancy of polyps and the onset of the cancer process. The danger is growths greater than 10 mm, which do not stop growing; if a small polyp has increased in a year and has become twice its original size, this may indicate the onset of malignancy. Neoplasms with a wide base that do not have a pronounced pedicle are more prone to malignant degeneration. With polyps larger than a centimeter, an operation is prescribed to remove the gall. In other cases, you can get by with choleretic drugs and correction of diet and lifestyle.
Can a polyp in the gallbladder hurt? Pain in gallbladder polyps is usually associated with the formation of cholesterol stones or are symptoms of cholecystitis. Usually polyps in the gallbladder do not cause pain.
Is it possible to visit a bath or sauna with polyps in the gallbladder? With polyps in the gallbladder, it is impossible to warm up the area of uXNUMXbuXNUMXbthe organ, therefore it is not recommended to go to the bath or sauna, spend a lot of time in the sun.
What to do if polyps are found in the gallbladder?

The treatment is carried out with chenodeoxycholic and ursodeoxycholic acid, which stimulate the mechanism of bile formation and improve the quality of bile, which contributes to the dissolution of cholesterol stones. A three-month course of treatment is prescribed, the dosage is calculated at 10 mg per 1 kg of the patient’s weight, taken in the evenings two hours after the last meal. Treatment with bile acids is combined with a diet according to table No. 5
After the end of the course of treatment, a control ultrasound is performed and conclusions are drawn about the need for surgery. If the growth of formations slows down, their number or size decreases, then conservative methods of treatment are effective in this case.
Treatment of polyps in the gallbladder without surgery
First of all, you need to contact a gastroenterologist and conduct all the necessary diagnostic examinations in order to determine the type of polyps, their size and the risk of malignancy.
Cholesterol polyps are the most common type of neoplasm in the gallbladder, with timely treatment they do not pose a great danger.
Cholesterol polyps occur as a network of small inclusions of 1-2 mm, diffusely distributed along the inner wall of the organ, or they can be up to 4 mm in size and look like outgrowths with even contours and a wide base on ultrasonography. Polyps larger than 4 mm already have a thin stalk.
Most often, the doctor prescribes ursodeoxycholic acid, which promotes the destruction of deposits, consisting of cholesterol, reduces the level of lipoproteins in the blood, and has a choleretic effect.
Multiple cholesterol polyposis may actually be not growths, but loose cholesterol stones, which subsequently cause pain in the patient. Common complaints in this case are sensations of heartburn, nausea and pain in the right hypochondrium, symptoms of cholecystitis caused by cholesterol stones.
Treatment of cholesterol polyps can be carried out conservatively if the growth height is not more than 10 mm.
A surgical operation to remove polyps or the entire gallbladder is prescribed only as a last resort, if there are many neoplasms and they are constantly growing. In most cases, doctors try to save the organ, since its absence can provoke digestive disorders and make it difficult to digest fatty foods.
Surgery for polyps in the gallbladder
The oncologically tense situation of our time requires careful control over any neoplasms in the body, otherwise there is a risk of oncological tissue degeneration. If a course of conservative treatment did not work, or large polyps were found during the first diagnosis, an operation is indicated.
Indications for surgical treatment of polyps:
High growth rate of polyps – from two mm per year;
The size of the neoplasm is from 10 mm;
A large number of growths with a wide base without a leg.
If the size of the polyps is less than 1 mm, surgery is not needed, but a preventive examination is necessary monthly for six months, and then every three months. If the neoplasms do not increase in size, then further diagnostics are carried out every six months.
Types of operations on the gallbladder:
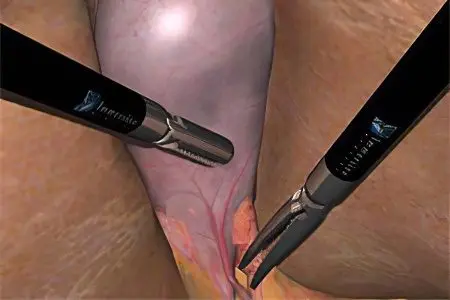
Videolaparoscopic cholecystectomy (LCE) – is considered the most gentle for the patient, uses modern endoscopy technologies.
Laparoscopic cholecystectomy – removal of the gallbladder without an incision, as in traditional cholecystectomy using instruments for endoscopic operations. It is considered the “gold standard” of modern surgery, but in five percent of cases the operation cannot be completed and a traditional cholecystectomy is performed.
Conventional cholecystectomy (TCE) – by open surgery, access is made through the upper midline or Kocher incision in the right hypochondrium. The disadvantage of this method, in comparison with laparoscopic cholecystectomy, is its invasiveness – the incision cuts through the skin, fatty tissue, white line of the abdomen and peritoneum.
Endoscopic polypectomy – used to remove polyps of the gallbladder while preserving the organ. This type of operation is performed using a diathermic loop, which is thrown over the leg of the polyp and cut off. Formations without a stem are removed by fragmentation. An electric charge is passed through the loop in order to coagulate the vessels, which helps to avoid bleeding. This method is used to remove polyps in the intestines, but it is rarely used in the treatment of gallbladder polyposis, so the consequences can be unpredictable.
Preparation for cholecystectomy
Before the operation, the patient must undergo a comprehensive diagnostic examination in order to avoid possible complications and choose the optimal method of cholecystectomy.
What diagnostic procedures should be carried out before the operation:
Ultrasound examination of the liver, gallbladder and pancreas, which allows you to identify concomitant diseases and inflammatory processes, evaluate the number of polyps, their size and type, determine the presence of stones in the liver and gallbladder;
Computed tomography allows you to assess the state of the tissues surrounding the gallbladder, determine the state of its mucosa, the presence of adhesions and scars, examine the state of its wall for thickening and nodular formations;
MRI – one of the most reliable methods for the study of polyps and stones in the gallbladder, which allows timely detection of adhesions, inflammation, pathology of the biliary tract;
Laboratory studies of bile for the presence of blood cells, calcium bilirubinate, cholesterol, epithelial cells, assessment of its rheological properties. Calcium bilirubinate found in the duodenal contents may indicate calcareous deposits in the gallbladder, the presence of epithelial cells in bile may be a sign of inflammatory processes. It is also necessary to examine the bile for the presence of protozoan parasites – lamblia.
Diagnosis of the state of the cardiovascular and respiratory systems using radiography and ECG allows you to correctly prescribe a treatment regimen; heart failure is a serious contraindication for some cholecystectomy methods.
Preparatory procedures necessary for the patient immediately before the operation:
Eliminate blood-thinning foods from the diet, stop taking medications that affect blood clotting, such as aspirin – this is necessary to minimize the risk of bleeding during surgery.
On the day of the operation, do not eat and drink liquids, even water is excluded.
The night before the operation, it is necessary to cleanse the intestines using an enema or laxative;
Immediately before the operation, thoroughly cleanse the body using antibacterial soap.
Can you live without a gallbladder?
All human organs can be conditionally divided into vital (like the brain, heart, liver, etc.) and organs without which life is possible, but the functionality of some systems will be impaired. These organs include the spleen, gallbladder, appendix, and stomach. Despite the fact that a person can easily live without these organs, subject to a strict diet and limiting stress on the body, it is not recommended to remove them without a compelling need.
Removal of the gallbladder is carried out only if its pathology threatens the entire body as a whole. Thus, a large number of polyps with an accelerated growth rate and an increased risk of malignancy can lead to gallbladder cancer with metastases to other internal organs. In this case, removal of the gallbladder or cholecystectomy is a matter of life and death. This is an absolute indication for surgery.
Rules of conduct after removal of the gallbladder
After the operation, the patient will have to slightly change the way of eating. The fact is that, thanks to the gallbladder, bile accumulates in the liver, and its concentration increases. In the absence of this organ, the digestive juice is sent directly to the intestines, and its concentration remains quite low. Removal of the gallbladder also affects the activity of enzymes – it is significantly reduced. It takes about two years for the body to fully adapt to a new way of digestion without the help of a remote organ.
For the first six months after the operation, it is necessary to strictly monitor the diet:
The first rule – You can eat only boiled or steamed food.
The second rule – Eat food in small pieces, chewing it slowly and thoroughly. This will give the liver time to activate all the necessary enzymes and start working.
Third rule – reduce the amount of food consumed at a time, but increase the number of servings. Otherwise, the digestive system will not have time to cope with its functions, and nausea and heaviness in the intestines will appear. Another negative consequence of violating this rule is stagnation of bile, which can occur in the ducts even after removal of the bladder.
After six months of strict abstinence, fresh vegetables and fruits, as well as dietary meat and fish, can be included in the diet. Although excessively acidic, spicy and essential oil-rich foods (onions, garlic, radishes, lemons, sour berries, pineapples, etc.) must be abandoned for another 12-18 months.
Two years after the removal of the gallbladder, the digestive system becomes strong enough for the patient to be able to return to his usual diet, excluding refractory fats (heavy meat and lard), although the second and third rules are best adhered to for life.
Physical activity after gallbladder surgery
After two to three months of the postoperative period, the patient is strongly recommended to take regular walks, taking at least half an hour a day. This is the very first and affordable way to avoid bile stasis.
Six months later, the patient can sign up for a pool or go swimming in the warm season on their own – regular soft massage with water almost completely eliminates the risk of stagnation.
At the same time, morning exercises are allowed, but this does not apply to the abdominal muscles. Significant tension of the muscular corset is recognized by doctors as safe only a year after the operation.
The problem with the microflora after cholecystectomy
A decrease in the concentration of bile also affects the microflora of the small intestine – microbes get the opportunity to multiply more intensively and provoke attacks of diarrhea, flatulence and constipation. To stop the reproduction of opportunistic and pathogenic microflora, change the nature of the diet (exclude sweets from the diet), maintain beneficial microflora by regularly taking prebiotics and food with bifidus and lactobacilli. To solve this problem, you can also contact a gastroenterologist for advice on the selection of drugs that destroy intestinal microbes without harm to the body.
Diet for polyps in the gallbladder and after removal

In diseases associated with insufficiency of the liver and gallbladder, the doctor must prescribe dietary table No. 5 or report on its basic requirements without specifying the diet, for example, simply says: “no fried, spicy, smoked, pickled”, etc. In any case, a patient with polyps in the gallbladder needs to know how to maintain his health by protecting himself from foods that are difficult for the liver.
Diet #5 consists of foods that provide a complete daily serving of protein, carbohydrates, and calories while limiting fat intake. When eating certain types of food, the patient’s condition may worsen, which is why they should be excluded from the diet. The consumption of food that unnecessarily stimulates the pancreas and the secretion of the stomach itself is also limited.
The ultimate goal of the diet is not only to reduce the chemical load on the liver, but also to speed up the excretion of cholesterol, due to the improvement of intestinal motility and the choleretic properties of food components. The diet should be followed so that the optimal daily calorie intake is maintained (for an adult – from 2200 to 2600 kilocalories, depending on the severity of physical labor performed regularly). In addition to the calorie content of food, the amount of food is extremely important, since even light and liquid foods taken in large portions can overload the gallbladder.
If polyps are found in the gallbladder, which often occurs by chance during a comprehensive examination, it is not necessary to consult a doctor in the first stages of the disease. The patient can adhere to this diet on his own, so as not to bring the disease to the need for surgical intervention and increase the effectiveness of conservative treatment.
What can you eat?
Flour – bread black and white, only yesterday’s baking or dried to crackers. It is permissible from time to time to pamper yourself with dry cookies or biscuits. No more than twice a week it is allowed to use well-baked buns or pies without butter in the dough;
Meat is just lean. If it is beef, then boiled, you can also eat tongue and ham. If the bird is dietary (chicken, turkey), only fillets (breasts) are desirable, but other meaty parts are also allowed to be boiled. Fish must be steamed or boiled, caviar and milk can be added only in small quantities as a flavor enhancer. When possible, boiled meat and fish can be additionally baked to improve the taste.
soft-boil eggs, consume no more than one per day. It is best to cook an omelet from it. If the omelette is large, it is necessary to divide it into parts and eat so that you get only one egg per day (for example, divide a dish of four eggs into four parts and do not eat more than one per day);
Vegetables with herbs can be eaten both raw and boiled. It is useful to use vegetables as side dishes and full meals, especially if it is beets and carrots;
Cereals, boiled in water or with milk, as well as pasta;
Fruits and berries – only sweet and preferably as part of jelly or compote, sour fruits are excluded from the diet. Baking and steaming fruits is not prohibited;
Dairy products can be eaten no more than 200 g per day. It can be low-fat raw foods (cottage cheese, kefir, milk, yogurt, mild cheese). It is also allowed to cook casseroles, dumplings, soufflés, cheesecakes, processed cheese from them.
Vegetable oil – no more than two tablespoons per day, use only as a dressing for vegetable salads and other prepared dishes.
Among sweets, you should choose natural honey, jam, marshmallows, marmalade, but not more than 70 g per day;
Sauces based on milk, berries and fruits;
Drinks: rosehip infusion, herbal preparations with a choleretic effect;
Among spices, give preference to greens (dill, parsley, basil), bay leaf, cinnamon and cloves.
Food is divided into small portions, the number of meals daily is at least five. You can not eat cold or very hot food, this can provoke irritation of the intestinal mucosa. Drink at least 1,5 liters of fluid daily, drink before each meal, this contributes to the release of bile, preventing its accumulation and stagnation. Minimize the amount of salt consumed. Food, if possible, should be crushed before eating.
What shouldn’t be eaten?
Under the ban are refractory fats and products containing them – lard, lamb, pork; a small amount of butter in the diet is acceptable;
Smoked meats, spicy, pickled, canned food;
Among greens and vegetables – exclude spinach, onions, garlic, turnips, radishes and sorrel from the diet;
All legumes;
Among dairy products, sour cream is prohibited;
Butter baking;
Chocolate, cocoa and ice cream;
Any carbonated drinks;
Vinegar, spices and spices;
Restriction of salt intake – no more than 10 g per day;
Any alcohol.









